Key points
- Spina bifida is a condition that affects the spine and is usually apparent at birth.
- It can happen anywhere along the spine if the neural tube does not form properly or close all the way.
- The severity of spina bifida can range from mild to severe.
- Spina bifida occurs among 1 in every 2,875 U.S. births each year.

What it is
Spina bifida is a condition that affects the spine and is usually apparent at birth. It is a type of neural tube defect (NTD).
Spina bifida can happen anywhere along the spine if the neural tube does not form properly or close all the way. When the neural tube doesn't close all the way, the backbone that protects the spinal cord doesn't form and close. This often results in damage to the spinal cord and nerves.
In the United States
Each year, about 1,278 babies are born with spina bifida, or 1 in every 2,875 births.1Hispanic women have the highest rate of having a child with spina bifida compared with non-Hispanic white and non-Hispanic black women.
Data from birth defects tracking programs were used to estimate the total number of pregnancies affected by spina bifida in the United States and are estimated as follows:
- Hispanic: 3.80 per 10,000 live births
- Non-Hispanic black or African-American: 2.73 per 10,000 live births
- Non-Hispanic white: 3.09 per 10,000 live births
Types
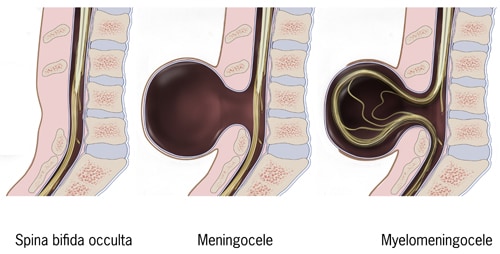
The three most common types of spina bifida include spina bifida occulta, meningocele, and myelomeningocele.
Myelomeningocele
(sounds like: my-low-ma-nin-jo-seal)
When people talk about spina bifida, most often they are referring to myelomeningocele. Myelomeningocele is the most serious type of spina bifida. With this condition, a sac of fluid comes through an opening in the baby's back. Part of the spinal cord and nerves are in this sac and are damaged. This type of spina bifida causes moderate to severe disabilities, such as not being able to move the legs.
Meningocele
(sounds like: ma-nin-jo-seal)
Meningocele happens when a sac of fluid comes through an opening in the baby's back, but the spinal cord is not in this sac. There is usually little or no nerve damage. This type of spina bifida can cause minor disabilities.
Spina bifida occulta
(sounds like: o-cult-tuh)
Spina bifida occulta is the mildest type of spina bifida and usually does not cause disabilities. It is sometimes called "hidden" spina bifida. With it, there is a small gap in the spine, but no opening or fluid sac on the back. The spinal cord and the nerves usually are normal. Many times, spina bifida occulta is not discovered until late childhood or adulthood.
Risk factors
We do not know all the causes of spina bifida. The role that genetics and the environment play in causing spina bifida needs to be studied further.
Research studies have reported some factors that might increase the chance of having a baby with spina bifida:
- Not getting enough folic acid daily
- Certain medications
- Diabetes that is not well-controlled
- Overheating or fever
Screening and diagnosis
Spina bifida can be diagnosed during pregnancy or after the baby is born. Spina bifida occulta might not be diagnosed until late childhood or adulthood or might never be diagnosed.
During pregnancy
During pregnancy, there are screening tests (prenatal tests) to check for spina bifida and other birth defects. For example, an AFP (alpha-fetoprotein) test might be part of a test called the “quad screen.” A high level of AFP might mean that a baby has spina bifida. Frequently, spina bifida can be seen with an ultrasound, which is a type of picture of the baby.
After the baby is born
In some cases, spina bifida might not be diagnosed until after the baby is born. Sometimes there is a hairy patch of skin or a dimple on the back that is seen after birth. A doctor can use an image scan, such as an X-ray, to get a clearer view of the baby's spine.
Treating spina bifida during pregnancy
Some scientists think that the impact of spina bifida to the legs, bladder and bowel may begin during pregnancy. Therefore, closing the opening in the back during pregnancy may reduce long-term disability associated with spina bifida. The Management of Myelomeningocele Study (MOMS) Trial looked at infants who had this surgery before 26 weeks of pregnancy. This landmark study found that closing spina bifida during pregnancy can:
- Decrease the risk of death in infancy from spina bifida
- Decrease the need for shunting by the end of the first year of life
- Improve motor function in childhood
This treatment does not come without risks, including problems with the placenta and infection. The rate of death in the first year of life ranged from 0-20%, but most reports show rates in the 2-6% range.2
- Stallings EB, Isenburg JL, Rutkowski RE, et al. National population-based estimates for major birth defects, 2016-2020. Birth Defects Res. 2024;116(1):e2301. https://doi.org/10.1002/bdr2.2301
- Paslaru FG, Panaitescu AM, Iancu G, Veduta A, Gica N, Paslaru AC, Gheorghiu A, Peltecu G, Gorgan RM. Myelomeningocele Surgery over the 10 Years Following the MOMS Trial: A Systematic Review of Outcomes in Prenatal versus Postnatal Surgical Repair. Medicina (Kaunas). 2021 Jul 12;57(7):707. doi: 10.3390/medicina57070707. PMID: 34356988; PMCID: PMC8307221. Myelomeningocele Surgery over the 10 Years Following the MOMS Trial: A Systematic Review of Outcomes in Prenatal versus Postnatal Surgical Repair - PubMed
