HIV and Transgender People: Viral Suppression
Viral suppression is one of the six Ending the HIV Epidemic in the U.S. indicators. Viral suppression refers to the percentage of people with diagnosed HIV who have less than 200 copies of HIV per milliliter of blood.
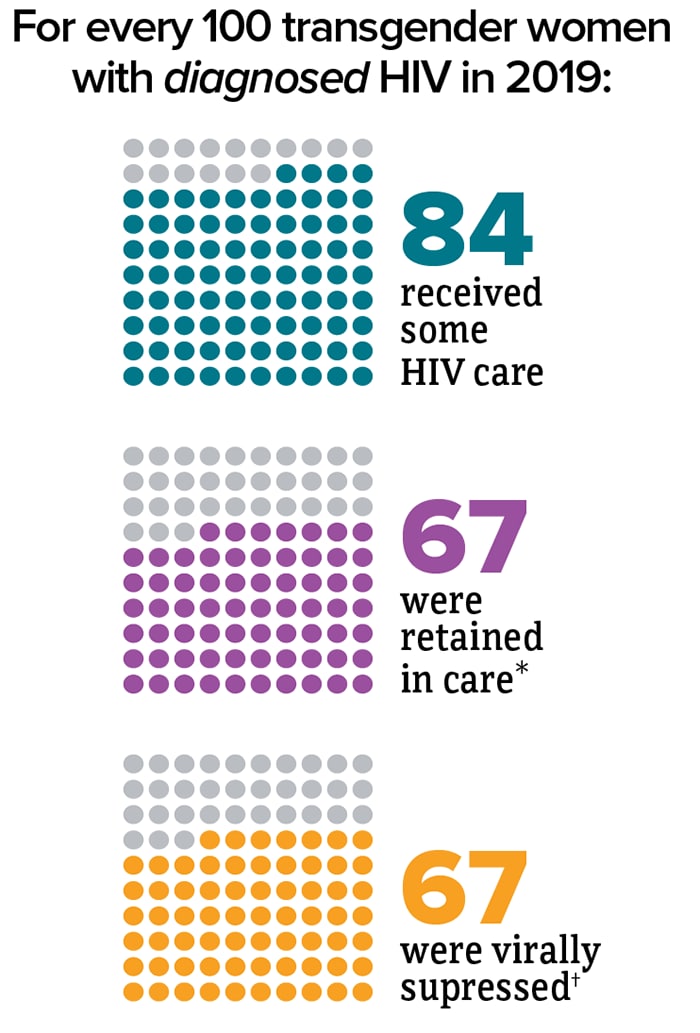
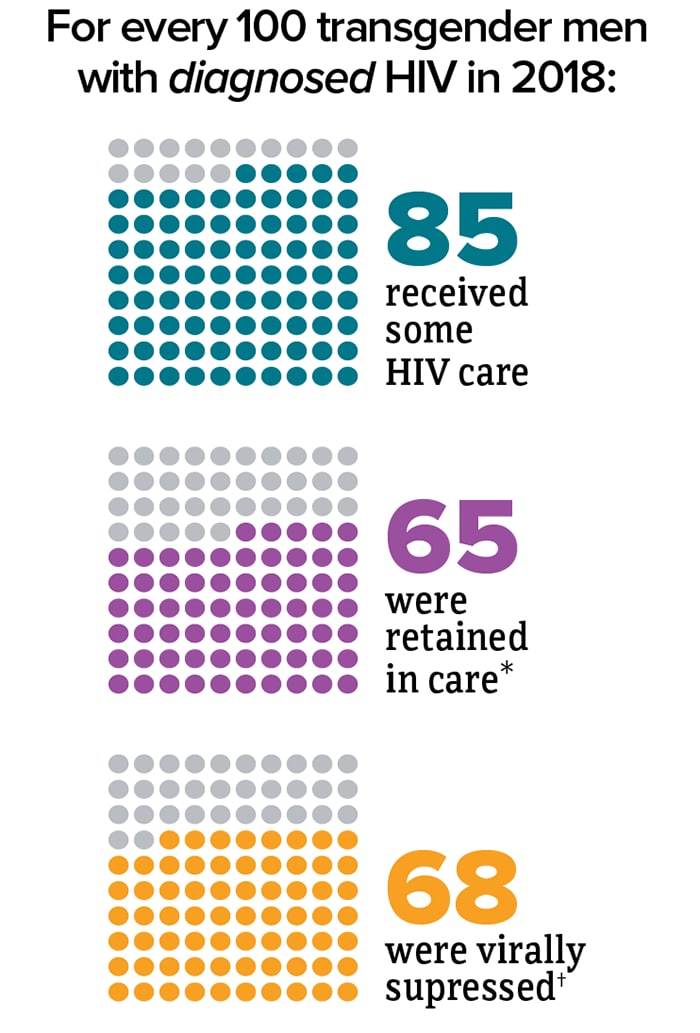

* Had 2 viral load or CD4 tests at least 3 months apart in a year.
