Key points
- Physicians who suspect tularemia should alert the laboratory to the possible need for special diagnostic and safety procedures.
- Positive serologic tests should be interpreted in the context of a compatible clinical illness and exposure.
Laboratory diagnosis
Confirmatory and supportive results for all recommended diagnostic tests for F. tularensis infection are listed below. Physicians who suspect tularemia should alert the laboratory to the possible need for special diagnostic and safety procedures.
Confirmatory
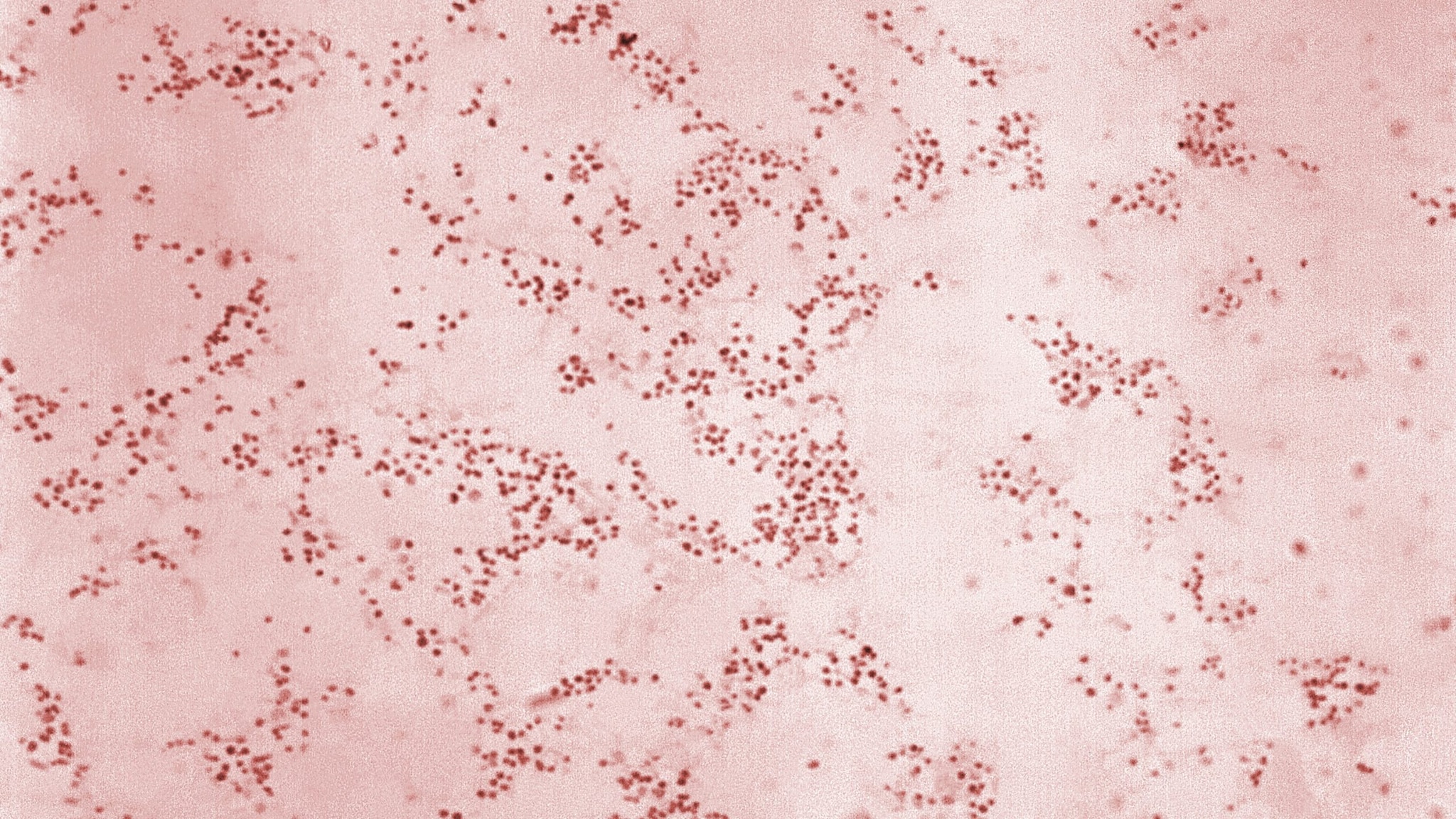
- Isolation of F. tularensis from a clinical specimen; appropriate specimens include scrapings of ulcers, conjunctival swabs, lymph node aspirates or biopsies, blood or respiratory specimens (e.g. pleural fluid), depending on the form of illness. The laboratory should be alerted if F. tularensis is suspected so cultures can be incubated for extended periods, due to the fastidious, slow-growing nature of the bacterium.
