At a glance
- Healthcare providers should be aware of emerging strains of dermatophytes causing severe ringworm.
- Diagnosis of emerging strains often requires specialized testing only available at select reference laboratories.
- Some are antimicrobial-resistant.
- One emerging strain, which is generally not antimicrobial resistant, is frequently transmitted through sexual contact.
- Treatment of antimicrobial-resistant strains may require itraconazole or other antifungal medications usually reserved for invasive fungal infections.

Overview
Healthcare providers are familiar with common ringworm ("tinea" and "dermatophytosis"), typically mild rashes treatable with antifungal medication.
Over the past decade, increasing reports of severe atypical cases of ringworm have been reported worldwide. One new strain is primarily sexually transmitted. Some emerging strains cause antimicrobial-resistant infections.
Three emerging strains that have been reported in the United States are:
- Trichophyton indotineae (T. indotineae)
- Trichophyton mentagrophytes genotype type VII (TMVII)
- Terbinafine-resistant Trichophyton rubrum (T. rubrum)
Antimicrobial resistance
Not all emerging types of ringworm are antimicrobial-resistant. However, it is important to monitor patient response to treatment. Consider antimicrobial susceptibility testing when symptoms do not improve with treatment. Two antimicrobial-resistant strains of public health concern in the United States are T. indotineae and terbinafine-resistant T. rubrum.
The true number of antimicrobial-resistant ringworm cases is difficult to estimate. Antifungal susceptibility testing for dermatophytes is not widely available and the United States does not require reporting.
Several factors may be contributing to the emergence and spread of antimicrobial-resistant ringworm:
- Use of topical antifungal-corticosteroid combination products.
- Inappropriate prescription of antifungal drugs.
- Misuse of over-the-counter topical antifungal drugs.
- Inadequate adherence to prescribed courses of antifungal medication.
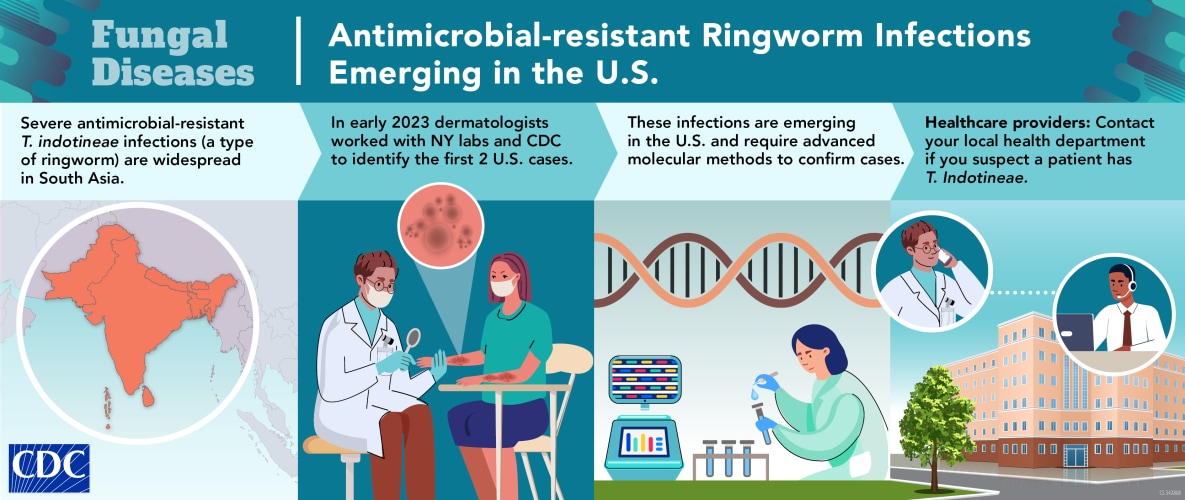
Get the clinician's perspective and learn how advanced molecular detection confirmed initial U.S. cases: Identifying Resistant Ringworm
Emerging strains
Trichophyton indotineae (T. indotineae)
T. indotineae, previously considered a subtype of Trichophyton mentagrophytes is now considered its own species. T. indotineae often has genetic mutations that make it resistant to antifungal drugs, including terbinafine, a first-line treatment.
Ringworm caused by T. indotineae is often severe (covering large regions of the body) and difficult to treat. Lesions affecting the genitals are uncommon but have been reported.
In South Asia, cases of antimicrobial-resistant T. indotineae infections became widespread. Although less common, cases are increasingly being reported outside of the Indian subcontinent, including in Europe, North America, South America, and Africa.
Diagnosing T. indotineae infection requires advanced molecular techniques such as genomic sequencing. Most clinical laboratories cannot distinguish T. indotineae from T. mentagrophytes or T. interdigitale, other types of dermatophyte that cause ringworm.

Trichophyton mentagrophytes genotype VII (TMVII)
TMVII is an emerging dermatophyte fungus that may be spread during sex. It can cause inflamed, painful, itchy, and persistent skin lesions, located on the genitals, buttocks, or face.
TMVII has been circulating in Europe for several years mostly reported among men who have sex with men. Some cases have also occurred among people who traveled to Southeast Asia for sex tourism. TMVII can also spread through clothing, towels, and bedding that have not been disinfected after use by someone with TMVII.
In June 2024, TMVII infection was documented in a man in New York City following travel to several European countries and California. TMVII cases do not appear to be widespread in the United States. Public health officials have identified several additional in New York City who have been affected.
Diagnosing TMVII infection requires advanced molecular techniques such as genomic sequencing. Most clinical laboratories cannot distinguish TMVII from T. mentagrophytes or T. interdigitale, two other types of dermatophytes.
Current evidence suggests that oral terbinafine is effective for TMVII infections, but some patients may require itraconazole. Patients may require weeks to months of antifungal therapy.
Terbinafine-resistant Trichophyton rubrum (T. rubrum)
Trichophyton rubrum (T. rubrum) is the most common cause of fungal nail infections (onychomycosis) and ringworm worldwide. Cases of T. rubrum that are resistant to the terbinafine, the first-line treatment, are increasingly being reported.
Public health efforts and research
CDC works closely with state and local health departments, academia, international organizations, and other federal agencies to address antimicrobial resistance.
CDC leads and supports several projects related to ringworm through its Antimicrobial Resistance Solutions Initiative, including:
- Performing outreach to healthcare providers and professional societies to raise awareness of antimicrobial-resistant ringworm and improve adherence to guidelines for ringworm diagnosis and treatment.
- Supporting studies to better understand the burden of antimicrobial-resistant ringworm in the United States, with an emphasis on preventing further spread.
- Increasing laboratory capacity for antifungal susceptibility testing.
More resources
Medscape
What to Know About Sexually Transmitted Ringworm
5 Things to Know About Antimicrobial-Resistant Tinea (Ringworm)
MMWR
Notes from the Field: Trichophyton mentagrophytes Genotype VII — New York City, April–July 2024
Webinar
Superficial Fungal Infections and Implantation Mycoses: What’s New?