† Had less than 200 copies of HIV per milliliter of blood on most recent viral load test.
Source: CDC. Monitoring selected national HIV prevention and care objectives by using HIV surveillance data—United States and 6 Dependent Areas, 2019. HIV Surveillance Special Report 2021; 26(2).
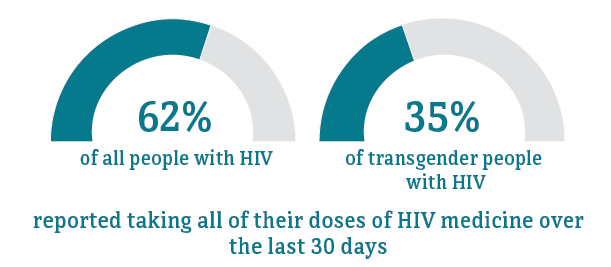
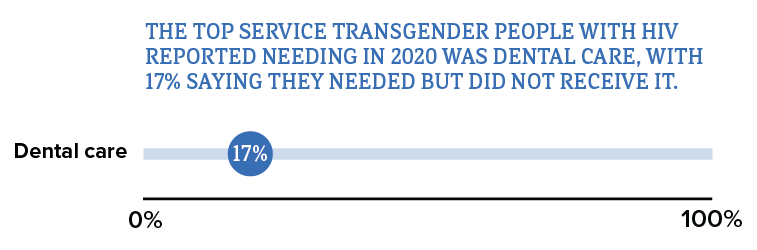
Although many people taking HIV medicine are virally suppressed, some people with HIV who are taking HIV medicine are currently not virally suppressed or do not maintain viral suppression over time. Some challenges with achieving and maintaining viral suppression include missing multiple doses of HIV treatment, missing medical appointments, or needing other important health care services.
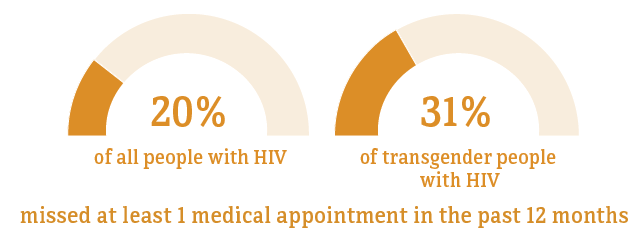
* Among people aged 18 and older.
Source: CDC. Medical Monitoring Project.
* Among people aged 18 and older.
Source: CDC. Medical Monitoring Project.


* Among people aged 18 and older.
† HIV ancillary services, such as case management and mental health services, are services that support retention in HIV care and viral suppression.
Source: CDC. Medical Monitoring Project.
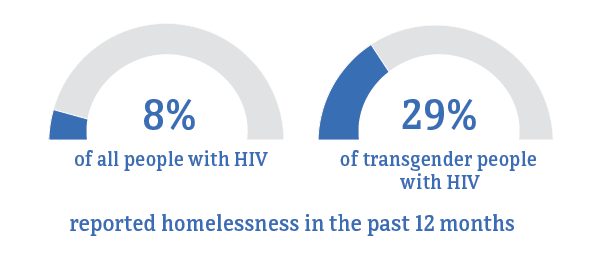
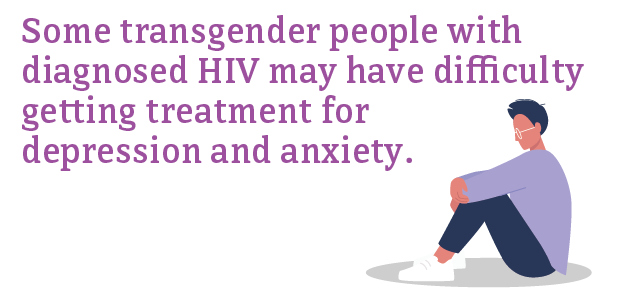
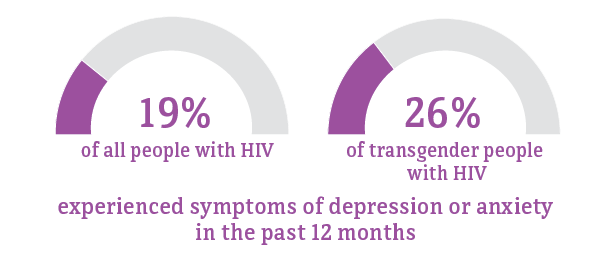
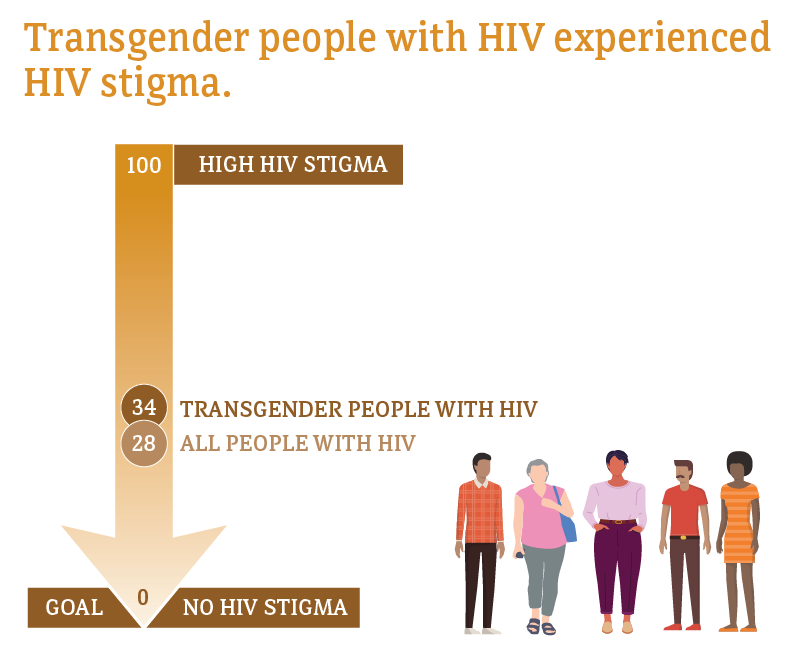
Social and economic issues—such as homelessness, depression, and stigma—have prevented some transgender people from getting the HIV care and treatment they need. These factors make it difficult for some transgender people with HIV to achieve and maintain viral suppression.

* Among people aged 18 and older.
Source: CDC. Medical Monitoring Project.
* Among people aged 18 and older.
Source: CDC. Medical Monitoring Project.
* Among people aged 18 and older.
