Key points
- People and animals are getting sick from harmful algal blooms (HABs) across the United States.
- Thirteen states reported 227 HAB events, 95 human illnesses, and at least 1,170 animal illnesses.
- The first human death reported to OHHABS was associated with paralytic shellfish poisoning.

Background
Harmful algal blooms (HABs) that result from the rapid growth of algae or cyanobacteria (sometimes referred to as blue-green algae) in natural waterbodies can harm people, animals, or the environment. HAB events of public health concern are primarily caused by microalgae called diatoms and dinoflagellates, cyanobacteria, and the toxins they can produce. HAB events, which can be intensified by factors such as nutrient pollution and warmer water temperature, can have public health, environmental, and economic impacts.
HABs are a One Health issue—they affect the health of people, animals, and our shared environment. One Health is a collaborative and multi-sectoral approach that involves engagement across disciplines including public health, animal health, and environmental health. Using a One Health approach, CDC collects data about HAB events and associated human or animal illnesses through the One Health Harmful Algal Bloom System (OHHABS) to inform public health prevention efforts.
Within the context of OHHABS, the term HAB event describes the identification of a bloom or the detection of HAB toxins in water or food (i.e., absent a visual bloom). Human illnesses are reported individually. Animal illnesses are reported as single cases of illness or in groups, such as flocks of birds. The reporting system can link HAB event data with human or animal illness data. OHHABS uses standard definitions to classify HAB events as suspected or confirmed and human or animal illness as suspected, probable, or confirmed.
OHHABS is available for voluntary reporting by public health agencies and their designated environmental health or animal health partners in the United States, District of Columbia, Federated States of Micronesia, Guam, Marshall Islands, Northern Mariana Islands, Palau, Puerto Rico, and U.S. Virgin Islands. Public health agencies use standard forms to report HAB events, human cases of illness, and animal cases of illness to OHHABS. Public health agencies do not need to submit all three types of forms to participate.
Data collected for HAB events include general information (e.g., observation date), geographic information, water body characteristics (e.g., salinity), observational characteristics (e.g., water color, scum), and laboratory testing. Data collected for cases of illness include general demographic characteristics, exposure information, signs and symptoms, medical care, and health outcomes. OHHABS is a dynamic electronic reporting system; data within individual reports are subject to change over time. Data included in this report are from a specific point in time.
Methods
This summary describes data from OHHABS for events occurring between January 1, 2020 and December 31, 2020. Reports were received by January 3, 2022 and reviewed by CDC using standardized data quality checks. CDC downloaded the final dataset on March 21, 2022. CDC used SAS (version 9.4; SAS Institute) to conduct descriptive analyses to characterize HAB events and associated human or animal cases of illness.
Reports that included environmental testing laboratory results were considered 'positive detections' even if they did not include a specific concentration detected (e.g., if a toxin was reported with no concentration). These results were included in the summarized environmental testing data. Reported concentrations of 0 were considered non-detects and not included.
If group animal reports were missing the number of individuals affected, the number was set to two for inclusion in descriptive analyses. If group animal reports indicated deaths occurred but did not provide the number of individuals that died, the number of deaths was set to missing as this could not be extrapolated from available information.
Public health agencies classified HAB events as suspected or confirmed and cases of illness as suspected, probable, or confirmed (2018 OHHABS case and event definitions). Animals within group animal reports were classified according to the overall classification (e.g., if a group of 10 animals was classified as "probable," then each animal was subsequently defined as a probable case of illness).
Findings
During 2020, 227 HAB events were reported by 13 state jurisdictions: Alaska, California, Connecticut, Kansas, Michigan, Ohio, Oregon, Pennsylvania, Tennessee, Utah, Virginia, Washington, and Wisconsin (Figure 1). These HAB events resulted in 95 human cases of illness and at least 1,170 animal cases of illness. Twenty-one groups of animals were reported, ranging in size from 2-1,000 individuals (Figure 2).
