Purpose
Hospital Sepsis Program Core Elements are essential to optimize patient care and help clinicians, hospitals, and health systems in efforts to improve the hospital management and outcomes of sepsis. Hospital Sepsis Program Core Elements outline structural and procedural components that are associated with the multidisciplinary expertise required to support the care of patients with sepsis.
Overview
Sepsis Core Elements: CDC Webinar Series with Free Continuing Education (CE)
Each webinar is independent and you can complete one or more of them for free CE.
Getting Started
For hospitals or healthcare systems just starting a sepsis program or those with limited resources.
Assessment Tool
This tool provides examples of ways to implement the Core Elements.
Resources
Practical resources that can help hospitals improve specific aspects of their sepsis programs.
Summary of Hospital Sepsis Program Core Elements
The development of a multi-disciplinary hospital sepsis program is critical to monitoring and improving the management and outcomes of patients with sepsis. Hospital quality improvement programs focused on sepsis have been associated with reductions in hospital mortality, length of stay, and healthcare costs.37-39
The structure of hospital sepsis programs may be specific to a single hospital or span an entire healthcare system. Likewise, programs may focus on sepsis specifically or may be part of a broader initiative that addresses multiple areas of quality improvement. Regardless of the structure of the hospital sepsis program, it should help healthcare staff improve outcomes from sepsis by aiding in the recognition of sepsis, facilitating the implementation of evidence-based management of sepsis, supporting the recovery of patients after sepsis, and monitoring the impact of hospital-based interventions to improve care and outcomes of sepsis.
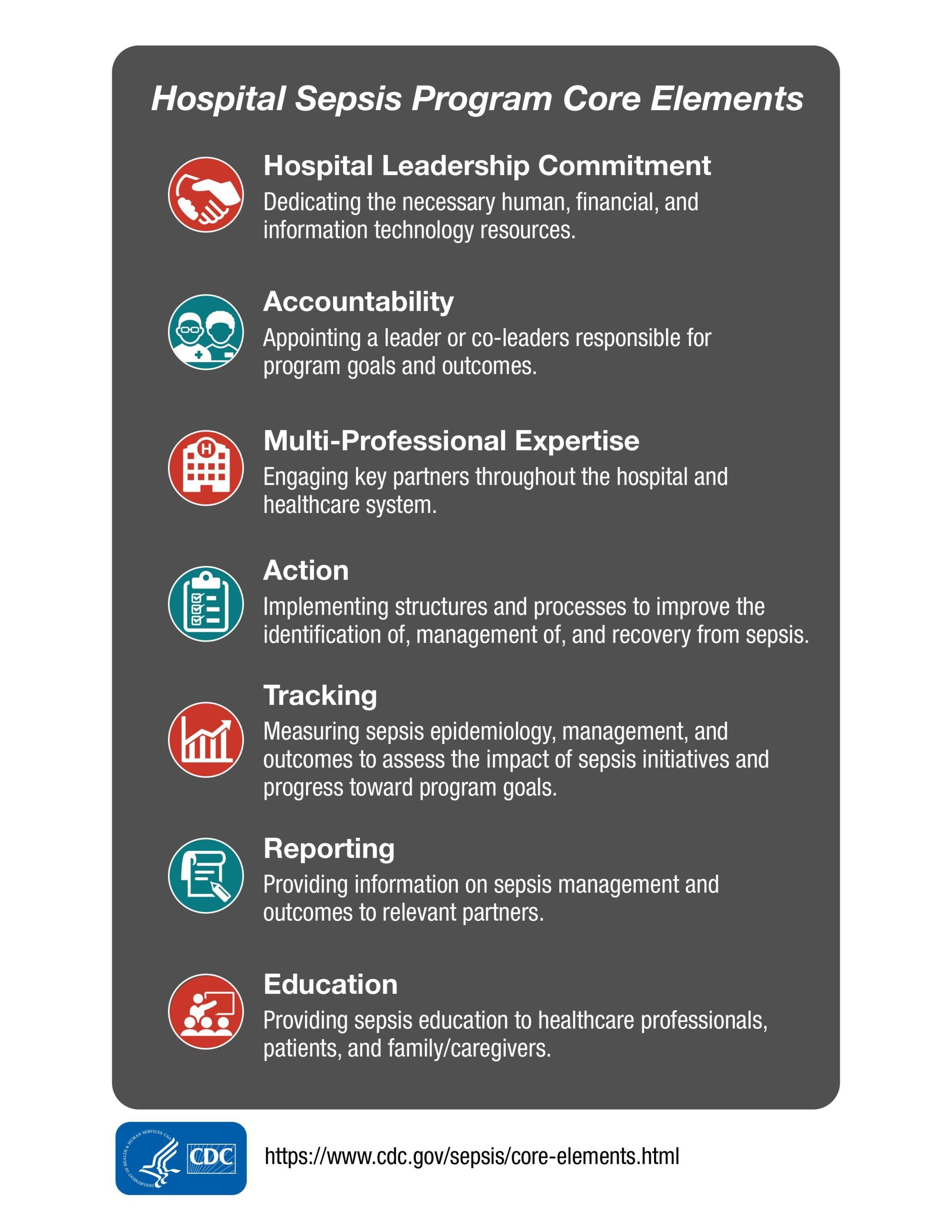
The Hospital Sepsis Program Core Elements include:
- Hospital Leadership Commitment: Dedicating the necessary human, financial, and information technology resources.
- Accountability: Appointing a leader or co-leaders responsible for program goals and outcomes.
- Multi-professional expertise: Engaging key partners throughout the hospital and healthcare system.
- Action: Implementing structures and processes to improve the identification of management of, and recovery from sepsis.
- Tracking: Measuring sepsis epidemiology, management, and outcomes to assess the impact of sepsis initiatives and progress toward program goals.
- Reporting: Providing information on sepsis management and outcomes to relevant partners.
- Education: Providing sepsis education to healthcare professionals, patients, and family/caregivers.
For each Core Element, "Priority Examples" are provided as the top priorities for hospital sepsis programs, and "Additional Examples" are additional important recommendations that can further enhance these programs.
For programs that are new or are reorganizing, the "Getting Started" box may be helpful for prioritizing initial activities.
Getting Started
For hospitals or healthcare systems just starting a sepsis program or those with limited resources, it maybe most efficient to address the following steps first:
- Identify the sepsis program leader or co-leaders
- Secure support from hospital or healthcare system leadership
- Conduct a needs analysis to identify applicable regulatory or reporting requirements (e.g., Centers for Medicare & Medicaid Services [CMS] Severe Sepsis and Septic Shock: Management Bundle [SEP-1]), existing sepsis screening processes, treatment guidelines, and order sets. Obtain summary data on regulatory performance and use of sepsis screening tools and order sets to identify areas in need of improvement.
- Establish initial goals for sepsis program based on needs analysis.
Core Elements Introduction
The burden of sepsis
Sepsis is defined as "life-threatening organ dysfunction caused by a dysregulated host response to infection".1 While sepsis is often attributed to bacterial infections, sepsis may result from infections of any etiology, including viral infections such as COVID-19. Sepsis is a leading cause of hospitalization and hospital mortality,2 contributing to over a third of all hospital deaths.34 In the United States (U.S.), there are an estimated 1.7 million adult sepsis hospitalizations annually, of which 350,000 result in hospital death or discharge to hospice.5 Beyond being a major driver of hospital mortality, sepsis also contributes to incident disability.6 Patients who survive hospitalization for sepsis are at increased risk for negative health outcomes including the development of new morbidity, inability to return to work, hospital readmission, and death.789 Due to the burden of morbidity and mortality from sepsis, the World Health Organization recognized sepsis as a global health priority in 2017.10 Despite the burden of sepsis and importance of early treatment, community knowledge of sepsis remains low.11
Efforts to improve sepsis identification, management, and outcomes
There have been many initiatives to improve identification, management, and outcomes of sepsis over the past two decades. The Surviving Sepsis Campaign first published international guidelines for the management of sepsis in 2004, and has issued updates to these guidelines every four years.1213 Dedicated pediatric guidelines were added in 2020. 1415More recent updates to the guidelines have used the GRADE approach to assess the quality of the evidence and formulate recommendations using an "evidence-to-decision framework" that takes into account not only the magnitude of effect and quality of evidence, but also patient values, resources and cost, equity, acceptability, and feasibility.16171819 Large-scale quality improvement and state-based regulatory initiatives (e.g. New York State Department of Health's "Rory's Regulations") focused on recognition and early management of sepsis have been associated with reductions in in-hospital mortality.2021222324 The Centers for Medicare & Medicaid Services (CMS) Severe Sepsis and Septic Shock: Management Bundle (SEP-1) has further emphasized the importance of early sepsis management in U.S hospitals. Recently, there is growing interest in and use of clinical decision support to facilitate sepsis recognition and treatment, although more work is needed to improve the accuracy, usability, and clinical impact of clinical decision support for sepsis.25262728293031
The challenges of implementing sepsis care
Despite the availability of evidence-based guidelines for sepsis, success of several large-scale quality improvement initiatives, and growing interest in clinical decision support, there remains much work to ensuring optimal sepsis care in hospitals. Sepsis is a complex condition that requires care to be coordinated across multiple clinical care locations and disciplines, and to be tailored to specific infections and clinical presentations. Ethnographic studies demonstrate that the implementation of seemingly simple sepsis bundles "involve[s] a complex trajectory comprising multiple interdependent tasks that require prioritization and scheduling, and which are prone to problems of coordination and operational failures."32 Five factors were identified as critical for improving the delivery of recommended sepsis practices:33
- Healthcare staff knowing what to do and why.
