Purpose
Medical providers should know the steps to take in evaluating patients with an acute, generalized vesicular or pustular rash illness.
View and download the protocol
Downloadable files
Steps to evaluate patients
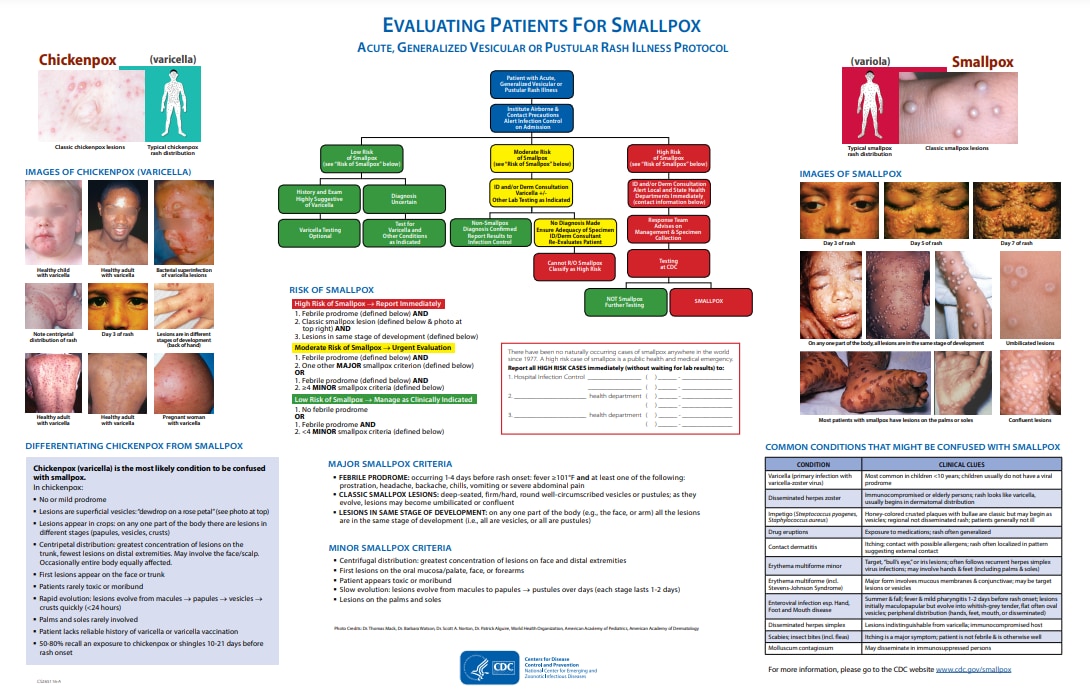
In the center of the graphic, the flow chart describes the steps medical providers should take to evaluate a patient with an acute, generalized vesicular or pustular rash illness. The steps are:
-
-
- When a patient presents with an acute, generalized vesicular or pustular rash illness, institute airborne and contact precautions. Alert infection control on admission.
- Determine the patient’s risk of smallpox using the MAJOR and MINOR criteria.
- There are three MAJOR criteria:
- Febrile prodrome: Fever of ≥101°F, 1–4 days prior to rash onset with at least prostration, headache, backache, chills, vomiting or severe abdominal pain
- Classic smallpox lesions: Deep-seated, firm/hard, round well-circumscribed vesicles or pustules; lesions may umbilicate or become confluent
- Lesions in same stage of development: On any one part of the body all lesions in same stage of development
- There are five MINOR criteria:
- Centrifugal distribution of lesions
- First lesions on the oral mucosalpalate, face, or forearms
- Patient appears toxic or moribund
- Slow evolution of lesions from macule, to papule, to vesicle (1-2 days each stage)
- Lesions on the palms and soles
- If the patient has no febrile prodrome OR has febrile prodrome AND <4 MINOR criteria, the patient’s risk of smallpox is low.
- If the patient has a history and exam suggestive of varicella, varicella testing is optional, and risk of smallpox is low.
