Purpose
- This report summarizes illnesses reported to the Cholera and Other Vibrio Illness Surveillance System (COVIS) in 2019.
- Data include geographic distribution, demographic and clinical characteristics, routes of transmission, and more.
- Maps and charts in this report are interactive. Categories can be shown and hidden by clicking on the legend of each figure.
Surveillance Summary
In 2019, 2,719 Vibrio infections were reported to COVIS.
- 2,708 were cases of vibriosis. Vibriosis is defined as infection with pathogenic species of the family Vibrionaceae other than toxigenic Vibrio cholerae serogroups O1 and O139 (which are generally associated with epidemic or pandemic cholera).
- 1,585 were culture-confirmed cases.
- 1,100 were probable cases detected by a culture-independent diagnostic test (CIDT) and not culture-confirmed.
- 23 were probable cases linked epidemiologically to a laboratory-diagnosed case. Note: Epi-linked cases are not included in the analyses below.
- 1,585 were culture-confirmed cases.
- 11 were cholera cases. Cholera is defined as infection with toxigenic cholerae serogroup O1 or O139.
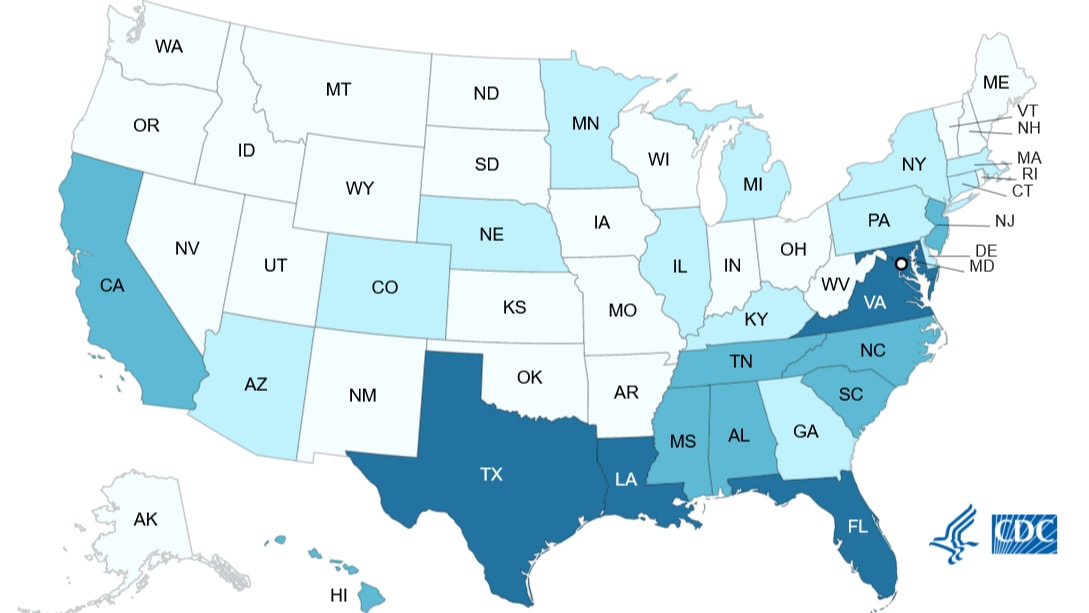
Geographic Distribution of Vibriosis Cases
Jurisdictions that reported vibriosis cases to COVIS during 2019 are shown in Figures 1a–1c.
- 49 jurisdictions reported 2,685 vibriosis cases (Figure 1a).
- Atlantic Coast states reported 789 (29%)
- Gulf Coast states reported 689 (26%)
- Non-coastal states reported 685 (26%)
- Pacific Coast states reported 522 (19%)
- Atlantic Coast states reported 789 (29%)
- 43 jurisdictions reported 670 V. parahaemolyticus cases (Figure 1b).
- Pacific Coast states reported 221 (33%)
- Atlantic Coast states reported 208 (31%)
- Non-coastal states reported 137 (20%)
- Gulf Coast states reported 104 (16%)
- Pacific Coast states reported 221 (33%)
- 26 jurisdictions reported 159 V. vulnificus cases (Figure 1c).