- Healthcare staff understanding risks and benefits of treatments.
- Healthcare staff having strong team collaboration.
- Healthcare staff feeling empowered and supported.
- Hospitals having adequate staffing.
Beyond the challenges of coordinating multi-disciplinary care, the best practices for sepsis treatment continue to evolve. Many guideline statements are based on weak evidence, such that guidance may change as more evidence is accrued.16 Given this landscape, hospitals must have processes in place to implement recommended sepsis practices and also evolve practice over time in response to accruing evidence.
The Purpose of the Hospital Sepsis Program Core Elements
This document summarizes Core Elements of hospital sepsis programs, which are intended to monitor and optimize hospital management and outcomes of sepsis. It complements existing sepsis guidelines, and helps facilitate implementation of guideline-recommended care practices that apply to a broad range of persons with sepsis, including adults, children, and people who are pregnant or post-partum.1418193435 There is no single template for a hospital sepsis program. Rather, the complexity of medical decision-making in identification and management of sepsis, and the variability of sepsis epidemiology and patient populations served by hospitals in the U.S. require flexibility in the structure of hospital sepsis programs and the implementation of sepsis care. However, sepsis programs can be implemented effectively in a wide variety of hospitals and healthcare systems, and this guidance lays out key features of effective programs.36 The guidance is informed by expert knowledge, examination of peer-reviewed literature, and extrapolation from the features of effective quality improvement programs addressing sepsis and other conditions.
Hospital Leadership Commitment
Support from hospital and health system leadership, especially that of the chief medical and chief nursing officers, is critical to the success of hospital sepsis programs.3738 Barriers to successful hospital sepsis programs include lack of engagement from hospital clinicians and staff and insufficient resources to effectively run the hospital sepsis program (e.g., lack of personnel, lack of analytic support, or insufficient time for sepsis activities). By setting sepsis performance improvement as a priority and allocating necessary resources to the program, hospital leadership can help ensure that sepsis programs have the engagement and resources necessary to accomplish their goals.
Priority examples of leadership commitment include:
- Providing the sepsis program leader(s) with dedicated time to manage the hospital sepsis program and to participate in sepsis-related performance evaluation and improvement activities. The amount of time required will vary depending on the type and size of hospital or healthcare system, but meaningful dedicated effort is required rather than volunteer service.
- Providing resources, including data analytics and information technology support, to operate the program effectively. Analytic and information technology support services may be provided by third party vendors, contracted personnel, or at the system level if expertise is not available in the hospital.
- Ensuring that relevant staff from key clinical groups and support departments have sufficient time to contribute to sepsis activities.
- Appointing a senior administrator (e.g., Chief Clinical Officer, Chief Medical Officer, of Chief Nursing Officer) to serve as an executive sponsor for the sepsis program to ensure the program has resources and support needed to accomplish its mission.
- Identifying sepsis as a hospital priority and communicating this priority to hospital staff.
Additional examples of leadership commitment include:
- Communicating to hospital staff and patients how the hospital is addressing sepsis.
- Having regular meetings with leaders of the sepsis program to assess the resources needed to accomplish the hospital's goals for sepsis activities and outcomes.
- Integrating sepsis activities into other quality improvement and patient safety efforts, such as emergency department (ED) triage, antimicrobial stewardship, transitions of care, and CMS Severe Sepsis and Septic Shock: Management Bundle (SEP-1)
- Tying staff performance incentives to the achievement of targets for sepsis care and/or outcomes.
- Including sepsis program-related duties in job descriptions or performance reviews for program leaders and key support staff.
- Supporting external training and education for program leaders and key support staff (e.g., attendance at sepsis meetings and quality improvement trainings).
- Supporting internal training and education on sepsis for hospital staff and trainees.
- Supporting participation in regional, national, and international sepsis quality improvement collaboratives and initiatives.
Antibiotic stewardship and sepsis.
There have been some misperceptions that antibiotic stewardship may hinder efforts to improve management of sepsis. However, rather than hindering effective patient care, antibiotic stewardship programs can play an important role in optimizing the use of antibiotics, leading to better patient outcomes. It is possible for hospitals to make simultaneous improvement in sepsis management and antimicrobial stewardship.39
Accountability
Hospital sepsis programs should have one leader or two co-leaders who are accountable for program management and outcomes within the hospital or healthcare system. We strongly recommend sepsis programs be co-led by a physician and a nurse. Effective leadership, management, and communication skills, as well as clinical expertise in sepsis, are essential to success. Programs with co-leaders should have clear delineation of responsibilities and expectations. For health system-wide programs, physician and nurse champions or point-persons should be identified at each hospital, as local champions are consistently identified as key facilitators to successful quality improvement programs.38 In addition, hospital sepsis programs must set concrete goals to improve sepsis care and outcomes, monitor progress towards these goals, and revise goals at regular intervals.
Priority examples of accountability include:
- Identifying a single clinician leader or two co-leaders who will be responsible for sepsis program management and patient outcomes. We strongly recommend that sepsis programs be co-led by a physician and a nurse.
- Setting ambitious but achievable goals for improving sepsis care and patient outcomes that are informed by review of hospital practices, hospital sepsis outcomes, and clinical practice guidelines.
- Assessing progress towards hospital sepsis goals at regular intervals and updating goals periodically (e.g., annually) to promote continual improvement.
- Identifying a physician and nurse leader or champion at each hospital to ensure physician and nursing engagement in the sepsis program.
- In hospitals with a healthcare system-wide sepsis program, appoint a physician and nurse champion at each hospital.
- In hospitals with a single leader of the sepsis program, appoint a champion of the other discipline.
- In hospitals with a healthcare system-wide sepsis program, appoint a physician and nurse champion at each hospital.
Additional examples of accountability include:
- Including sepsis program-related activities and outcomes in annual performance reviews for sepsis program leaders.
- Identifying unit-level physician and nurse champions.
- Reporting sepsis program activities and outcomes to senior hospital leadership and/or board of directors on a regular basis (e.g., including sepsis measures in hospital quality dashboard reports).
Multi-Professional Expertise
Sepsis programs require engagement of multidisciplinary partners throughout the hospital, including clinicians and healthcare staff who support the care of patients with sepsis throughout the organization; individuals who facilitate performance evaluation and improvement activities (e.g., data analytics, information technology); and patients, family members, and caregivers who can provide insight into the experience of being hospitalized with and recovering from sepsis. Dedicated sepsis coordinators can greatly increase the effectiveness of the hospital sepsis program by contributing to action, tracking/reporting, and education activities.
Priority examples of multi-professional expertise include:
- Having a dedicated sepsis coordinator. Hospital sepsis coordinators oversee the day-to-day implementation of the sepsis program activities. The position can greatly enhance the impact of a hospital sepsis program. In many hospitals, a sepsis coordinator can serve as the sepsis program co-leader, but it can also be a separate position. Specific job duties for hospital sepsis coordinators vary, but often include reviewing sepsis cases in near real-time, providing feedback to staff regarding the reviewed cases, educating healthcare staff and trainees, identifying areas of focus for sepsis quality improvement initiatives, monitoring adherence to hospital sepsis protocols, and monitoring the impact of hospital sepsis initiatives. Depending on the size of the hospital, the sepsis coordinator role may be shared with other duties such serving on a rapid response team or as a coordinator for teams that oversee other time-sensitive conditions (e.g., stroke coordinator, trauma coordinator). Alternatively, hospitals with a high volume of sepsis hospitalizations are likely benefit from having multiple sepsis coordinators.
- Collaborating across hospital locations. Clinicians and leaders from the ED, inpatient wards, and intensive care units (ICUs) should be fully engaged in hospital sepsis program activities. Participation and collaboration across care locations is important to ensure coordination of sepsis care throughout the institution.
- Engaging multi-professional experts. In most hospitals, sepsis programs should include representation from antimicrobial stewardship, critical care, emergency medicine, hospital medicine, infectious diseases, nursing, other primary services (e.g., surgery, oncology, obstetrics, pediatrics), pharmacy, and social work. It is possible that a single individual may represent more than one group.
Engagement of the antibiotic stewardship program is critical to optimize the treatment of sepsis by ensuring antibiotic recommendations are based on local microbiology data, and that mechanisms are in place to review antibiotics started for suspected sepsis are tailored or stopped if unnecessary or treatment is complete.
