Key points
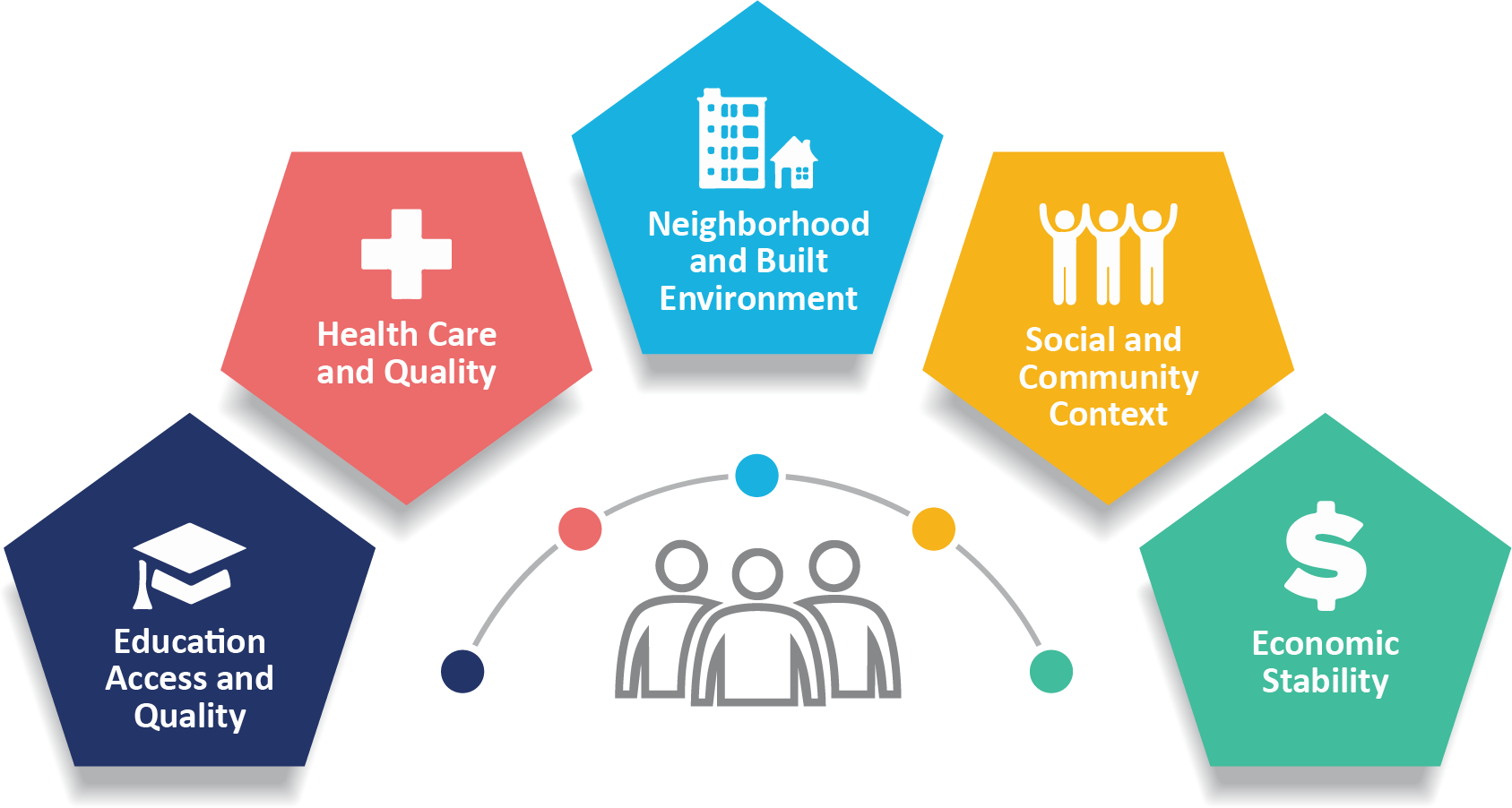
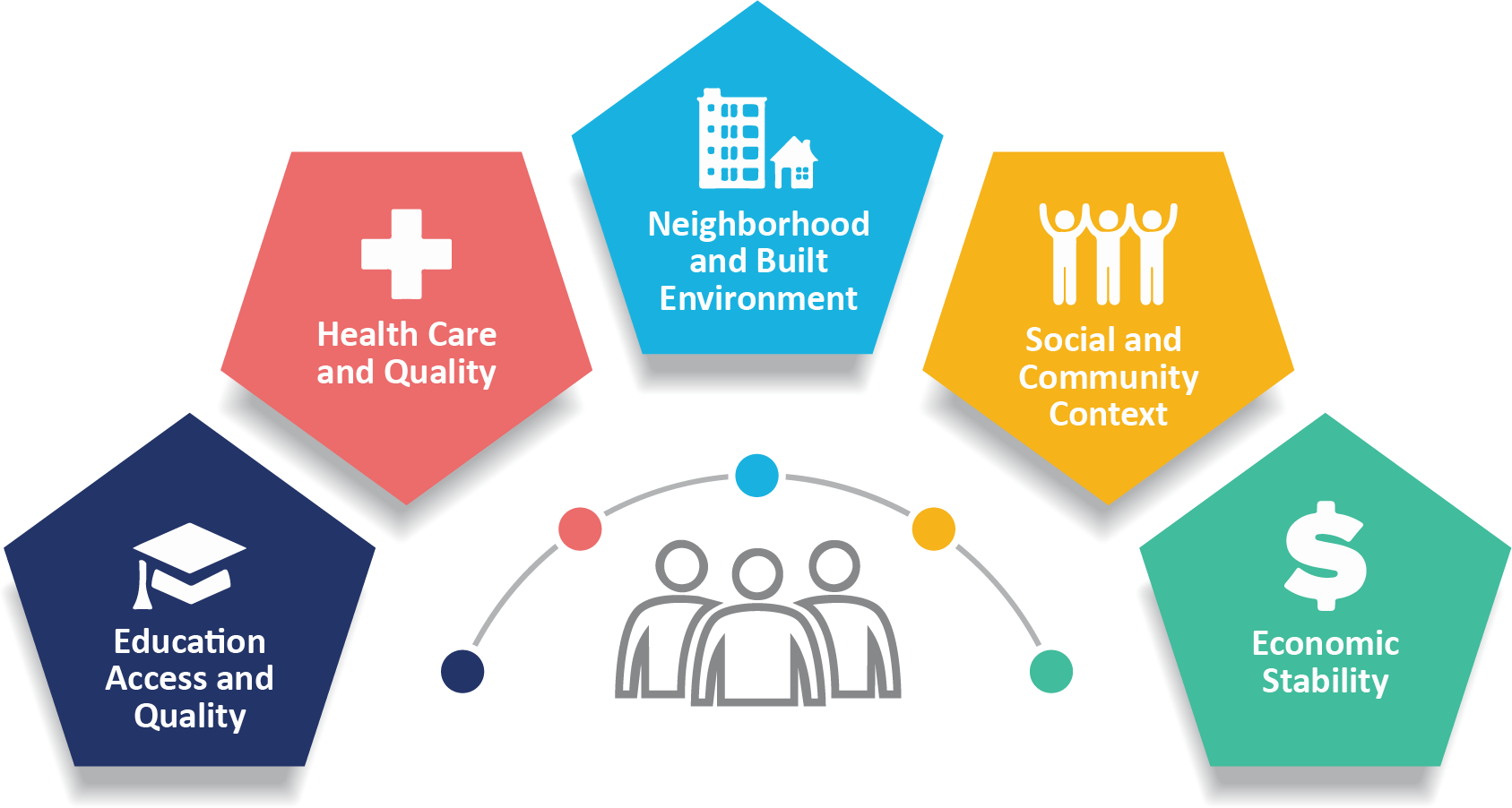
- Social determinants of health (SDOH) are non-medical factors affecting health, like socioeconomic status, and geographic location.
- Addressing SDOH can enhance health and lead to better outcomes.
Overview
Social determinants of health (SDOH) are non-medical factors that affect health outcomes. They include the conditions in which people are born, grow, work, live, and age. SDOH also include the broader forces and systems that shape everyday life conditions.
These forces and systems encompass economic policies, development agendas, social norms, social policies, racism, climate change, and political structures. CDC adapted this definition from the WHO 2022 definition of SDOH. Healthy People 2030 highlights SDOH in its key health indicators.
How SDOH Impacts Lives
A better understanding of incorporating SDOH into public health work and the 10 Essential Public Health Services strengthens public health capacity. Health equity ensures everyone has a fair chance to achieve optimal health. Along with the powerlessness that can arise from poverty and discrimination, limited access to the following can also occur:
- Quality jobs
- Education
- Housing
- Safe environments
- Healthcare
To advance health equity, SDOH factors, such as those above, should be addressed.
Resources
The following are a few ways in which the CDC's National Center for State, Tribal, Local, and Territorial Public Health Infrastructure and Workforce (Public Health Infrastructure Center) integrates SDOH into its activities.
Pathways to Population Health Equity
Pathways to Population Health Equity (P2PHE) provides tools for public health leaders to enhance population health, well-being, and equity. P2PHE includes a framework, roadmaps, compass, and various tools to help public health practitioners develop more prepared, resilient, and proactive systems. These tools and framework are adaptable to address the most pressing issues in any jurisdiction.
Community health assessment and improvement planning
CDC collaborates with various partners to offer technical support, resources, and training. This helps health departments and community partners in assessment and planning. For instance, the Public Health Infrastructure Center partners with the National Association of County and City Health Officials to promote the Mobilizing for Action through Planning and Partnerships (MAPP) planning framework. This framework integrates health equity in its guidance and practice.