Median HIV stigma scores are presented based on a ten-item scale ranging from 0 (no stigma) to 100 (high stigma) that measures personalized stigma during the past 12 months, current disclosure concerns, current negative self-image, and current perceived public attitudes about people with HIV.
Source: CDC. Medical Monitoring Project.
- CDC. HIV infection, risk, prevention, and testing behaviors among transgender women–National HIV Behavioral Surveillance–7 U.S. Cities, 2019-2020 [PDF - 2 MB]. HIV Surveillance Special Report 2021.
- CDC. Monitoring selected national HIV prevention and care objectives by using HIV surveillance data—United States and 6 Dependent Areas, 2019. HIV Surveillance Special Report 2021.
- CDC. Behavioral and clinical characteristics of persons with diagnosed HIV infection—Medical Monitoring Project, United States, 2018 cycle (June 2018–May 2019) [PDF - 905 KB]. HIV Surveillance Special Report 2020;25.
- CDC. Selected national HIV prevention and care outcomes [PDF - 2 MB] (slides).
- Becasen JS, Denard CL, Mullins MM, Higa DH, Sipe TA. Estimating the prevalence of HIV and sexual behaviors among the US transgender population: a systematic review and meta-analysis, 2006–2017. Am J Public Health 2018. e1-e8. PubMed abstract.
- Baral SD, Poteat T, Strömdahl S, Wirtz AL, Guadamuz TE, Beyrer C. Worldwide burden of HIV in transgender women: a systematic review and meta-analysis. Lancet Infect Dis 2013;13(3):214-22. PubMed abstract.
- Brennan J, Kuhns LM, Johnson AK, Belzer M, Wilson EC, Garofalo R, et al. Syndemic theory and HIV-related risk among young transgender women: the role of multiple, co-occurring health problems and social marginalization. Am J Public Health 2012;102(9):1751-7. PubMed abstract.
- Herman JL, Flores AR, Brown TNT, Wilson BDM, Conron KJ (2017). Age of individuals who identify as transgender in the United States. Los Angeles, CA: The Williams Institute.