- Gulf Coast states reported 83 (52%)
- Atlantic Coast states reported 50 (31%)
- Non-coastal states reported 15 (9%)
- Pacific Coast states reported 11 (7%)
- Gulf Coast states reported 83 (52%)
Figure 1a
Figure 1b
Figure 1c
Demographic and Clinical Characteristics of Patients
Demographic characteristics and clinical outcomes of patients with vibriosis are shown in Table 1.
- Among culture-confirmed infections, the most frequently reported species was V. parahaemolyticus (655 cases, 41%).
- The median age of patients was 51 years (range <1–103 years); 1,628 (61%) were male.
- 772 (33%) hospitalizations and 70 (3%) deaths were reported.
Table 1
| Demographic Characteristics | Clinical Outcomes | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Genus and Species | Cases | Age (years) | Sex | Hospitalizations | Deaths | ||||
| N | Median | Range | Male (n/N) | % | n/N | % | n/N | % | |
| Confirmed cases | 1,585 | 50 | <1–93 | 1,092/1,574 | 69 | 454/1,370 | 33 | 57/1,426 | 4 |
| V. parahaemolyticus | 655 | 48 | <1–93 | 456/646 | 71 | 114/578 | 20 | 7/586 | 1 |
| V. alginolyticus | 277 | 34 | 2–92 | 189/276 | 68 | 35/213 | 16 | 5/252 | 2 |
| V. cholerae (excluding toxigenic O1 and O139)† | 174 | 51.5 | <1–91 | 104/173 | 60 | 67/161 | 42 | 5/162 | 3 |
| V. vulnificus | 158 | 65 | 6–93 | 138/158 | 87 | 125/146 | 86 | 30/142 | 21 |
| V. fluvialis | 110 | 60 | 6–92 | 63/110 | 57 | 44/94 | 47 | 4/99 | 4 |
| V. mimicus | 37 | 55 | 13–88 | 25/37 | 68 | 8/29 | 28 | 1/33 | 3 |
| G. hollisae | 13 | 43 | 26–65 | 11/13 | 85 | 6/11 | 55 | 0/10 | 0 |
| V. furnissii | 7 | 59 | 29–78 | 3/7 | 43 | 4/4 | 100 | 0/7 | 0 |
| V. harveyi | 6 | 57 | 15–64 | 2/6 | 33 | 1/6 | 17 | 0/5 | 0 |
| V. metschnikovii | 6 | 71.5 | 10–85 | 5/6 | 83 | 3/6 | 50 | 0/6 | 0 |
| P. damselae | 5 | 54 | 6–77 | 4/5 | 80 | 3/4 | 75 | 1/4 | 25 |
| V. cincinnatiensis | 2 | 85.5 | 78–93 | 2/2 | 100 | 2/2 | 100 | 1/2 | 50 |
| V. metoecus | 1 | 41 | 41–41 | 0/1 | 0 | 1/1 | 100 | 0/1 | 0 |
| V. navarrensis | 1 | 4 | 4–4 | 1/1 | 100 | 0/0 | - | 0/1 | 0 |
| V. ponticus | 1 | 30 | 30–30 | 0/1 | 0 | 0/1 | 0 | 0/1 | 0 |
| Multiple Species | 44 | 53 | 4–89 | 29/44 | 66 | 12/36 | 33 | 1/36 | 3 |
| Species not identified | 88 | 47.5 | 1–90 | 60/88 | 68 | 29/78 | 37 | 2/79 | 3 |
| Probable cases†† | 1,100 | 53 | <1–103 | 536/1,091 | 49 | 318/978 | 33 | 13/971 | 1 |
| V. cholerae (serogroup not specified) | 197 | 49 | <1–97 | 98/196 | 50 | 56/166 | 34 | 3/176 | 2 |
| V. parahaemolyticus | 15 | 65.5 | 24–85 | 8/15 | 53 | 0/14 | 0 | 0/15 | 0 |
| V. vulnificus | 1 | 57 | 57–57 | 0/1 | 0 | 1/1 | 100 | 0/1 | 0 |
| Species not identified | 887 | 53 | <1–103 | 430/879 | 49 | 261/797 | 33 | 10/779 | 1 |
| Total | 2,685 | 51 | <1–103 | 1,628/2,665 | 61 | 772/2,348 | 33 | 70/2,397 | 3 |
*Proportions of demographic characteristics and clinical outcomes are based on total cases with known information, by genus and species.