- Engaging relevant support services. Hospital sepsis programs should have access to ongoing support from individuals with expertise and formal training in data management and analytics; information technology (e.g., individuals with expertise in implementing and revising electronic health records-based tools such as sepsis order sets); and quality improvement and patient safety (e.g., individuals with formal training in quality improvement processes such as the Institute for Healthcare Improvement's plan-do-study-act model40.)
Additional examples of multi-professional expertise include:
- Having availability of ad hoc domain expertise. Hospital sepsis programs should have at least ad hoc involvement of case management, microbiology, laboratory medicine, phlebotomy, outpatient clinicians, hospital epidemiologists, infection preventionists, patients, families, caregivers, and community members.
Action
The main goal of hospital sepsis programs is to improve the treatment and outcomes of patients with sepsis. To support this goal, sepsis programs should develop and implement structures and processes to facilitate recognition of sepsis, evidence-based management of sepsis, and longer-term recovery from sepsis. When designing and implementing interventions to improve sepsis management, it is important to use structured quality improvement processes and implementation science principles to promote uptake of the intervention.4142 Additionally, hospital sepsis programs should monitor use and effectiveness of hospital interventions and refine interventions as needed to optimize treatment and outcomes.
Priority examples of action include:
- Implementing a standardized process to screen for sepsis: Early administration of sepsis treatment is lifesaving, so it is important that clinicians recognize sepsis as early as possible.4344454647 To this end, hospitals should have a standardized process to screen at-risk patients for sepsis upon presentation to the hospital and throughout their hospitalization. Screening may use paper-based or electronic health record-based tools and may occur at standard recurring intervals (e.g., every 8-12 hours) and/or in response to clinical events (e.g., upon ICU transfer, upon clinical deterioration). Given the variety of clinical decision support systems in use and the low quality of studies evaluating their impact, the optimal approach to screening for sepsis remains unclear.2527 Indeed, the 2021 Surviving Sepsis Campaign Guidelines include a strong recommendation that hospital sepsis programs have a process to screen for sepsis, but do not recommend any specific tool or approach.1819 Regardless of the method chosen, screening for sepsis should be implemented according to user-centered design principles and should be tailored to the specific patient population served (e.g., adult, pediatric, obstetric). Screening should be integrated into clinical workflow in such a way that it enhances recognition of sepsis, while minimizing false-positive alarms and alarms on patients already recognized to have sepsis. Furthermore, newer, complex screening tools such as those using machine learning or artificial intelligence should be analyzed to ensure they do not project bias by patient race, ethnicity, gender, or other characteristics.
Examples of hospital screening tools are available on the Resources page.
- Developing and maintaining a hospital guideline or a standardized care pathway for management of sepsis: Hospital guidelines or standardized care pathways can greatly enhance the effectiveness of sepsis programs by establishing clear recommendations for care. Ideally, guidelines should address management across the continuum of hospital care including screening, clinical evaluation (e.g., recommended/suggested laboratory, microbiology, laboratory, or imaging studies), diagnosis, antimicrobial selection, source control, fluid resuscitation (e.g., indications, contraindications, type, and volume of fluid), indications for treatment escalation (e.g., admission to critical care unit), antimicrobial narrowing, antimicrobial stopping, patient and family/caregiver education on sepsis, and peri-discharge management. Recommendations should be based on published guidelines and generally accepted standards of care, but also take into consideration the available resources, local epidemiology, and patient population served (e.g., adult, pediatric, obstetric). For example, while international/national guidelines recommend prompt antimicrobials and source control, hospital guidelines can provide guidance on the selection of antimicrobials based on local resistance patterns and antimicrobial formulary options and guidance on approaching source control based on hospital availability of surgical and interventional radiology services. Empiric antimicrobial options should be recommended in conjunction with Antimicrobial Stewardship or Infectious Diseases staff. To ensure viability of hospital guidelines, they should be updated at least biannually and based on existing evidence-based sepsis guidelines.
Examples of hospital guidelines and/or clinical pathways addressing sepsis management are available on the Resources page.
- Hospital order sets for management of sepsis: Templated order sets can further aid in implementation of recommended practices for sepsis evaluation and management, including selection of antimicrobial therapy, timely delivery of the first dose of antimicrobials, clinical evaluation, source control, fluid resuscitation, antimicrobial narrowing, and antimicrobial stopping. Order sets should be tailored to the specific patient population (e.g., pediatric versus adult patients). As with hospital screening for sepsis, the content and scope of sepsis order sets may vary across hospitals, but they should always be developed with user-centered design principles. The easier it is to order appropriate sepsis evaluation and treatment, the more likely the order set will be used by clinicians.
- Structures and processes to facilitate prompt delivery of antimicrobials: Timely delivery of antimicrobial therapy in sepsis is life-saving.4344454647 In addition to facilitating prompt recognition of sepsis, hospitals should facilitate the prompt administration of initial antimicrobial therapy after the order for antimicrobial therapy has been placed.48 It has been estimated that one-third of the interval from patient presentation to antimicrobial delivery occurs after the antimicrobial order, and that post-order delays are associated with increased mortality.49 Furthermore, while there is concern that efforts to hasten recognition of sepsis and antimicrobial ordering may increase unnecessary antimicrobial prescribing, efforts to shorten time from antimicrobial order to delivery do not carry this risk. There are many processes that hospitals may use to shorten the time from antimicrobial order to antimicrobial delivery, including, but not limited, some examples below:48
- stocking of common antimicrobials in locations outside the pharmacy, such as in the ED, the ICU, and on hospital wards.
- immediate processing of new antimicrobial orders in patients with sepsis.
- clinician order entry systems that default to immediate administration of new antimicrobials (as opposed to the next standard medication administration time).
- pharmacists on-site in key locations outside the pharmacy, such as in the ED or ICU.
- stocking of common antimicrobials in locations outside the pharmacy, such as in the ED, the ICU, and on hospital wards.
- Structures and processes to support effective hospital hand-offs in patients with sepsis: Transfers between units (e.g., ED-to-ward, ward-to-ICU, and ICU-to-ward transfers), between treating clinicians (e.g., during physician and nursing shift changes), and between hospitals are high-risk times for information loss. Incomplete awareness of a patient's working diagnosis, uncertainty regarding the diagnosis, and/or treatment-to-date contribute to lapses in the delivery of subsequent care. For example, delays in first-to-second antimicrobial dose in sepsis are common and are associated with worse outcomes.5051 Structured communication processes to hand-off key information during transitions of care are consistently associated with reduced errors and improved outcomes. Hospitals should prioritize these procedures, such as templated notes to document sepsis diagnosis and treatment information, to help ensure effective transitions of care within the hospital. Hospitals should also have processes for safe patient transfer between healthcare facilities to continue the plan of care and facilitate infection control, akin to the inter-facility infection control transfer form.52
Additional examples of action include:
- Rapid response teams trained in sepsis recognition and care: Rapid response teams (also known as medical emergency teams) were first developed in the 1990s to bring needed expertise to the bedside of patients experiencing acute clinical deterioration. Sepsis rapid response teams are rapid response teams specifically focused on managing patients with sepsis.53 The teams are often multi-disciplinary, consisting of nurses, physicians, respiratory therapists, pharmacists, and phlebotomists. Implementation of sepsis-specific rapid response teams and training of general rapid response teams on the management of sepsis have been associated with improved care practices.54
- A "Code Sepsis" protocol: Many hospitals use "Code Sepsis" huddles to hasten sepsis recognition and treatment.58-60 "Code Sepsis" is activated by clinical staff based on suspicion of sepsis, often in response to vital signs and chief complaint upon presentation to the ED. Code sepsis activation triggers a multi-disciplinary team huddle (e.g., physician or physician assistant, primary nurse, ED pharmacist, and ED charge nurse) at the patient's bedside for evaluation of the clinical scenario and initiation of expedited early sepsis treatment (e.g., cultures, lactate measurement, imaging, antimicrobials, fluid) if indicated. Implementation of a code sepsis protocol has been associated with increased recognition of sepsis and faster delivery of initial treatment.555657 At the same time, some studies have suggested that "Code Sepsis" may also increase delivery of antimicrobials to patients who ultimately turn out to have non-infectious or non-bacterial causes, particularly "Code Sepsis" protocols based on the prior systemic inflammatory response syndrome (SIRS)-based sepsis definition.5859 A large, multi-hospital study showed that it is feasible to shorten time-to-antibiotics among patients with sepsis while simultaneously improving antimicrobial stewardship among patients at-risk for sepsis.39 However, it is still possible that efforts to hasten sepsis treatment may increase unnecessary antimicrobial. Definitive confirmation of infection is rarely possible in real-time, so decisions to initiate antimicrobial therapy must often precede confirmation of infection.60 Given these challenges, "Code Sepsis" protocols must be designed carefully, should include iterative reassessment with stopping of antimicrobials if an alternative non-infection-related diagnosis is found, and should be evaluated to understand their impact.