- Seroconversion from negative to positive IgM and/or IgG antibodies in paired sera. Ideally, the first serum sample would be collected during the acute phase of illness (within first week of onset) and the second serum sample would be collected 2–3 weeks later.
Supportive
- Detection of F. tularensis in a clinical specimen by immunohistochemical staining, sequence-based technologies, or polymerase chain reaction (PCR) assay.
- Detection of antibodies to F. tularensis through a single serologic test. Ideally, serum would be collected at least 14 days after illness onset to ensure sufficient time for development and detection of an antibody response.
Diagnostic considerations for serologic testing
- Antibodies are often not detectable until 2–3 weeks after symptom onset.
- A rise in IgM and IgG antibodies often occurs concurrently.
- Once increased, both IgM and IgG antibodies may remain detectable for several years following resolution of disease.
- Note: some serologic tests detect total antibody levels and do not distinguish between IgM and IgG.
- Positive serologic tests should be interpreted in the context of a compatible clinical illness and exposure. The validity of a positive test result depends on the probability that a person has the disease (positive predictive value) and the sensitivity and specificity of the diagnostic test.
- A negative serologic test soon after illness onset does not exclude the diagnosis of tularemia. A second test obtained several weeks later is needed to confirm or exclude the diagnosis.
- Patients with acute illness should be managed based on clinical suspicion.
- Serology is not useful for proving that a patient has been cured of tularemia.
- False positive results by serologic testing can occur for many diseases, including tularemia. Non-specific antibody binding can lead to false positives by serologic testing. F. tularensis serologic tests may also cross-react with antibodies to some other bacteria, including Brucella.
- Repeat testing may be useful if testing was performed early after illness onset—before detectable levels of antibodies developed. In this case, it can be useful to document seroconversion. If seroconversion did not occur, it is possible that another condition may be responsible for the patient's illness.
- Repeat testing may also be useful if an initial test result falls in the equivocal or borderline range. This result may occur when testing is performed on a serum sample drawn soon after illness onset, before the antibody response has fully developed. An equivocal or borderline serologic test result may also be due to non-specific antibody binding or antibody cross-reactivity. If the test result does not change with repeat testing, it is possible another condition may be responsible for the current symptoms.
Reporting cases
Notes regarding interpretation of tularemia serologic test results for public health purposes:
- Positive serologic tests should be interpreted in the context of a compatible clinical illness and exposure. False positive results by serologic testing can occur for many diseases, including tularemia.
- Some commercial laboratories perform reflex testing to improve overall specificity of serologic testing. Check the commercial laboratory test directory website for information to ensure that all test results, including any reflex tests, have been received. Check with the reporting laboratory to obtain reflex testing results.
For emergency assistance after hours, please contact the CDC Emergency Operations Center (EOC) at 770-488-7100.
- Petersen JM and Dietrich EA. Detection of Francisella tularensis Antibodies. In: Leber AL and Burnham CAB, eds. Clinical Microbiology Procedures Handbook, 4th Edition. 2021. ASM Press, Washington DC.
- Maurin M. Francisella tularensis, tularemia and serological diagnosis. Review Front Cell Infect Microbiol. 2020 Oct 26;10:512090.