†Includes non-toxigenic V. cholerae non-O1, non-O139 (123 cases); non-O1 (19 cases); serogroup not specified (19 cases); O1 (7 cases); O141 (4 cases); and O75 (2 cases).
††Species are summarized according to how they were reported to COVIS. Multiplex polymerase chain reaction (PCR) panels used to identify the vast majority of probable vibriosis cases are not known to provide species-level results; such cases are considered “Species not identified.” However, some brands or laboratory-developed “in-house” PCR tests that are designed to provide species-level results have been reported to COVIS and are therefore included in this table.
Routes of Transmission
Transmission routes are classified based on exposure categories (seafood consumption and marine/estuarine contact) and the type(s) of clinical specimen from which the Vibrio bacteria was isolated. More information can be found in the appendix: Method for Classification of Transmission Routes in COVIS. The proportion of domestically acquired cases with each transmission route and species are shown in Figures 2a–c. The frequency of domestically acquired cases by transmission route and month are shown in Figures 3a–c.
- Among 2,214 cases of vibriosis with known travel information, 215 (10%) reported international travel in the 7 days before illness began.
- Of 2,470 domestically acquired vibriosis cases:
- 1,754 (71%) were classified as foodborne or likely foodborne transmission.
- 575 (23%) were classified as non-foodborne or likely non-foodborne transmission.
- 141 (6%) were classified as unknown transmission.
- 1,754 (71%) were classified as foodborne or likely foodborne transmission.
Figure 2a
Figure 2b
Figure 2c
Figure 3a
Figure 3b
Figure 3c
Seafood, Marine, and Estuarine Exposures
Seafood exposures among domestically acquired vibriosis cases are shown in Tables 2a–c.
- Among patients with domestically acquired vibriosis who reported eating seafood (N=1,233)
- 685 (56%) consumed oysters, 490 (40%) consumed shrimp, and 468 (38%) consumed fish.
- Among those who reported eating a single seafood item, 287 (47%) ate oysters, 85% of whom consumed them raw.
- 685 (56%) consumed oysters, 490 (40%) consumed shrimp, and 468 (38%) consumed fish.
- Among patients with domestically acquired vibriosis who reported a marine or estuarine exposure (N=714)
- 607 (85%) reported having skin exposure to a body of water within 7 days before illness onset.
- 213 (30%) reported contact with drippings from raw or live seafood.
- 77 (11%) reported contact with marine life.
- 607 (85%) reported having skin exposure to a body of water within 7 days before illness onset.
Table 2a
| Mollusks | Crustaceans | Other | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Oysters | Clams | Scallops | Mussels | Shrimp | Crab | Crayfish | Lobster | Finfish | Other Shellfish | |
| Patients who ate single seafood item, n (% of 606) | 287 (47) | 20 (3) | 6 (1) | 3 (0) | 102 (17) | 45 (7) | 12 (2) | 5 (1) | 123 (20) | 3 (0) |
| Patients who ate the single seafood item raw, n (% of n in row above) | 244 (85) | 14 (70) | 0 (0) | 1 (33) | 8 (8) | 4 (9) | 0 (0) | 1 (20) | 23 (19) | 0 (0) |
*Includes all vibriosis cases, culture-confirmed and CIDT-positive only, reported to COVIS.