- Peri-discharge evaluation: Survivors of hospitalization for sepsis may experience new or worsening functional limitations, cognitive impairment, post-traumatic stress disorder (PTSD)/anxiety symptoms, and chronic health conditions.7 Up to 40% of patients are re-hospitalized within three months of discharge. Common causes for re-hospitalization include recurrent infection, heart failure exacerbation, chronic obstructive pulmonary disease (COPD) exacerbation, acute renal failure, and aspiration pneumonitis. Some of these hospitalizations may be preventable with optimal medical management.61 The following practices are recommended to support recovery from sepsis:71819
- screening for new/worsening difficulty completing activities and instrumental activities of daily living (I/ADLs).
- referring patients with new I/ADL limitations to appropriate supports (e.g., physical or occupational therapy).
- screening for swallowing dysfunction in at-risk patients and referral to speech therapy as needed.
- review of chronic conditions to ensure optimal medical management of chronic conditions and dose-optimization in response to physiologic changes as a result of sepsis (e.g., changes to renal function, blood pressure, weight).
- medication reconciliation and optimization, including a review of planned outpatient parenteral antimicrobial therapy (OPAT) if indicated and review of medical management of heart failure and COPD (which are common causes of readmission after sepsis).
- screening for social vulnerability (e.g., food and housing instability) and referral to available resources as needed.
- screening for new/worsening difficulty completing activities and instrumental activities of daily living (I/ADLs).
- Post-discharge care coordination and anticipatory guidance: The weeks and months after discharge from sepsis hospitalization are a period of heightened vulnerability to clinical deterioration and hospital readmission. To optimize recovery from sepsis, it is important to convey the ongoing care plan to the patient, involved family and caregivers, and the patient's outpatient clinician(s). When discharging a patient from the hospital, optimal practices to support recovery include:
- communicating the diagnosis of sepsis and ongoing care plan to the patient's primary care provider.
- providing contact information for clinical staff at the hospital to address post-discharge questions and/or troubleshoot post-discharge issues.
- contacting patient within two days of discharge by clinical staff to follow up on discharge instructions, symptoms, and/or issues.
- ensuring that patient, family, or caregivers are aware of times and indications for any follow-up visits and tests.
- reviewing patient's medication list to ensure that patient, family, or caregiver are aware of the (1) indication for each medication, (2) any changes to the medication regimen during hospitalization, and (3) any anticipated changes to the medication regimen in the following weeks.
- discussing the diagnosis of sepsis with the patient, family, or caregiver, including signs/symptoms of sepsis, indications to seek evaluation for potential sepsis, and any infection prevention measures that should be followed post-discharge. Sepsis education may be provided by healthcare staff, written educational material, and/or pre-recorded video material.
- discussing the potential effect of sepsis on cognitive, social, and emotional wellbeing, including fatigue and anxiety. Provide information on available support services.
- streamlining post-hospital care to the extent possible by scheduling follow-up visits and testing prior to discharge, consolidating visits and tests to single day where possible and preferred.
- communicating the diagnosis of sepsis and ongoing care plan to the patient's primary care provider.
- Prevention of healthcare-associated infections and hospital-onset sepsis: Hospitals that follow facility-based infection prevention recommendations through use of infection prevention teams may prevent acquisition of infections that lead to sepsis acquired in the healthcare setting62. Infection prevention teams that regularly audit provider understanding of hand hygiene and competency-based indwelling device insertion and monitoring bundles have been associated with reductions in healthcare-associated infections, which may include infections from multi-drug resistant pathogens that are difficult to treat.6364
Tracking
Tracking of sepsis epidemiology, management, and outcomes is critical for identifying gaps, trends, and improvement opportunities, as well as for understanding the impact of hospital-based sepsis interventions and progress towards hospital sepsis goals. However, tracking requires resources, and no program can measure everything. Before tracking sepsis metrics, it is important to prioritize what to measure, focusing on the processes and outcomes that are most important to patients and anticipated to represent the greatest opportunity for improvement in the hospital. Hospital sepsis programs may consider collaborating with hospital infection control programs, which measure healthcare-associated infections that may contribute to hospital-onset sepsis. When tracking sepsis measures, it is important to consider special patient populations (such as neonatal, pediatric, obstetric, oncology, transplant) and patient demographic groups to assess for disparities in sepsis management and outcomes.
Defining and Counting Sepsis Hospitalizations
While sepsis has been broadly defined as "life-threatening organ dysfunction caused by a dysregulated host response to infection", different approaches are needed to identify sepsis hospitalizations depending on the setting and patient population (e.g., neonatal, pediatric, maternal, adult)65666768697071. Sepsis programs must also carefully consider how to best define sepsis for the intended purpose, which may include clinical care, research, surveillance, quality improvement, and audit.6572
For example, diagnostic codes may be readily accessible and reflect individual clinical judgments. However, use of diagnostic codes may also be subject to provider, hospital, and temporal variation in coding practices.73747576 Furthermore, sepsis quality improvement initiatives that raise provider awareness can lead to stage migration by including more patients with milder disease, thus lower perceived sepsis mortality.747778
Definitions that use objective clinical data, such as the CDC Adult Sepsis Event (CDC ASE) criteria, can be used to benchmark sepsis quality improvement initiatives that require a consistent measure that can be extracted from data available in electronic health records.7980 However, the CDC ASE approach is retrospective in nature and not intended to guide diagnostic or clinical decision making. Furthermore, implementation of CDC ASE may be challenging depending on available information technology resources.
A sepsis program's decisions on how to define and count sepsis will depend on the intended audience (e.g., clinicians, quality improvement, hospital administration, payors), intended uses, and available resources. Thus, a hospital sepsis program may use diagnostic codes for monitoring clinical care processes, but then use objective criteria such as the CDC ASE to evaluate outcomes of a new quality improvement initiative.
Finally, methods for defining and counting sepsis are likely to continue to evolve over time. In this dynamic environment, hospital sepsis programs should be empowered to leverage the definitions of sepsis that will best provide the insights needed to improve patient care and outcomes.
Categories of tracking include:
- Sepsis epidemiology metrics, such as hospital sepsis case volume and break-down of community-onset vs hospital-onset sepsis, are important to understanding hospital sepsis case-mix. Example sepsis epidemiology metrics are provided in the table.
- Sepsis management metrics, such as antimicrobial timing and fluid administration, and important to understanding hospital processes of care for managing sepsis. Examples sepsis management metrics are provided in the Table.
- Sepsis outcomes metrics, such as mortality, ICU admission, and length of hospitalization, are important to understanding the outcomes of hospital sepsis management. Examples sepsis outcome metrics are provided in the Table.
- Progress towards achieving sepsis program goals. Hospital sepsis program goals may focus on management or outcomes of sepsis, and it is important to track these metrics over time to evaluate the impact of the hospital sepsis program and to update hospital sepsis program goals to drive continual improvement.
- Use, usability, and impact of sepsis program tools. To understand and improve the impact of hospital sepsis program tools (e.g., guidelines, triage algorithms, order sets, clinical decision support), it is important to assess how often they are being used, how acceptable they are to front-line clinicians, and the extent to which they are informing practice. Examples metrics are provided in the Table.
- Chart reviews of sepsis hospitalizations. Beyond tracking sepsis epidemiology, management, and outcome metrics, chart review of sepsis hospitalizations is helpful for clinician feedback, education, root cause analyses of adverse outcomes, and process. Chart review, which is often done by the sepsis coordinator, is resource intensive. Therefore, hospitals may review a random sample of sepsis hospitalizations, or a targeted sample (e.g., over-sampling of hospitalizations with adverse outcomes).