- CDC. CDC-funded HIV testing: United States, Puerto Rico, and U.S. Virgin Islands, 2015 [PDF - 2 MB]. July 2017.
- Chen S, McFarland W, Thompson HM, Raymond HF. Transmen in San Francisco: what do we know from HIV test site data?AIDS Behav 2011;15:659-62. PubMed abstract.
- Clark H, Babu AS, Wiewel EW, Opoku J, Crepaz N. Diagnosed HIV infection in transgender adults and Adolescents: Results from the National HIV Surveillance System, 2009-2014. PubMed abstract.
- De Santis JP. HIV infection risk factors among male-to-female transgender persons: a review of the literature. J Assoc Nurses AIDS Care 2009;20(5):362-72. PubMed abstract.
- Flores AR, Herman JL, Gates GJ, Brown TNT. How many adults identify as transgender in the United States? Los Angeles, CA: The Williams Institute. June 2016.
- Garofalo R, Johnson AK, Kuhns LM, Cotton C, Joseph H, Margolis A. Life Skills: evaluation of a theory-driven behavioral HIV prevention intervention for young transgender women. J Urban Health 2012;89(3):419-31. PubMed abstract.
- Herbst JH, Jacobs ED, Finlayson TJ, McKleroy VS, Neumann MS, Crepaz N. Estimating HIV prevalence and risk behaviors of transgender persons in the United States: a systematic review. AIDS Behav 2008;12(1):1-17. PubMed abstract.
- Hotton AL, Garofalo R, Kuhns LM, Johnson AK. Substance use as a mediator of the relationship between life stress and sexual risk among young transgender women. AIDS Educ Prev 2013;25(1):62-71. PubMed abstract.
- James SE, Herman JL, Rankin S, Keisling M, Mottet L, Anafi M. The Report of the 2015 U.S. Transgender Survey. Washington, DC: National Center for Transgender Equality; 2016.
- Meerwijk EL, Sevelius JM. Transgender population size in the United States: a meta-regression of population-based probability samples. Am J Public Health 2017; 107(2):e1-e8. PubMed abstract.
- Mizuno Y, Frazier EL, Huang P, Skarbinski J. Characteristics of transgender women living with HIV receiving medical care in the United States LGBT Health 2015;2(00):1-7. PubMed abstract.
- New York City Department of Health and Mental Hygiene. Surveillance slide sets: HIV among people identified as transgender in New York City, 2015-2019. December 2020. Accessed March 22, 2021.
- Nuttbrock L, Hwahng S, Bockting W, Rosenblum, A, Mason, M, Macri M, et al. Lifetime risk factors for HIV/sexually transmitted infections among male-to-female transgender persons. J Acquir Immun Def Syndr 2009;52(3):417–21. PubMed abstract.
- Reisner SL, Perkovich B, Mimiaga MJ. A mixed methods study of the sexual health needs of New England transmen who have sex with nontransgender men. AIDS Patient Care STDS 2010;24(8):501-13. PubMed abstract.
- Rowniak S, Chesla C, Rose CD, Holzemer WL. Transmen: the HIV risk of gay identity. AIDS Educ Prev 2011;23(6):508-20. PubMed abstract.
- Sanchez T, Finlayson T, Murrill C, Guilin V, Dean L. Risk behaviors and psychosocial stressors in the New York City House Ball community: a comparison of men and transgender women who have sex with men. AIDS Behav 2010;14:351-8. PubMed abstract.
- CDC. HIV testing among transgender women and men — 27 states and Guam, 2014–2015. MMWR 2017;66:883–887.
- Lemons A, Beer L, Finlayson T, Hubbard McCree D, Lentine D, Shouse RL. Characteristics of HIV-positive transgender men receiving medical care: United States, 2009–2014. Am J Public Health 2018;108(1):128-30. PubMed abstract.
- Reisner SL, Jadwin-Cakmak L, White Hughto JM, Martinez M, Salomon L, Harper GW. Characterizing the HIV prevention and care continua in a sample of transgender youth in the U.S. AIDS Behav. 2017; 21(12):3312-3327. PubMed abstract.
- Poteat T, Malik M, Scheim A, Elliott A. HIV prevention among transgender populations: knowledge gaps and evidence for action. Curr HIV/AIDS Rep. 2017;14(4):141-152. PubMed abstract.
- Mizuno Y, Frazier EL, Huang P, Skarbinski J. Characteristics of transgender women living with HIV receiving medical care in the United States. LGBT Health. 2015;2(3):228-34. PubMed abstract.
- National Center for Transgender Equality; Annual report 2016. The T’s Not Silent.