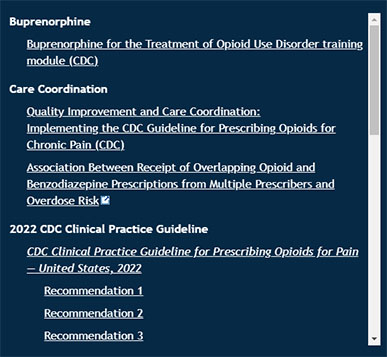
Buprenorphine
Buprenorphine for the Treatment of Opioid Use Disorder training module (CDC)
Care Coordination
2022 CDC Clinical Practice Guideline
CDC Clinical Practice Guideline for Prescribing Opioids for Pain — United States, 2022
Clinical Practice Guideline at a Glance (CDC)
Motivational Interviewing
Motivational Interviewing training module (CDC)
Motivational Interviewing patient case (CDC)
Naloxone
Opioids
Opioid Use Disorder
Assessing and Addressing Opioid Use Disorder (OUD) training module (CDC)
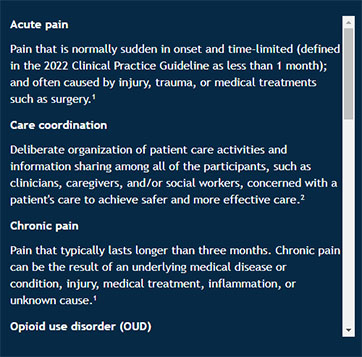
Acute pain
Pain that is normally sudden in onset and time-limited (defined in the 2022 Clinical Practice Guideline as less than 1 month); and often caused by injury, trauma, or medical treatments such as surgery.1
Care coordination
Deliberate organization of patient care activities and information sharing among all of the participants, such as clinicians, caregivers, and/or social workers, concerned with a patient's care to achieve safer and more effective care.2
Chronic pain
Pain that typically lasts longer than three months. Chronic pain can be the result of an underlying medical disease or condition, injury, medical treatment, inflammation, or unknown cause.1
Opioid use disorder (OUD)
A problematic pattern of opioid use leading to clinically significant impairment or distress. A diagnosis is based on specific Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) criteria, such as unsuccessful efforts to cut down or control use, or use resulting in social problems and a failure to fulfill obligations at work, school, or home, among other criteria.3
Subacute pain
Pain with a duration of at least one month and up to three months.1 Subacute pain can be the result of an underlying medical disease or condition, injury, medical treatment, inflammation, or unknown cause.
Psychosocial supports - Ancillary services to enhance a patient's overall functioning and well-being, including recovery support services, case management, housing, employment, and educational services.4
Tapering
The deliberate and gradual reduction of medication dosage over a period of time to provide the body with an opportunity to adjust to the decreasing dosage, thereby reducing the likelihood of withdrawal symptoms and other negative consequences associated with abrupt cessation of a medication. This process is often implemented for a variety of reasons, including, but not limited to, reducing the dosage of opioids to minimize side effects, or discontinuing the use of opioids completely.
1 Dowell D, Ragan KR, Jones CM, Baldwin GT, Chou R. CDC Clinical Practice Guideline for Prescribing Opioids for Pain — United States, 2022. (2022). MMWR Recommendations and Reports; 71(No. RR-3):1–95. DOI: http://dx.doi.org/10.15585/mmwr.rr7103a1
2 Agency for Healthcare Research and Quality. (2018, August). Care Coordination. Retrieved September 6, 2022, from https://www.ahrq.gov/ncepcr/care/coordination.html
3 American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. Arlington, VA, American Psychiatric Association, 2013.
4 Treatment Improvement Protocol (TIP) Series 63: Medications for Opioid Use Disorder. (2021). Substance Abuse and Mental Health Services Administration. Publication No. PEP21-02-01-002. Retrieved September 6, 2022, from https://store.samhsa.gov/sites/default/files/SAMHSA_Digital_Download/PEP21-02-01-002.pdf