Table 2b
| Mollusks | Crustaceans | Other | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Oysters | Clams | Scallops | Mussels | Shrimp | Crab | Crayfish | Lobster | Finfish | Other Shellfish | |
| Patients who ate single seafood item, n (% of 387) | 226 (58) | 17 (4) | 5 (1) | 2 (1) | 42 (11) | 29 (7) | 8 (2) | 4 (1) | 53 (14) | 1 (0) |
| Patients who ate the single seafood item raw, n (% of n in row above) | 193 (85) | 12 (71) | 0 (0) | 1 (50) | 6 (14) | 4 (14) | 0 (0) | 1 (25) | 13 (25) | 0 (0) |
*Includes vibriosis cases reported to COVIS that were culture-confirmed.
Table 2c
| Mollusks | Crustaceans | Other | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Oysters | Clams | Scallops | Mussels | Shrimp | Crab | Crayfish | Lobster | Finfish | Other Shellfish | |
| Patients who ate single seafood item, n (% of 219) | 61 (28) | 3 (1) | 1 (0) | 1 (0) | 60 (27) | 16 (7) | 4 (2) | 1 (0) | 70 (32) | 2 (1) |
| Patients who ate the single seafood item raw, n (% of n in row above) | 51 (84) | 2 (67) | 0 (0) | 0 (0) | 2 (3) | 0 (0) | 0 (0) | 0 (0) | 10 (14) | 0 (0) |
*Includes vibriosis cases reported to COVIS that were CIDT-positive but not culture-confirmed.
National Cholera Surveillance
In 2019, 11 cholera cases were reported to COVIS. These cases are summarized in Table 3.
- All were toxigenic V. cholerae serogroup O1 infections and had a marker (found in the tcpA gene) identified by PCR that identified the isolate as the El Tor biotype.
- 6 (55%) patients were hospitalized, and none died.
- Among 10 cases with travel information, all were international travel-associated. Travel destinations include Kenya (4), Pakistan (2), Yemen (2), Bangladesh (1), and India (1).
Table 3
| Location | Age | Sex | Month of Illness Onset | International Travel | Serogroup | Serotype |
|---|---|---|---|---|---|---|
| Illinois | 64 | F | February | Pakistan | O1 | Inaba |
| Massachusetts | 64 | F | September | Kenya | O1 | Inaba |
| Michigan | 67 | F | March | Yemen | O1 | Ogawa |
| Michigan | 38 | M | August | Kenya | O1 | Inaba |
| Minnesota | 68 | M | February | Pakistan | O1 | Inaba |
| Minnesota | 36 | M | April | Kenya | O1 | Inaba |
| Minnesota | 40 | M | April | Kenya | O1 | Inaba |
| New Jersey | 72 | F | September | India | O1 | Ogawa |
| New York | 44 | F | September | Bangladesh | O1 | Ogawa |
| North Carolina | 63 | M | September | Yemen | O1 | Ogawa |
| Wisconsin | 43 | F | October | Unknown | O1 | Inaba |
*V. cholerae isolates sent to CDC undergo antimicrobial susceptibility testing through the National Antimicrobial Resistance Monitoring System (NARMS) laboratory. Among 21 toxigenic V. cholerae O1 isolates tested by NARMS from 2017–2019, 11 (52%) had antimicrobial resistance to both sulfisoxazole and trimethoprim-sulfamethoxazole. 7 (33%) had intermediate susceptibility to ampicillin. 1 (5%) had intermediate susceptibility to chloramphenicol. 17 (81%) had decreased susceptibility to both ciprofloxacin (MIC >=0.12 ug/mL) and nalidixic acid (MIC >32 ug/mL). None had resistance to ampicillin, azithromycin, chloramphenicol, or tetracycline.
Appendix: Method for Classification of Transmission Routes in COVIS
Exposure categories
To classify transmission routes, the first step is to categorize patient exposures. For a given illness episode, more than one patient exposure can be reported to COVIS; each reported exposure is categorized individually. If all exposures fall into a single category, then the case is considered to have a single exposure category. If not, the case is considered to have multiple exposure categories. For a given case, if any exposure is reported, we assume that other exposures for which information was not reported were not present. Exposures are classified using three categories:
- Seafood consumption: Ingestion of any type of seafood. Does not include touching seafood.