Health department, hospitals, and others use certain tools and requirements to drive planning for community health assessment and health improvement. These tools and requirements emphasize data on health inequities, SDOH, and structural determinants of health in state and community planning efforts.
These collaborative processes involve diverse populations and multi-sector partners across jurisdictions. This results in plans that identify priorities and strategies to tackle health disparities.
Innovative funding strategies to support SDOH efforts
The Public Health Infrastructure Center works with partner organizations to explore health department use of innovative financing strategies. These strategies can be opportunities to address SDOH. Examples from partners include case stories about the following:
- Braiding and layering funds to address housing and food insecurity.
- Use of participatory budgeting to ensure community-driven funding decisions.
COVID-19 health equity grant
The National Initiative to Address COVID-19 Health Disparities Among Populations at High-Risk and Underserved, Including Racial and Ethnic Minority Populations and Rural Communities is a $2.5 billion grant supporting 108 state, territorial, local, and tribal health departments. It aims to reduce COVID-19 health disparities and promote health equity by enhancing capacity and services of the following health departments:
- State
- Local
- US territorial
- Freely associated state
One key strategy is to engage partners and collaborators to advance health equity and address SDOH related to COVID-19's effect on higher-risk and underserved groups.
Public health accreditation
The CDC backs the national accreditation program, managed by the Public Health Accreditation Board (PHAB). The national standards, which are central to the accreditation program, emphasize health equity and SDOH across various requirements. This includes community health assessment, health improvement planning, health promotion, policy development, and internal training. Health departments are striving to meet these standards. Evidence from evaluation studies and accredited sites indicates that in doing so, they are enhancing multi-sectoral partnerships and adopting practices like:
- Formulating health equity policies.
- Setting up agency-wide health equity councils.