- If the diagnosis is uncertain, test for varicella and other conditions as indicated. Risk of smallpox is low.
- If the patient has a febrile prodrome AND one other MAJOR smallpox criterion OR if the patient has a febrile prodrome AND ≥ 4 MINOR criteria, the patient’s risk of smallpox is moderate.
- Obtain Infectious Disease and/or Dermatology consultation.
- Test for Varicella and other conditions as indicated.
- If tests confirm a non-smallpox diagnosis, report results to infection control. The patient’s risk of smallpox is low.
- If no diagnosis is made after tests are completed, ensure specimen adequacy and re‑evaluate the patient. At this point, the patient’s risk of smallpox is moderate.
- If re‑evaluation does not reveal a diagnosis, you CANNOT rule out smallpox. Patient’s risk of smallpox is HIGH.
- If the patient has a febrile prodrome AND classic smallpox lesions AND lesions in the same stage of development, the patient’s risk of smallpox is HIGH.
- Obtain Infectious Disease and/or Dermatology consultation and alert local and state public health departments immediately.
- The Response team from the local and/or state public health department will advise on management and specimen collection.
- Perform variola testing at variola testing laboratory and at CDC
- If variola testing rules out smallpox, continue other diagnostic testing. Patient’s risk of smallpox is low.
- If variola is positive, then smallpox is confirmed.
- There are three MAJOR criteria:
-
There have been no naturally occurring cases of smallpox anywhere in the world since 1977. A high-risk case of smallpox is a public health and medical emergency. Report all HIGH-RISK CASES immediately (without waiting for lab results) to hospital infection control and applicable public health department.
Report high-risk cases immediately
Images of patients with smallpox
On the right side of the graphic, there are images of patients with smallpox. These images show the classic smallpox lesions and the typical smallpox rash distribution. Images of patients with smallpox show that on any one part of the body, all lesions are in the same stage of development. Other images show the lesions are umbilicated, may be confluent, and that most patients with smallpox have lesions on the palms or soles.
Common conditions that might be confused with smallpox
On the bottom right of the graphic above, there is a table listing the common conditions that might be confused with smallpox. These conditions and their clinical cues are listed below.
| Condition | Clinical Clues |
|---|---|
| Varicella (primary infection with varicella-zoster virus) |
|
| Disseminated herpes zoster |
|
| Impetigo (Streptococcus pyogenes, Staphylococcus aureus) |
|
| Drug eruptions |
|
| Contact dermatitis |
|
| Erythema multiforme minor |
|
| Erythema multiforme major (Stevens-Johnson syndrome) |
|
| Enteroviruses infection, especially Hand, Foot, and Mouth Disease |
|
| Disseminated herpes simplex |
|
| Scabies; insect bite (including fleas) |
|
| Molluscum contagiosum |
|
Differentiating chickenpox
On the left side of the graphic, there are images of patients with chickenpox (varicella), classic chickenpox lesions, and the typical chickenpox rash distribution. The images of patients with chickenpox show the centripetal distribution of the rash. Another image shows the back of a patient's hand, with lesions in different stages of development.
On the bottom left of the graphic, there is a table listing the ways to differentiate chickenpox from smallpox. Chickenpox (varicella) is the most likely condition to be confused with smallpox. In chickenpox:
- No or mild prodrome
- Lesions are superficial vesicles: "dewdrop on a rose petal"
- Lesions appear in crops: on any one part of the body there are lesions in different stages (papules, vesicles, crusts)
- Centripetal distribution: greatest concentration of lesions on the trunk, fewest lesions on distal extremities. May involve the face/scalp. Occasionally entire body equally affected.
- First lesions appear on the face or trunk
- Patients rarely toxic or moribund
- Rapid evolution: lesions evolve from macules to papules to vesicles to crusts quickly (<24 hours)
- Palms and soles rarely involved
- Patient lacks reliable history of varicella or varicella vaccination
- 50-80% recall an exposure to chickenpox or shingles 10-21 days before rash onset