Reported HAB events occurred predominantly in summer months, peaking in July (59; 26%) (Figure 3) and were most often classified as confirmed (79%) (Figure 3). Human cases of illness occurred primarily in July and August (73%). A single fish kill (i.e., localized die off of a fish population) in September included at least 1,000 carp. The remaining animal cases of illness (15%) occurred primarily in May and June (43%). Case classification differed between human and animal cases of illness; the majority (61; 64%) of human cases of illness were classified as suspected and 1,134 (97%) animal cases of illness as probable (Figure 4).
Data
Overview
Figure 1: States reporting HAB events for 2020
13 states reported to OHHABS for 2020.
Figure 2: Reported HAB events with associated human and animal cases, 2020
227 HAB events resulted in 95 human illnesses and at least 1,170 animal illnesses in 2020.
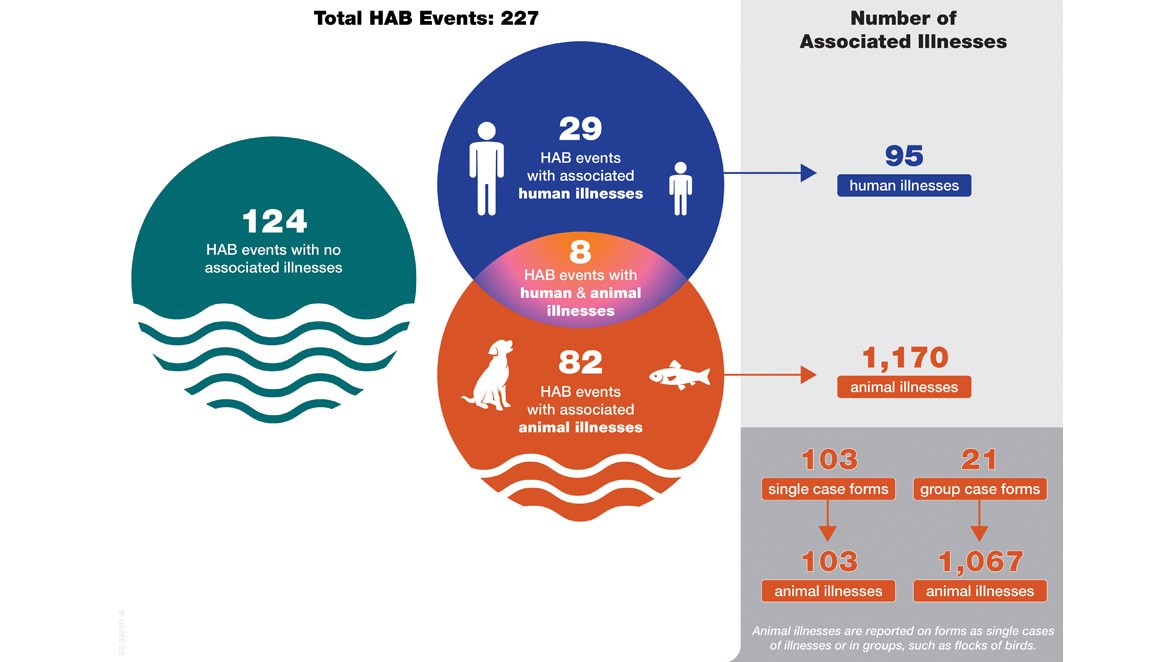
Figure 3: Reported HAB events and cases by month, 2020
Most reported HAB events and illnesses occurred during the summer and early fall in 2020.
Figure 4. Proportion of reported HAB events and associated human and animal cases by classification, 2020
In 2020, 79% of HAB events were classified as confirmed, 64% of human illnesses as suspected, and 97% of animal illnesses as probable.
HAB events can only be classified as “suspected” or “confirmed.”
