Ending the HIV Epidemic

Overview
We can end the HIV epidemic in the US. Immediate, effective treatment is key. Taking HIV medicine as prescribed can make the amount of virus in the body very low (called viral suppression* or undetectable). People with HIV who stay undetectable can stay healthy and have effectively no risk of sexually transmitting HIV.
To reduce new infections:
- Early HIV diagnosis is crucial. Everyone aged 13-64 should be tested at least once. People at high risk should be tested at least annually. Sexually active gay and bisexual men may benefit from more frequent testing (e.g., every 3-6 months).
- People with HIV should take HIV treatment as soon as possible. People who stay in lifetime treatment can live longer, prevent complications from HIV, and prevent transmission through sex.
- Prevention tools like condoms and pre-exposure prophylaxis (PrEP) can protect people who are at risk for HIV.
* Less than 200 copies of HIV per milliliter of blood
HIV Treatment Can Prevent Transmission
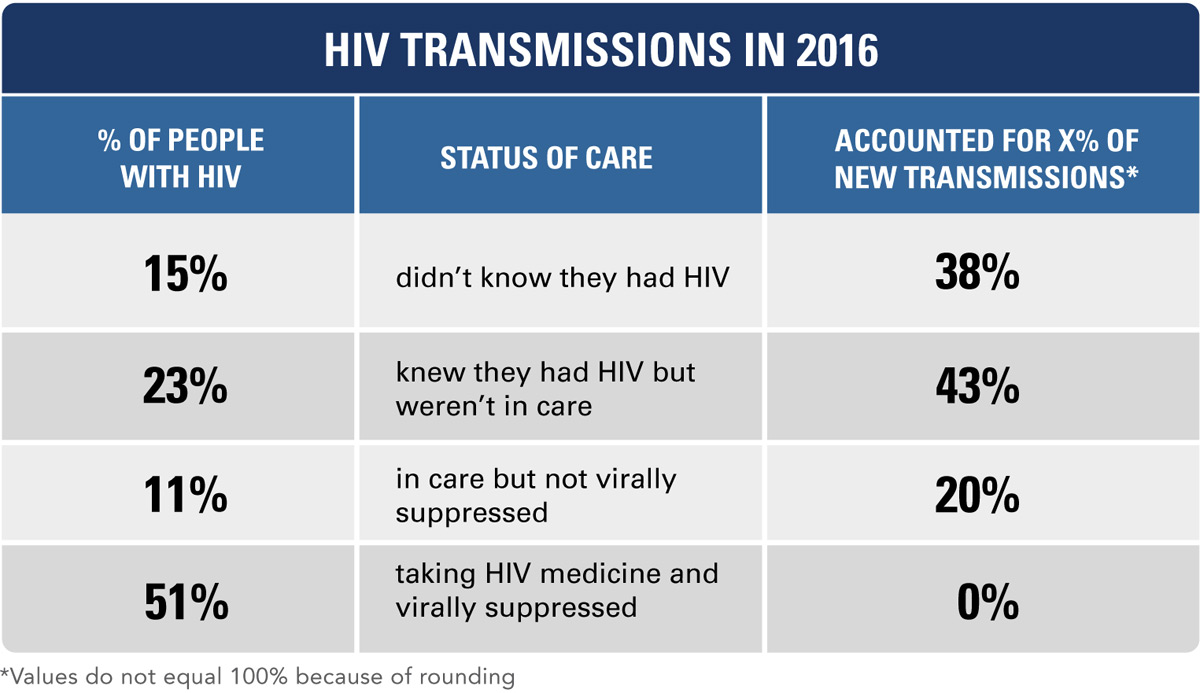
View Text Description
SOURCE: Vital Signs, 2019
Many people with HIV aren’t getting the treatment they need.
About half of people with HIV are virally suppressed or undetectable.
- There are nearly 40,000 new HIV infections a year.
- New HIV infections come from people who aren’t virally suppressed or undetectable.
- Nearly 40% of people with HIV don’t know they have it or know but aren’t in care.
Healthcare Providers Can:
- Test patients for HIV. Quickly link people with HIV to care and help them stay in care.
- Discuss prevention with patients who may benefit from condoms and PrEP.
People with HIV Can:
- Start HIV care now, stay in care, and take medicine as prescribed.
- Tell their provider if they have problems taking the medicine.
- Learn more about HIV care and how to live well with HIV.
Health Departments Can:
- Test people for HIV, and quickly link people with HIV to care.
- Find people who fall out of HIV care, and help them get back in care.
Everyone Can:
- Learn how to prevent HIV, and know their HIV status. gettested.cdc.gov
- Support family and friends who have HIV.
Ending the HIV Epidemic: The pathway is clear. Join us: hiv.gov/federal-response/ending-the-hiv-epidemic/overview
- Ask patients about their challenges taking medicine; talk about the importance of taking it as prescribed.
- Address mental health issues and drug/alcohol misuse, which may make it harder for patients to stay in care.
- Provide a supportive environment for HIV care that includes help with transportation, housing, health insurance, and other needs.
Related Pages and Resources
- Vital Signs: Press Release – Las brechas en la realización de pruebas y el tratamiento del VIH obstaculizan los esfuerzos por detener las nuevas infecciones [Spanish]
- Vital Signs: HIV Transmission Along the Continuum of Care – United States, 2016, Morbidity and Mortality Weekly Report (MMWR)
- HIV Treatment as Prevention
- Preventing HIV
- Treating HIV
Other Sites
- Ending the HIV Epidemic: A Plan for America
- HIV Testing Sites and Care Locator
- US Preventive Services Task Force HIV Screening Recommendations
- HRSA’s Ryan White HIV/AIDS Program AIDS Education and Training Centers Program
- HIV Treatment and Care: A Focus on Mental Health and Substance Use (CME)
- MedlinePlus – HIV/AIDS
- HIV.gov
- AIDSInfo
- UNAIDS
Science Behind the Issue
For More Information
1-800-CDC-INFO (232-4636)
TTY: 1-888-232-6348
Web: www.cdc.gov
Centers for Disease Control and Prevention
1600 Clifton Road NE
Atlanta, GA 30333
Publication date: March 18, 2019