Table: Examples of tracking sepsis epidemiology, management, and outcomes
| Category | Priority | Concept | Example |
|---|---|---|---|
| Sepsis epidemiology | Priority | Community-onset sepsis | Numerator: Hospitalizations meeting criteria for sepsis within 48 hours of arrival to hospital or emergency department Denominator: All hospitalizations not admitted through inter-hospital transfer |
| Sepsis epidemiology | Priority | Hospital-onset sepsis | Numerator: Hospitalizations meeting criteria for sepsis after 48 hours of arrival to hospital or emergency department Denominator: All hospitalizations |
| Sepsis epidemiology | Priority | Sepsis (without shock) | Numerator: Hospitalizations meeting criteria for sepsis without shock Denominator: All hospitalizations |
| Sepsis epidemiology | Priority | Septic shock | Numerator: Hospitalizations meeting criteria for sepsis and criteria for shock Denominator: All hospitalizations |
| Sepsis epidemiology | Additional | Sepsis transfers out | Numerator: All hospitalizations meeting criteria for sepsis whose hospital discharge disposition was to another acute care hospital Denominator: Al hospitalizations meeting criteria for sepsis |
| Sepsis epidemiology | Additional | Sepsis transfers in | Numerator: All hospitalizations meeting criteria for sepsis who were admitted as an inter-hospital transfer Denominator: Al hospitalizations meeting criteria for sepsis |
| Sepsis epidemiology | Additional | Community-onset sepsis in special population(s) | Numerator: Hospitalizations among special population meeting criteria for sepsis within 48 hours of arrival to hospital or emergency department Denominator: All hospitalizations among special population (e.g., neonatal, pediatric, obstetric, oncology, transplant) |
| Sepsis epidemiology | Additional | Hospital-onset sepsis in special population(s) | Numerator: Hospitalizations meeting criteria for sepsis after 48 hours of arrival to hospital or emergency department Denominator: All hospitalizations among special population (e.g., neonatal, pediatric, obstetric, oncology, transplant) |
| Sepsis epidemiology | Additional | Sepsis site(s) of infection | Numerator: Hospitalizations meeting criteria for sepsis with a specific site of infection (e.g., pneumonia, genitourinary, gastrointestinal, neurologic, skin/soft tissue, bacteremia, endocarditis, etc.) Denominator: Hospitalizations meeting criteria for sepsis |
| Sepsis epidemiology | Additional | Sepsis pathogen(s) | Numerator: Hospitalizations meeting criteria for sepsis with a specific pathogen identified (e.g., staph aureus, MRSA, etc.) <Denominator: Hospitalizations meeting criteria for sepsis |
| Sepsis epidemiology | Additional | Surgical sepsis | Numerator: Hospitalizations meeting criteria for sepsis with a surgical or interventional procedure for source control Denominator: Hospitalizations meeting criteria for sepsis |
| Sepsis management | Priority | Time-to-antimicrobial in community-onset sepsis with hypotension | Measure: Time from emergency department or hospital arrival to time of administration of systemic antimicrobial therapy Eligibility: Hospitalizations meeting criteria for community onset sepsis, with evidence of hypotension on presentation (e.g., SBP<90, MAP<65, or initiated on systemic vasopressor therapy), without a viral cause of infection (e.g., influenza, COVID-19), and without intravenous antimicrobial therapy prior to hospital arrival. |
| Sepsis management | Priority | Time from antibiotic order to administration | Measure: Time from emergency department or hospital arrival to time of administration of systemic antimicrobial therapy Eligibility: Hospitalizations meeting criteria for community onset sepsis, with evidence of hypotension on presentation (e.g., SBP<90, MAP<65, or initiated on systemic vasopressor therapy), without a viral cause of infection (e.g., influenza, COVID-19), and without intravenous antimicrobial therapy prior to hospital arrival. |
| Sepsis management | Additional | Antimicrobial selection | Measure: Time from first antimicrobial order to first administration of systemic antimicrobial therapy Eligibility: Hospitalizations meeting criteria for sepsis and not admitted as an inter-hospital transfer and not on intravenous antimicrobial therapy prior to arrival |
| Sepsis management | Additional | Lactate measurement | Numerator: Hospitalizations whose initial antimicrobial therapy selection was consistent with institutional guidelines Denominator: Hospitalizations meeting criteria for sepsis and initiated on systemic antimicrobial therapy |
| Sepsis management | Additional | Lactate remeasurement | Numerator: Hospitalizations with a lactate measurement within 3 hours of arrival in community-onset sepsis or 3 hours of onset of hospital-onset sepsis Denominator: Hospitalizations meeting criteria for sepsis |
| Sepsis management | Additional | Blood culture prior to antimicrobial initiation | Numerator: Hospitalizations with a lactate collected within 4 hours of the collection of the first lactate measurement ≥2 mmol/L | Denominator: Hospitalizations meeting criteria for sepsis and with a lactate measurement ≥2 mmol/L |
| Sepsis management | Additional | Fluid resuscitation | Numerator: Hospitalizations receiving ≥30 ml/kg crystalloid fluid within 6 hours of evidence of low blood pressure and/or elevated lactate Denominator: Hospitalizations meeting criteria for sepsis, with low blood pressure (e.g., SBP<90, MAP<65, or initiated on vasopressor therapy) and/or elevated lactate (≥2-4 mmol/L), and without contraindications to fluid administration (e.g., excluding patients with severely reduced cardiac function, end-stage renal disease, or evidence of fluid overload) |
| Sepsis management | Additional | Fluid type | Numerator: ≥75% of crystalloid fluid resuscitation provided as a balanced solution (e.g., lactated ringers) Denominator: Hospitalizations meeting criteria for sepsis and treated with crystalloid fluid for sepsis-induced hypotension or lactate elevation |
| Sepsis management | Additional | Antimicrobial narrowing | Numerator: Hospitalizations with anti-MRSA treatment stopped within 3 calendar days of initiation Denominator: Hospitalizations meeting criteria for sepsis, initiated on anti-MRSA antimicrobial treatment, and with no MRSA identified in culture or microbial testing |
| Sepsis management | Additional | Blood culture contamination [PDF - 3 Pages] | Numerator: Number of blood culture sets with growth of skin commensals without the same organism in other sets collected within 24hrs Denominator: Total number of all eligible blood culture sets collected |
| Sepsis management | Additional | Single Blood Culture | Numerator: Number of single blood culture sets collected among adult patients Denominator: Total number of all blood culture sets collected among adults |
| Sepsis management | Additional | Sepsis documentation | Numerator: Hospitalizations with specific aspects of sepsis diagnosis and management documented during transitions of care (e.g., certainty of sepsis diagnosis, antimicrobial therapy plan) Denominator: Hospitalizations with a transition of care (e.g., ED-to-ward; ICU-to-ward transfer) |
| Sepsis management | Additional | Timely post-hospital follow-up visit | Numerator: Hospitalizations with a primary care follow-up visit scheduled prior to discharge, to occur within 14 days of discharge Denominator: Hospitalizations meeting criteria for sepsis, discharged to home or assisted living |
| Sepsis management | Additional | Post-hospital follow-up call | Numerator: Hospitalizations with post-discharge follow-up call attempted within 3 calendar days of discharge Denominator: Hospitalizations meeting criteria for sepsis, discharged to home or assisted living |
| Sepsis management | Additional | Functional assessment | Numerator: Hospitalizations with a functional assessment at admission and discharge (e.g., assessment ability to bathe, dress, toilet, transfer, walk, and manage medications independently) Denominator: Hospitalizations meeting criteria for sepsis |
| Sepsis outcomes | Priority | In-hospital mortality, overall | Numerator: Hospitalizations meeting criteria for sepsis and with in-hospital mortality Denominator: All hospitalizations meeting criteria for sepsis |
| Sepsis outcomes | Priority | In-hospital mortality, subgroup | Numerator: Hospitalizations meeting criteria for subgroup (e.g., community-onset sepsis, hospital-onset sepsis, septic shock, sepsis without shock, etc.) and with in-hospital mortality Denominator: All hospitalizations meeting criteria for sepsis and the subgroup of interest |
| Sepsis outcomes | Additional | 30-day mortality | Numerator: Hospitalizations with sepsis who are alive at 30 days from the date of hospital admission Denominator: All hospitalizations meeting criteria for sepsis |
| Sepsis outcomes | Additional | 90-day mortality | Numerator: Hospitalizations with sepsis who are alive at 90 days from the date of hospital admission Denominator: All hospitalizations meeting criteria for sepsis |
| Sepsis outcomes | Additional | Post-discharge mortality | Numerator: Death within 90 days of discharge from hospitalization with sepsis Denominator: All hospitalizations meeting criteria for sepsis with live discharge |
| Sepsis outcomes | Additional | Discharge to hospice | Numerator: Hospitalizations with sepsis who were discharge to inpatient or home hospice Denominator: All hospitalizations meeting criteria for sepsis |
| Sepsis outcomes | Additional | ICU admission | Numerator: Hospitalizations in which the patient was admitted to the ICU Denominator: All hospitalizations meeting criteria for sepsis |
| Sepsis outcomes | Additional | In-hospital mortality, special populations | Numerator: Hospitalizations meeting criteria for subgroup (e.g., neonatal, pediatric, maternal, oncologic, transplant, etc.) and with in-hospital mortality Denominator: All hospitalizations meeting criteria for sepsis and the special population of interest |
| Sepsis outcomes | Additional | Length of hospitalization, survivors | Measure: Length of hospitalization in days Eligibility: All hospitalizations meeting criteria for sepsis and with live discharge to a location other than an acute care hospital |
| Sepsis outcomes | Additional | Length of hospitalization, non-survivors | Measure: Length of hospitalization in days Eligibility: All hospitalizations meeting criteria for sepsis and with in-hospital mortality |
| Sepsis outcomes | Additional | New discharge to a healthcare or nursing facility | Numerator: Hospitalizations in which the patient is discharge to a long-term acute care facility, skilled nursing facility, or custodial nursing facility. Denominator: All hospitalizations meeting criteria for sepsis, with live discharge, and in which the patient did not reside at home or in assisted living prior to hospital admission |
| Usability of hospital sepsis tools | Priority | Use of hospital sepsis order set | Numerator: Hospitalizations in which the sepsis order set was used Denominator: All hospitalizations meeting criteria for sepsis |
| Usability of hospital sepsis tools | Additional | Use of hospital sepsis decision-support | Numerator: Specific response of the clinician receiving the sepsis alert (e.g., snooze, ignore, change in clinical management) Denominator: Sepsis alert notification |
Reporting
Reporting of sepsis treatment and outcomes to relevant staff can help maintain staff engagement, motivate behavior change, and facilitate improvement in sepsis treatment and outcomes. It is critical that information be provided in a clear and transparent manner. Reports should explain how data were collected and how measures were calculated. In addition, providing the option to "drill down" and review data for individual hospitalizations can be help facilitate targeted review of cases for performance improvement. Data that are timely and focused (e.g., to a specific hospital unit or an individual clinician) are often most actionable.81 Reports to hospital leadership and the board can also help raise awareness of and support for sepsis program efforts.