HAB Events
Most (173; 76%) of the 227 HAB events occurred in fresh water (Figure 5a), primarily in lakes and reservoirs (88%) (Figure 5b). Within the freshwater HAB event subset, observers most frequently noted green water color (23%), however, one or more observations of clear water were reported during 20% of these HAB events. (Figure 6). Scum or algal matter was observed in 116 of 120 (97%) HAB events that included information on scum presence or absence.
Environmental testing for algal toxins or species was conducted for 187 HAB events (82%), with the most frequently reported reasons being monitoring (72%) and citizen complaints (26%) (Figure 7). Overall, toxins were detected in 51% of all HAB events (115/227), 97% of which were freshwater events (Figure 8). Toxin testing primarily identified microcystins (107; 93%) (Figure 9a); multiple toxins were reported for 11 HAB events. Pseudo-nitzschia was the most identified genus during environmental testing, detected in 22 HAB events. Microcystis was the most commonly identified cyanobacterial genus, detected in 10 of 23 (43%) HAB events caused by cyanobacteria (Figure 9b). Cyanobacterial genera (Anabaena and Nodularia) were identified in marine coastal waters during one HAB event.
Figure 5a: Reported HAB events by water salinity, 2020
Most of the 227 HAB events during 2020 occurred in fresh water (n=173).
Figure 5b: Reported freshwater HAB events by water type, 2020
Freshwater HAB events during 2020 (n=173) were mostly in lakes, reservoirs, or impoundments.
Figure 6: Reported water color for freshwater HAB events, 2020
Freshwater HAB events with observational data (n=173) were most often green in color or clear.
Figure 7: Reasons for environmental testing of HAB events, 2020
In 2020, environmental testing occurred for 82% of HAB events (n=187) and was primarily due to water quality monitoring.
Figure 8: Environmental testing findings during HAB events, 2020
Environmental testing identified toxins in 51% of all reported 2020 HAB events (n=227).
Figure 9a. Identified toxins during environmental testing of HAB events, 2020
Microcystins were the most commonly identified toxins during environmental testing, detected in 107 of 115 HAB events (93%).
Figure 9b. Identified genera during environmental testing of HAB events, 2020
Pseudo-nitzschia was the most commonly identified genus during environmental testing, detected in 22 HAB events, and Microcystis was the most commonly identified cyanobacterial genus, detected in 10 events.
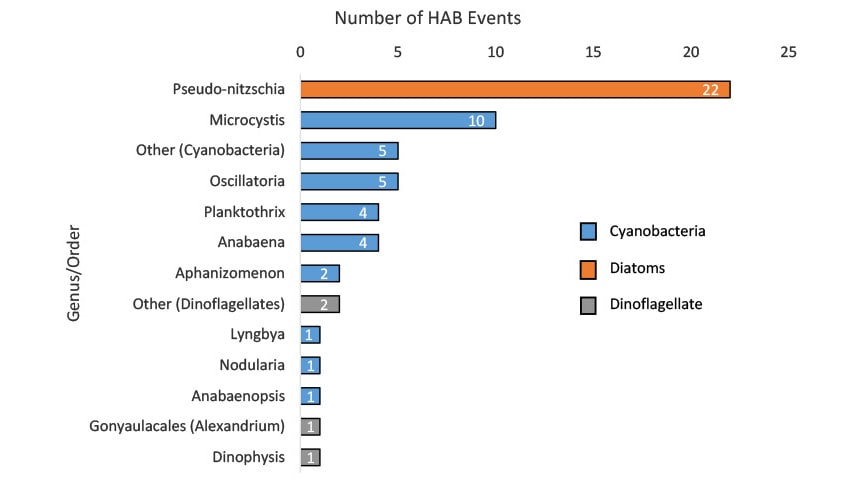
| Cyanobacteria Genus | Number of HAB Events |
|---|---|
| Anabaena | 4 |
| Anabaenopsis | 1 |
| Aphanizomenon | 2 |
| Lyngbya | 1 |
| Microcystis | 10 |
| Nodularia | 1 |
| Oscillatoria | 5 |
| Other | 5 |
| Planktothrix | 4 |
| Diatom Genus | Number of HAB Events |
| Pseudo-nitzschia | 22 |
| Dinoflagellate Order | Number of HAB Events |
| Dinophysis | 1 |
| Gonyaulacales (Alexandrium) | 1 |
| Other | 2 |
Human Illnesses