- Marine/estuarine contact: Includes direct skin contact with marine/estuarine life, bodies of water, or drippings from raw or live seafood.
- Unknown or no exposure: All seafood consumption or marine/estuarine exposure history questions are reported as unknown, or no exposures are reported.
Specimen site categories
The next step in classifying transmission routes is to categorize reported specimen sites. For a given illness episode, more than one specimen site can be reported; each reported site is categorized individually. If all specimen sites fall into a single category, then the report is considered to have a single specimen site category. If not, then the report is considered to have multiple specimen site categories. Specimen sites are classified using five categories:
- Gastrointestinal site (GI): stool, bile, appendix, rectum, gall bladder, colon
- Blood or other normally sterile site (sterile): blood, cerebrospinal fluid (CSF), peritoneal fluid, lumbar disc fluid, lymph node, bullae
- Skin or soft tissue site (SST): wound, ear (other than otitis media and middle ear, which are included in 'other, non-sterile site'), appendage, tissue
- Other, non-sterile site (ONS): urine, sputum, aspirate, bronchial washing, effusion, catheter, endotracheal, eye, nasal, placenta, respiratory, sinus, tonsil
- Unknown site (unknown): no specimen site reported or no site specified for 'other'
Note: The lists of sites for each category above are not intended to be exhaustive. Rather, they reflect the sites traditionally reported to COVIS and may be updated if new sites are reported.
Transmission route
The final step in classifying transmission involves review of exposure and specimen site categories for each reported case. Cases are classified into one of five transmission routes (foodborne, likely foodborne, non-foodborne, likely non-foodborne, and unknown) based on the criteria below:
- Single exposure category: seafood consumption
- Foodborne: Vibrio isolated only from GI or sterile site OR Vibrio isolated from multiple specimen site categories, with GI reported.
- Likely Foodborne: Vibrio isolated only from SST, ONS, or unknown sites OR Vibrio isolated from multiple specimen site categories, not including GI.
- Foodborne: Vibrio isolated only from GI or sterile site OR Vibrio isolated from multiple specimen site categories, with GI reported.
- Single exposure category: marine/estuarine contact
- Non-foodborne: Vibrio isolated only from SST or sterile site OR Vibrio isolated from multiple specimen site categories, with SST reported.
- Likely Non-foodborne: Vibrio isolated only from GI, ONS, or unknown sites OR Vibrio isolated from multiple specimen site categories, not including SST.
- Non-foodborne: Vibrio isolated only from SST or sterile site OR Vibrio isolated from multiple specimen site categories, with SST reported.
- Multiple exposure categories: both seafood consumption AND marine/estuarine contact
- Foodborne: Vibrio isolated only from a GI site OR Vibrio isolated from multiple specimen site categories, with GI reported and SST not reported.
- Non-foodborne: Vibrio isolated only from a SST site OR Vibrio isolated from multiple specimen site categories, with SST reported and GI not reported.
- Unknown: Vibrio isolated only from a sterile, ONS, or unknown site OR Vibrio isolated from multiple specimen site categories, including either 1) both GI and SST or 2) neither GI nor SST.
- Foodborne: Vibrio isolated only from a GI site OR Vibrio isolated from multiple specimen site categories, with GI reported and SST not reported.
- Unknown or no reported exposure (note that categorization is the same as for multiple exposure categories)
- Foodborne: Vibrio isolated only from a GI site OR Vibrio isolated from multiple specimen site categories, with GI reported and SST not reported.
- Non-foodborne: Vibrio isolated only from a SST site OR Vibrio isolated from multiple specimen site categories, with SST reported and GI not reported.
- Unknown: Vibrio isolated only from a sterile, ONS, or unknown site OR Vibrio isolated from multiple specimen site categories, including either 1) both GI and SST or 2) neither GI nor SST.
- Foodborne: Vibrio isolated only from a GI site OR Vibrio isolated from multiple specimen site categories, with GI reported and SST not reported.