Examples of reporting include:
- Priority examples:
- Regular reports to hospital, unit, and clinical leadership: It is important to report sepsis treatment and outcome data to nursing, physician, unit-based, and hospital leadership at routine intervals (e.g., monthly or quarterly). The following data are particularly helpful for engaging clinical leadership:
- Unit-level data
- Trends over time
- Comparative or benchmarking data (e.g., comparison to other similar units or hospitals)
- Unit-level data
- Additional examples:
- Focused feedback to individual clinicians. Timely feedback on the management of specific patients with sepsis can be extremely effective at re-enforcing desired behaviors and providing targeted education on any areas where care lagged. In many hospitals, sepsis coordinators review cases in near real time and provide direct feedback to involved clinicians—both positive feedback for good care and constructive feedback for any areas where care could have been improved. Public recognition of excellent sepsis care (e.g., through department emails, recognition pins) may further engage and motivate clinicians.
- Live Sepsis Dashboard. Development and maintenance of a sepsis dashboard that is updated in real time can provide continuous information to nursing, physician, and unit-based leadership.
- Focused feedback to individual clinicians. Timely feedback on the management of specific patients with sepsis can be extremely effective at re-enforcing desired behaviors and providing targeted education on any areas where care lagged. In many hospitals, sepsis coordinators review cases in near real time and provide direct feedback to involved clinicians—both positive feedback for good care and constructive feedback for any areas where care could have been improved. Public recognition of excellent sepsis care (e.g., through department emails, recognition pins) may further engage and motivate clinicians.
Education
For optimal sepsis treatment and outcomes, it is imperative that hospital staff have strong knowledge of sepsis and understand their role in team-based management of sepsis. Educational efforts should be focused on all healthcare workers involved in sepsis care, all patient-facing staff, and all health profession trainees. There are many methods of providing education to hospital staff, including simulation or case-based training; in-person or video-recorded lectures; flyers or posters; and email or newsletters. The optimal approach to education may vary by audience.
Knowledge of sepsis is also important to patients, families, and caregivers. Patients hospitalized for sepsis are at increased risk for subsequent episodes of sepsis.6182 However, despite the increased risk for recurrent sepsis, many patients are unaware of both their diagnosis of sepsis and their risk for recurrent sepsis.83 In an international survey of sepsis survivors, nearly half reported dissatisfaction with sepsis education.84 Hospitalization and post-hospital follow-up are a key opportunity to educate patients and families on sepsis, when to suspect sepsis, and when to seek evaluation for potential sepsis. The Surviving Sepsis Campaign guidelines suggest offering both verbal and written sepsis education prior to hospital discharge and in the follow-up setting, particularly since education may facilitate timely health-seeking behavior in sepsis survivors who experience complications.1819
Educational resources for healthcare professional, patients, families, and caregivers are available on the Materials for Patients page and the Materials for Healthcare Providers page.
Examples of sepsis education include:
- Priority examples:
- Including sepsis-specific training and education in the hiring or on-boarding process for healthcare staff and trainees
- Providing annual sepsis education to clinical staff
- Providing written and verbal education on sepsis to patients, families, and/or caregivers prior to hospital discharge
- Including sepsis-specific training and education in the hiring or on-boarding process for healthcare staff and trainees
- Additional examples:
- Posting information on recognition of sepsis in prominent areas for patient-facing staff (e.g., attached to vital sign machines, in staff beak rooms)
- Holding hospital lectures (e.g., grand rounds) or an annual meeting focused on sepsis
- Including sepsis recognition and treatment in annual nursing competencies.
- Posting information on recognition of sepsis in prominent areas for patient-facing staff (e.g., attached to vital sign machines, in staff beak rooms)
CDC Efforts to Support Sepsis Care
The Hospital Sepsis Program Core Elements is one of several initiatives to help improve awareness, management, and outcomes of sepsis.
- Singer M, Deutschman CS, Seymour CW, et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA. Feb 23 2016;315(8):801-10. doi:10.1001/jama.2016.0287
- Rudd KE, Johnson SC, Agesa KM, et al. Global, regional, and national sepsis incidence and mortality, 1990-2017: analysis for the Global Burden of Disease Study. Lancet. Jan 18 2020;395(10219):200-211. doi:10.1016/S0140-6736(19)32989-7
- Liu V, Escobar GJ, Greene JD, et al. Hospital deaths in patients with sepsis from 2 independent cohorts. JAMA. Jul 2 2014;312(1):90-2. doi:10.1001/jama.2014.5804
- Rhee C, Jones TM, Hamad Y, et al. Prevalence, Underlying Causes, and Preventability of Sepsis-Associated Mortality in US Acute Care Hospitals. JAMA Netw Open. Feb 1 2019;2(2):e187571. doi:10.1001/jamanetworkopen.2018.7571
- CDC. What is sepsis? Available at https://www.cdc.gov/sepsis/what-is-sepsis.html (accessed January 23, 2023).
- Iwashyna TJ, Ely EW, Smith DM, Langa KM. Long-term cognitive impairment and functional disability among survivors of severe sepsis. Research Support, N.I.H., ExtramuralResearch Support, Non-U.S. Gov'tResearch Support, U.S. Gov't, Non-P.H.S. JAMA. Oct 27 2010;304(16):1787-94. doi:10.1001/jama.2010.1553
- Prescott HC, Angus DC. Enhancing Recovery From Sepsis. JAMA. 2018;319(1):62-75. doi:10.1001/jama.2017.17687
- Prescott HC, Osterholzer JJ, Langa KM, Angus DC, Iwashyna TJ. Late mortality after sepsis: Propensity matched cohort study. BMJ (Online). 2016;353:i2375. doi:10.1136/bmj.i2375
- Carlton EF, Gebremariam A, Maddux AB, et al. New and Progressive Medical Conditions After Pediatric Sepsis Hospitalization Requiring Critical Care. JAMA Pediatr. Nov 1 2022;176(11):e223554. doi:10.1001/jamapediatrics.2022.3554
- Reinhart K, Daniels R, Kissoon N, Machado FR, Schachter RD, Finfer S. Recognizing Sepsis as a Global Health Priority – A WHO Resolution. The New England Journal of Medicine. 2017;377(5):414-417. doi:10.1056/NEJMp1707170
- Sepsis Alliance. Disparities in Sepsis Awareness Highlighted in 2022 Survey. Available at https://www.sepsis.org/news/disparities-in-sepsis-awareness-highlighted-in-2022-survey/ (Accessed February 20, 2023).