Of 95 human cases of illness reported to OHHABS for 2020, 41 (43%) illnesses occurred in adults aged 18-45 years and 24 (25%) illnesses occurred in people under age 18 (Figure 10). People who became ill were exposed to HABs predominately at public outdoor areas and parks (72%). National parks were associated with 22 (23%) human cases of illness, with 21 illnesses attributed to a single HAB event. Nearly all (95%) of the 95 people who became ill reported water and 9% reported air as a source of exposure (multiple sources were reported in 7% of illnesses). People sought care in 73 (77%) instances; over half (71%) called a poison control center, and 2% of illnesses resulted in an emergency department visit. One death associated with paralytic shellfish poisoning was reported following a non-commercial shellfish harvest (Table 1).
Numerous signs and symptoms were reported; the most commonly reported types were dermatologic (42%), gastrointestinal (41%), and generalized (36%) (Figure 11). Overall, rash (23%) and nausea (20%) were most commonly reported signs and symptoms (Table 2). Median time to illness onset was 3.75 hours (0.02-96; n=73) and median illness duration was 24 hours (0.17-504; n=47); 64% of ill people still exhibited signs or symptoms at the time of interview (Table 1).
Figure 10: HAB-associated human cases by age group, 2020
Nearly half (43%) of reported human illnesses during 2020 were among adults, while people under the age of 18 accounted for 25%.
Figure 11: Signs and symptoms of HAB-associated human cases, 2020
Dermatologic and gastrointestinal were the most frequently reported types of signs and symptoms among people who became ill during 2020 (n=95).
Table 1. Medical care for HAB-associated human cases, 2020
77% of ill people sought care from at least one source.
| Health-seeking Behavior | Number (%) |
|---|---|
| Any health-seeking behavior | 73 (77) |
| Call to a poison control center | 67 (71) |
| Visit to healthcare provider | 15 (16) |
| Visit to emergency department | 2 (2) |
| Received first aid care | 13 (14) |
| Symptoms at time of case interview | 61 (64) |
Table 2. Signs and symptoms reported by HAB-associated human cases, 2020
Rash (23%) and nausea (20%) were the most commonly reported signs and symptoms of human illness (n=95).
| Classification | Sign/Symptom | Number (%) |
|---|---|---|
| Dermatologic | 40 (42) | |
| Bullous skin lesions (fluid filled blisters) | 3 (3) | |
| Dermatologic symptoms (nonspecific) | 1 (1) | |
| Erythema (redness) | 3 (3) | |
| Irritated skin | 4 (4) | |
| Pruritus (itchy skin) | 15 (16) | |
| Rash | 22 (23) | |
| Skin blisters | 3 (3) | |
| Skin burning/pain | 4 (4) | |
| Skin infection | 1 (1) | |
| Urticaria (hives) | 5 (5) | |
| Gastrointestinal | 39 (41) | |
| Abdominal cramps | 3 (3) | |
| Abdominal pain (tenderness) | 8 (8) | |
| Diarrhea | 18 (19) | |
| Gas/bloating | 2 (2) | |
| Gastroenteritis (nonspecific) | 1 (1) | |
| Gastrointestinal (nonspecific) | 2 (2) | |
| Nausea | 19 (20) | |
| Vomiting | 12 (13) | |
| Generalized | 34 (36) | |
| Anorexia (loss of appetite) | 1 (1) | |
| Chills | 1 (1) | |
| Faintness (lightheadedness) | 1 (1) | |
| Fatigue | 11 (12) | |
| Fever | 4 (4) | |
| Flu-like symptoms | 1 (1) | |
| Flushing (face or body) | 1 (1) | |
| Headache | 13 (14) | |
| Hot flash | 1 (1) | |
| Irritability | 3 (3) | |
| Lethargy (lack of energy, tiredness) | 1 (1) | |
| Malaise (general discomfort) | 4 (4) | |
| Myalgia (general achiness, pain) | 4 (4) | |
| Pain (general) | 1 (1) | |
| Ear, Nose, Throat | 13 (14) | |
| Nasal inflammation | 1 (1) | |
| Nasal, congestion (rhinitis) | 3 (3) | |
| Nasal, coryza (runny nose) | 3 (3) | |
| Oral ulcers | 1 (1) | |
| Oral, swelling | 1 (1) | |
| Throat pain | 2 (2) | |
| Throat, irritation | 4 (4) | |
| Throat, sore | 5 (5) | |
| Other | 12 (13) | |
| Other | 12 (13) | |
| Ophthalmologic | 9 (9) | |
| Eyes, burning | 2 (2) | |
| Eyes, conjunctivitis (pinkeye) | 1 (1) | |
| Eyes, discharge | 1 (1) | |
| Eyes, irritation | 2 (2) | |
| Eyes, pain | 3 (3) | |
| Eyes, periorbital edema (swelling) | 3 (3) | |
| Eyes, red | 1 (1) | |
| Neurologic | 7 (7) | |
| Dizziness | 3 (3) | |
| Neurological symptoms (nonspecific) | 2 (2) | |
| Numbness | 1 (1) | |
| Paresthesia (tingling sensation) | 2 (2) | |
| Weakness | 1 (1) | |
| Cardiopulmonary | 4 (4) | |
| Cardiac symptoms (nonspecific) | 1 (1) | |
| Respiratory (nonspecific) | 1 (1) | |
| Respiratory irritation | 2 (2) | |
| Shortness of breath | 1 (1) | |
| Musculoskeletal | 1 (1) | |
| Musculoskeletal (nonspecific) | 1 (1) |
Animal Illnesses
At least 1,170 animal cases of illness occurred and were reported to OHHABS for 2020, including a large fish kill involving at least 1,000 carp. Most cases were classified as probable (97%), regardless of animal category (Figure 12). Among 37 domestic pet cases and 1,133 wildlife cases, dogs (100%) and fish (90%), respectively, were the most common animals affected (Figure 13a). No livestock cases were reported. Veterinary care was provided to 89 animals, including 66 marine mammals, 19 dogs, and 4 birds (Figure 13b).
Data describing signs of illness were available for 37 animals, all of which were dogs. Generalized (76%) and gastrointestinal (68%) signs were most frequently reported overall (Figure 14). Individually, vomiting (46%) was most commonly reported (Table 3). Median time to illness onset was 3.5 hours (0.02-72) for the 19 animals with available information, and median duration of illness was 6 hours (0.02-168) for 12 animals with available information. In total, 1,094 (94%) of the animals died.
Figure 12: Proportion of HAB-associated animal cases by animal category by classification, 2020
Most animal illnesses reported for 2020 were classified as probable.
Figure 13a: Reported animal types of HAB-associated animal cases, 2020
Most animal illnesses reported for 2020 were associated with a fish kill affecting at least 1,000 individual carp. All of the domestic pet illnesses occurred in dogs.