- Dellinger RP, Carlet JM, Masur H, et al. Surviving Sepsis Campaign guidelines for management of severe sepsis and septic shock. Crit Care Med. Mar 2004;32(3):858-73. doi:10.1097/01.ccm.0000117317.18092.e4
- Dellinger RP, Rhodes A, Evans L, et al. Surviving Sepsis Campaign. Crit Care Med. Apr 1 2023;51(4):431-444. doi:10.1097/CCM.0000000000005804
- Weiss SL, Peters MJ, Alhazzani W, et al. Surviving Sepsis Campaign International Guidelines for the Management of Septic Shock and Sepsis-Associated Organ Dysfunction in Children. Pediatr Crit Care Med. Feb 2020;21(2):e52-e106. doi:10.1097/PCC.0000000000002198
- Weiss SL, Peters MJ, Alhazzani W, et al. Surviving sepsis campaign international guidelines for the management of septic shock and sepsis-associated organ dysfunction in children. Intensive Care Med. Feb 2020;46(Suppl 1):10-67. doi:10.1007/s00134-019-05878-6
- Evans L, Rhodes A, Alhazzani W, et al. Executive Summary: Surviving Sepsis Campaign: International Guidelines for the Management of Sepsis and Septic Shock 2021. Crit Care Med. Nov 1 2021;49(11):1974-1982. doi:10.1097/CCM.0000000000005357
- Schunemann HJ, Wiercioch W, Brozek J, et al. GRADE Evidence to Decision (EtD) frameworks for adoption, adaptation, and de novo development of trustworthy recommendations: GRADE-ADOLOPMENT. J Clin Epidemiol. Jan 2017;81:101-110. doi:10.1016/j.jclinepi.2016.09.009
- Evans L, Rhodes A, Alhazzani W, et al. Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock 2021. Crit Care Med. Nov 1 2021;49(11):e1063-e1143. doi:10.1097/CCM.0000000000005337
- Evans L, Rhodes A, Alhazzani W, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock 2021. Intensive Care Med. Oct 2 2021;doi:10.1007/s00134-021-06506-y
- Ferrer R, Artigas A, Levy MM, et al. Improvement in process of care and outcome after a multicenter severe sepsis educational program in Spain. JAMA. May 21 2008;299(19):2294-303. doi:10.1001/jama.299.19.2294
- Levy MM, Dellinger RP, Townsend SR, et al. The Surviving Sepsis Campaign: results of an international guideline-based performance improvement program targeting severe sepsis. Intensive care medicine. 2010;36:222-31. doi:10.1007/s00134-009-1738-3
- van Zanten AR, Brinkman S, Arbous MS, et al. Guideline bundles adherence and mortality in severe sepsis and septic shock. Crit Care Med. Aug 2014;42(8):1890-8. doi:10.1097/CCM.0000000000000297
- Levy MM, Gesten FC, Phillips GS, et al. Mortality Changes Associated with Mandated Public Reporting for Sepsis. The Results of the New York State Initiative. Am J Respir Crit Care Med. Dec 1 2018;198(11):1406-1412. doi:10.1164/rccm.201712-2545OC
- Kahn JM, Davis BS, Yabes JG, et al. Association Between State-Mandated Protocolized Sepsis Care and In-hospital Mortality Among Adults With Sepsis. JAMA. Jul 16 2019;322(3):240-250. doi:10.1001/jama.2019.9021
- Ackermann K, Baker J, Green M, et al. Computerized Clinical Decision Support Systems for the Early Detection of Sepsis Among Adult Inpatients: Scoping Review. J Med Internet Res. Feb 23 2022;24(2):e31083. doi:10.2196/31083
- Makam AN, Nguyen OK, Auerbach AD. Diagnostic accuracy and effectiveness of automated electronic sepsis alert systems: A systematic review. Journal of hospital medicine : an official publication of the Society of Hospital Medicine. Jun 2015;10(6):396-402. doi:10.1002/jhm.2347
- Warttig S, Alderson P, Evans DJ, Lewis SR, Kourbeti IS, Smith AF. Automated monitoring compared to standard care for the early detection of sepsis in critically ill patients. Cochrane Database Syst Rev. Jun 25 2018;6:CD012404. doi:10.1002/14651858.CD012404.pub2
- Manaktala S, Claypool SR. Evaluating the impact of a computerized surveillance algorithm and decision support system on sepsis mortality. Journal of the American Medical Informatics Association : JAMIA. Jan 2017;24(1):88-95. doi:10.1093/jamia/ocw056
- Burdick H, Pino E, Gabel-Comeau D, et al. Effect of a sepsis prediction algorithm on patient mortality, length of stay and readmission: a prospective multicentre clinical outcomes evaluation of real-world patient data from US hospitals. BMJ Health Care Inform. Apr 2020;27(1)doi:10.1136/bmjhci-2019-100109
- Adams R, Henry KE, Sridharan A, et al. Prospective, multi-site study of patient outcomes after implementation of the TREWS machine learning-based early warning system for sepsis. Nature medicine. Jul 2022;28(7):1455-1460. doi:10.1038/s41591-022-01894-0
- Shimabukuro DW, Barton CW, Feldman MD, Mataraso SJ, Das R. Effect of a machine learning-based severe sepsis prediction algorithm on patient survival and hospital length of stay: a randomised clinical trial. BMJ Open Respir Res. 2017;4(1):e000234. doi:10.1136/bmjresp-2017-000234
- Tarrant C, O'Donnell B, Martin G, Bion J, Hunter A, Rooney KD. A complex endeavour: an ethnographic study of the implementation of the Sepsis Six clinical care bundle. Implementation science : IS. Nov 16 2016;11(1):149. doi:10.1186/s13012-016-0518-z
- Steinmo SH, Michie S, Fuller C, Stanley S, Stapleton C, Stone SP. Bridging the gap between pragmatic intervention design and theory: using behavioural science tools to modify an existing quality improvement programme to implement "Sepsis Six". Implementation science : IS. Feb 3 2016;11:14. doi:10.1186/s13012-016-0376-8
- American College of Emergency Physicians. DaRT Guide. Available at https://www.acep.org/patient-care/dart/ (accessed January 23, 2023).
- California Maternal Quality Care Collaborative. Improving Diagnosis and Treatment of Maternal Sepsis; A CMQCC Quality Improvement Toolkit Available at https://www.cmqcc.org/sites/default/files/Sepsis%20Toolkit_FINAL.2_Errata_7.1.22.pdf [PDF – 67 Pages] (accessed April 5, 2023).
- Damiani E, Donati A, Serafini G, et al. Effect of performance improvement programs on compliance with sepsis bundles and mortality: a systematic review and meta-analysis of observational studies. PloS one. 2015;10(5):e0125827. doi:10.1371/journal.pone.0125827
- Weiner BJ, Shortell SM, Alexander J. Promoting clinical involvement in hospital quality improvement efforts: the effects of top management, board, and physician leadership. Health Serv Res. Oct 1997;32(4):491-510.
- Zoutman DE, Ford BD. Quality improvement in hospitals: barriers and facilitators. Int J Health Care Qual Assur. Feb 13 2017;30(1):16-24. doi:10.1108/IJHCQA-12-2015-0144
- Prescott HC, Seelye S, Wang XQ, et al. Temporal Trends in Antimicrobial Prescribing During Hospitalization for Potential Infection and Sepsis. JAMA Intern Med. Aug 1 2022;182(8):805-813. doi:10.1001/jamainternmed.2022.2291
- Berwick DM. Developing and testing changes in delivery of care. Ann Intern Med. Apr 15 1998;128(8):651-6. doi:10.7326/0003-4819-128-8-199804150-00009
- Jones B, Vaux E, Olsson-Brown A. How to get started in quality improvement. BMJ. Jan 17 2019;364:k5408. doi:10.1136/bmj.k5437
- Bauer MS, Damschroder L, Hagedorn H, Smith J, Kilbourne AM. An introduction to implementation science for the non-specialist. BMC Psychol. Sep 16 2015;3(1):32. doi:10.1186/s40359-015-0089-9
- Liu VX, Fielding-Singh V, Greene JD, et al. The Timing of Early Antibiotics and Hospital Mortality in Sepsis. Am J Respir Crit Care Med. Oct 1 2017;196(7):856-863. doi:10.1164/rccm.201609-1848OC
- Seymour CW, Gesten F, Prescott HC, et al. Time to Treatment and Mortality during Mandated Emergency Care for Sepsis. N Engl J Med. Jun 8 2017;376(23):2235-2244. doi:10.1056/NEJMoa1703058
- Peltan ID, Brown SM, Bledsoe JR, et al. ED Door-to-Antibiotic Time and Long-term Mortality in Sepsis. Chest. May 2019;155(5):938-946. doi:10.1016/j.chest.2019.02.008
- Reitz KM, Kennedy J, Li SR, et al. Association Between Time to Source Control in Sepsis and 90-Day Mortality. JAMA Surg. Sep 1 2022;157(9):817-826. doi:10.1001/jamasurg.2022.2761
- Ruddel H, Thomas-Ruddel DO, Reinhart K, et al. Adverse effects of delayed antimicrobial treatment and surgical source control in adults with sepsis: results of a planned secondary analysis of a cluster-randomized controlled trial. Crit Care. Feb 28 2022;26(1):51. doi:10.1186/s13054-022-03901-9
- Klompas M, Rhee C. Antibiotic Order-to-Infusion Time for Patients With Septic Shock: A Potential New Quality Metric. Crit Care Med. Oct 2019;47(10):1467-1470. doi:10.1097/CCM.0000000000003940
- Kashiouris MG, Zemore Z, Kimball Z, et al. Supply Chain Delays in Antimicrobial Administration After the Initial Clinician Order and Mortality in Patients With Sepsis. Crit Care Med. Oct 2019;47(10):1388-1395. doi:10.1097/CCM.0000000000003921
- Taylor SP, Shah M, Kowalkowski MA, Taylor B, Chou SH. First-to-second antibiotic delay and hospital mortality among emergency department patients with suspected sepsis. Am J Emerg Med. Aug 2021;46:20-22. doi:10.1016/j.ajem.2021.02.059
- Harpenau TL, Bhatti SN, Hoffman BM, Kirsch WB. Impact of extended emergency department stay on antibiotic re-dosing delays and outcomes in sepsis. Am J Emerg Med. May 2022;55:32-37. doi:10.1016/j.ajem.2022.02.028
- US Centers for Disease Control and Prevention. Inter-Facility Infection Control Transfer Form for States Establishing HAI Prevention Collaboratives. Available at https://www.cdc.gov/hai/prevent/prevention_tools.html Accessed (Accessed February 7, 2023).