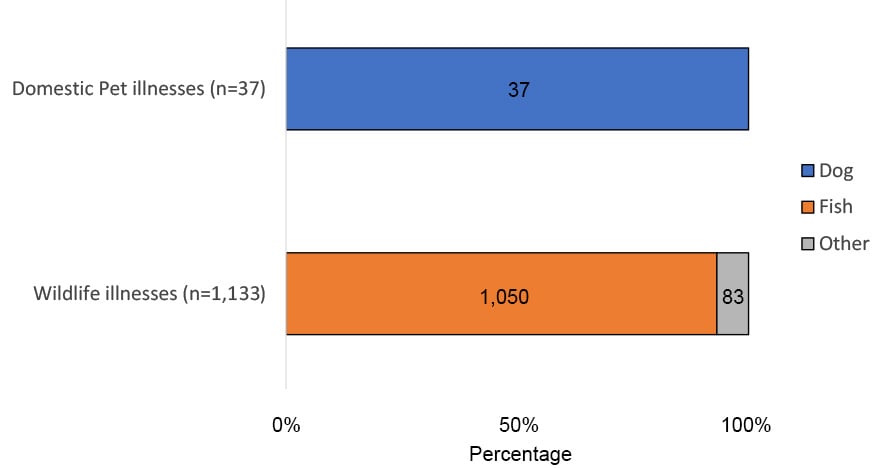
| Reported Animal Illnesses | Frequency | Percent |
|---|---|---|
| Individual Number of Animals Affected | 1,170 | 100% |
| Domestic Pet | 37 | 3% |
| Dog | 37 | 100% |
| Wildlife | 1,133 | 97% |
| Fish | 1,050 | 93% |
| Other | 77 | 7% |
Figure 13b: Reported animal types of HAB-associated animal cases (excluding fish kill), 2020
Excluding the fish kill, marine mammals were the most reported type of animal that became ill during 2020.
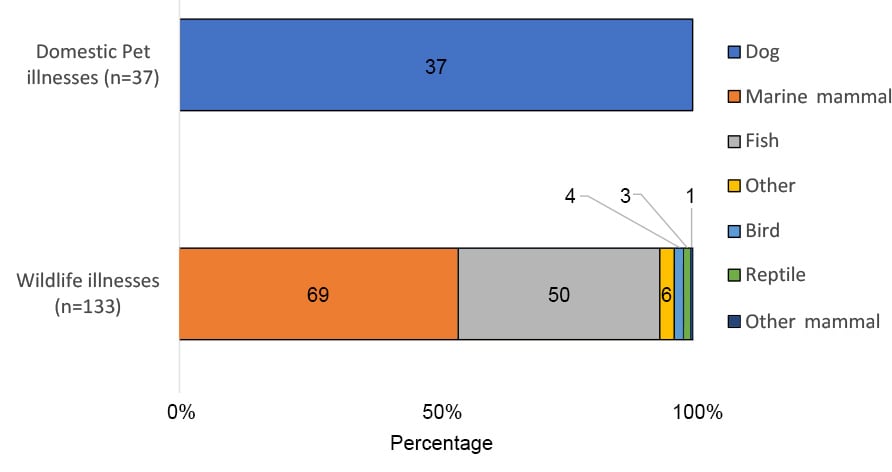
| Animal | Illness Type | Number | Percent |
|---|---|---|---|
| Dog | Domestic Pet Illness | 37 | 100% |
| Bird | Wildlife Illness | 4 | 3% |
| Fish | Wildlife Illness | 50 | 38% |
| Marine mammal | Wildlife Illness | 69 | 52% |
| Reptile | Wildlife Illness | 3 | 2% |
| Other | Wildlife Illness | 6 | 5% |
| Other mammal | Wildlife Illness | 1 | 1% |
Figure 14: Signs in HAB-associated animal cases, 2020
Generalized and gastrointestinal signs were the most frequently reported signs for animal illnesses during 2020 (n=37).
Table 3: Signs reported for HAB-associated animal cases, 2020
Vomiting (46%) and lethargy (41%) were the most commonly observed signs in reported animal illnesses (n=37).
| Classification | Symptom | Number (%) |
|---|---|---|
| Generalized | 28 (76) | |
| Anorexia (loss of appetite) | 8 (22) | |
| Dehydration (refusing water) | 1 (3) | |
| Fever | 1 (3) | |
| Lethargy | 21 (57) | |
| Muscle tremors | 4 (11) | |
| Weakness | 1 (3) | |
| Whining or abnormal vocalization | 2 (5) | |
| Gastrointestinal | 25 (68) | |
| Blood in stool | 1 (3) | |
| Diarrhea | 11 (30) | |
| Drooling/salivation | 6 (16) | |
| Liver failure | 1 (3) | |
| Mucous in stool | 1 (3) | |
| Vomiting | 22 (59) | |
| Neurologic | 11 (30) | |
| Ataxia (stumbling, loss of balance) | 5 (14) | |
| Behavior change | 4 (11) | |
| Coma (non-responsive to stimuli) | 1 (3) | |
| Loss of balance | 1 (3) | |
| Seizure/Convulsions | 3 (8) | |
| Cardiopulmonary | 8 (22) | |
| Cardiac Arrest | 1 (3) | |
| Cough | 1 (3) | |
| Labored breathing | 3 (8) | |
| Panting | 2 (5) | |
| Respiratory arrest | 4 (11) | |
| Wheezing | 1 (3) | |
| Other | 8 (22) | |
| Limping | 1 (3) | |
| Other | 7 (19) | |
| Dermatologic | 5 (14) | |
| Rash | 5 (14) | |
| Ear, Nose, Throat | 4 (11) | |
| Ear irritation | 4 (11) | |
| Genitourinary | 4 (11) | |
| Bladder incontinence | 3 (8) | |
| Dark urine | 1 (3) | |
| Ophthalmologic | 1 (3) | |
| Eye discharge | 1 (3) |
Limitations
Data reported in OHHABS for 2021 are not representative of HAB event or illness occurrence in the United States because reporting is voluntary and not all states are currently reporting to this system. States may not report information for all HAB events or illnesses due to variability in surveillance capacity, surveillance program scope, or limitations to the environmental or health data available for HAB events. Environmental testing might have been limited by availability of testing for one or more toxins. Additionally, the total number of individual animals described in this report underrepresents the total affected or that died during these events because some group animal reports did not provide these numbers or indicated that the number was an underestimate. Summarized data therefore underrepresent the total number of HAB events and illnesses that occurred within or across states. Similarly, relative contributions of HAB events in salt water, toxins identified in fresh water, and types of illnesses (e.g., domestic pets versus wildlife species), may also be affected. The effects of the COVID-19 pandemic on surveillance of HAB events (e.g., bloom detection and monitoring) and illnesses (e.g., exposure to HABs, healthcare seeking behavior) are not known.
Conclusion
Thirteen states reported to OHHABS for 2020. The findings from this annual data summary indicate that HAB events and associated illnesses occur throughout the United States. HAB event and illness reporting primarily characterized environmental data, exposures, and outcomes associated with freshwater cyanobacterial blooms. Affected people primarily reported dermatologic and gastrointestinal signs and symptoms, while affected animals—specifically dogs—presented with generalized and gastrointestinal signs.
The first report of a HAB-associated death to OHHABS demonstrates the health risks of consuming shellfish contaminated with algal toxins, along with potential for OHHABS to complement state/territorial surveillance (Newell, 2022) by aggregating case data about foodborne illnesses nationally. Data from environmental sampling, human illnesses, and animal illnesses highlight the diversity of HAB species, toxins, and health effects associated with HAB events.
Human health, animal health, and environmental health are interconnected; the continued use of a One Health approach to surveillance will inform illness prevention by increasing scientific understanding and data available to characterize HAB events and associated illnesses.
Acknowledgements
CDC would like to thank state and local waterborne disease coordinators, epidemiologists, environmental health practitioners, laboratorians, toxicologists, and animal health practitioners, as well as other partners who were involved in investigating or reporting these data to OHHABS.