- Ju T, Al-Mashat M, Rivas L, Sarani B. Sepsis Rapid Response Teams. Crit Care Clin. Apr 2018;34(2):253-258. doi:10.1016/j.ccc.2017.12.004
- Dooley K, Guzik W, Rooker G, Beecher L, Hiniker C, Olson A. Improving hospital sepsis care using PAs and NPs on a rapid response team. JAAPA. Oct 1 2022;35(10):43-45. doi:10.1097/01.JAA.0000873808.41684.d3
- Currie KE, Barry H, Scanlan JM, Harvey EM. Impact of a multidisciplinary sepsis huddle in the emergency department. Am J Emerg Med. Feb 2023;64:150-154. doi:10.1016/j.ajem.2022.12.006
- Delawder JM, Hulton L. An Interdisciplinary Code Sepsis Team to Improve Sepsis-Bundle Compliance: A Quality Improvement Project. J Emerg Nurs. Jan 2020;46(1):91-98. doi:10.1016/j.jen.2019.07.001
- Whitfield PL, Ratliff PD, Lockhart LL, et al. Implementation of an adult code sepsis protocol and its impact on SEP-1 core measure perfect score attainment in the ED. Am J Emerg Med. May 2020;38(5):879-882. doi:10.1016/j.ajem.2019.07.002
- Kang M, Torriani FJ, Sell RE, Wardi G, Abeles SR. The Impact of an Inpatient Nurse-Triggered Sepsis Alert on Antimicrobial Utilization. Jt Comm J Qual Patient Saf. Mar 2021;47(3):157-164. doi:10.1016/j.jcjq.2020.11.004
- Taylor SP, Rozario N, Kowalkowski MA, et al. Trends in False-Positive Code Sepsis Activations in the Emergency Department. Annals of the American Thoracic Society. Apr 2020;17(4):520-522. doi:10.1513/AnnalsATS.201910-757RL
- Prescott HC, Iwashyna TJ. Improving Sepsis Treatment by Embracing Diagnostic Uncertainty. Annals of the American Thoracic Society. Apr 2019;16(4):426-429. doi:10.1513/AnnalsATS.201809-646PS
- Prescott HC, Langa KM, Iwashyna TJ. Readmission diagnoses after hospitalization for severe sepsis and other acute medical conditions. JAMA. Mar 10 2015;313(10):1055-7. doi:10.1001/jama.2015.1410
- US Centers for Disease Control and Prevention. Healthcare Infection Control Practices Advisory Committee (HICPAC) guidelines and publications. https://www.cdc.gov/infectioncontrol/guidelines/index.html. (Accessed February 7, 2023).
- Boyce JM, Pittet D, Healthcare Infection Control Practices Advisory C, Force HSAIHHT. Guideline for Hand Hygiene in Health-Care Settings. Recommendations of the Healthcare Infection Control Practices Advisory Committee and the HICPAC/SHEA/APIC/IDSA Hand Hygiene Task Force. Society for Healthcare Epidemiology of America/Association for Professionals in Infection Control/Infectious Diseases Society of America. MMWR Recomm Rep. Oct 25 2002;51(RR-16):1-45, quiz CE1-4.
- Pronovost P, Needham D, Berenholtz S, et al. An intervention to decrease catheter-related bloodstream infections in the ICU. N Engl J Med. Dec 28 2006;355(26):2725-32. doi:10.1056/NEJMoa061115
- Singer M, Deutschman CS, Seymour CW, et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA. 2016;315(8):801-810. doi:10.1001/jama.2016.0287
- Angus DC, Seymour CW, Coopersmith CM, et al. A Framework for the Development and Interpretation of Different Sepsis Definitions and Clinical Criteria. Critical care medicine. 2016;44:e113-21. doi:10.1097/CCM.0000000000001730
- Seymour CW, Liu VX, Iwashyna TJ, et al. Assessment of Clinical Criteria for Sepsis: For the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA. 2016;315(8):762-74. doi:10.1001/jama.2016.0288
- Shankar-Hari M, Phillips GS, Levy ML, et al. Developing a New Definition and Assessing New Clinical Criteria for Septic Shock: For the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA. Feb 23 2016;315(8):775-87. doi:10.1001/jama.2016.0289
- Carrol ED, Ranjit S, Menon K, et al. Operationalizing Appropriate Sepsis Definitions in Children Worldwide: Considerations for the Pediatric Sepsis Definition Taskforce. Pediatr Crit Care Med. Apr 25 2023;doi:10.1097/PCC.0000000000003263
- Bonet M, Nogueira Pileggi V, Rijken MJ, et al. Towards a consensus definition of maternal sepsis: results of a systematic review and expert consultation. Reprod Health. May 30 2017;14(1):67. doi:10.1186/s12978-017-0321-6
- Molloy EJ, Wynn JL, Bliss J, et al. Neonatal sepsis: need for consensus definition, collaboration and core outcomes. Pediatr Res. Jul 2020;88(1):2-4. doi:10.1038/s41390-020-0850-5
- Seymour CW, Coopersmith CM, Deutschman CS, et al. Application of a Framework to Assess the Usefulness of Alternative Sepsis Criteria. Critical care medicine. 2016;44:e122-30. doi:10.1097/CCM.0000000000001724
- Jafarzadeh SR, Thomas BS, Marschall J, Fraser VJ, Gill J, Warren DK. Quantifying the improvement in sepsis diagnosis, documentation, and coding: the marginal causal effect of year of hospitalization on sepsis diagnosis. Ann Epidemiol. Jan 2016;26(1):66-70. doi:10.1016/j.annepidem.2015.10.008
- Lindenauer PK, Lagu T, Shieh MS, Pekow PS, Rothberg MB. Association of diagnostic coding with trends in hospitalizations and mortality of patients with pneumonia, 2003-2009. JAMA. Apr 4 2012;307(13):1405-13. doi:10.1001/jama.2012.384
- Klompas M, Rhee C. Sepsis and the theory of relativity: measuring a moving target with a moving measuring stick. Crit Care. Nov 21 2016;20(1):396. doi:10.1186/s13054-016-1559-z
- Gaieski DF, Edwards JM, Kallan MJ, Carr BG. Benchmarking the incidence and mortality of severe sepsis in the United States. Crit Care Med. May 2013;41(5):1167-74. doi:10.1097/CCM.0b013e31827c09f8
- Iwashyna TJ, Angus DC. Declining case fatality rates for severe sepsis: good data bring good news with ambiguous implications. JAMA. 2014;311:1295-1297. doi:10.1001/jama.2014.2639
- Rhee C, Klompas M. Sepsis trends: increasing incidence and decreasing mortality, or changing denominator? J Thorac Dis. Feb 2020;12(Suppl 1):S89-S100. doi:10.21037/jtd.2019.12.51
- CDC. Hospital Toolkit for Adult Sepsis Surveillance. Accessed Jan 30, 2019. https://www.cdc.gov/sepsis/pdfs/Sepsis-Surveillance-Toolkit-Mar-2018_508.pdf [PDF – 32 Pages]
- Rhee C, Dantes R, Epstein L, et al. Incidence and Trends of Sepsis in US Hospitals Using Clinical vs Claims Data, 2009-2014. JAMA. 2017;318(13):1241-1249. doi:10.1001/jama.2017.13836
- McGrath BM, Takamine L, Hogan CK, et al. Interpretability, credibility, and usability of hospital-specific template matching versus regression-based hospital performance assessments; a multiple methods study. BMC Health Serv Res. Jun 3 2022;22(1):739. doi:10.1186/s12913-022-08124-w
- Pandolfi F, Brun-Buisson C, Guillemot D, Watier L. One-year hospital readmission for recurrent sepsis: associated risk factors and impact on 1-year mortality-a French nationwide study. Crit Care. Nov 29 2022;26(1):371. doi:10.1186/s13054-022-04212-9
- Gallop KH, Kerr CEP, Nixon A, Verdian L, Barney JB, Beale RJ. A qualitative investigation of patients' and caregivers' experiences of severe sepsis*. Critical care medicine. 2015;43(2):296-307. doi:10.1097/CCM.0000000000000613
- Huang CY, Daniels R, Lembo A, et al. Life after sepsis: an international survey of survivors to understand the post-sepsis syndrome. Int J Qual Health Care. Jun 19 2018;doi:10.1093/intqhc/mzy137.
- Afshar M, Arain E, Ye C, et al. Patient Outcomes and Cost-Effectiveness of a Sepsis Care Quality Improvement Program in a Health System. Crit Care Med. Oct 2019;47(10):1371-1379. doi:10.1097/CCM.0000000000003919
- Thursky K, Lingaratnam S, Jayarajan J, et al. Implementation of a whole of hospital sepsis clinical pathway in a cancer hospital: impact on sepsis management, outcomes and costs. BMJ Open Qual. 2018;7(3):e000355. doi:10.1136/bmjoq-2018-000355
- Sreeramoju P, Voy-Hatter K, White C, et al. Results and lessons from a hospital-wide initiative incentivised by delivery system reform to improve infection prevention and sepsis care. BMJ Open Qual. Feb 2021;10(1)doi:10.1136/bmjoq-2020-001189