At a glance
- Antimicrobial resistance is a major global public health threat.
- Resistant bacteria can spread from food animals to people.
- Responsible use of antibiotics can help prevent resistant infections.
- CDC helps prevent resistant infections by tracking resistance, identifying sources of infection, and improving food safety.

The basics
Antimicrobial resistance
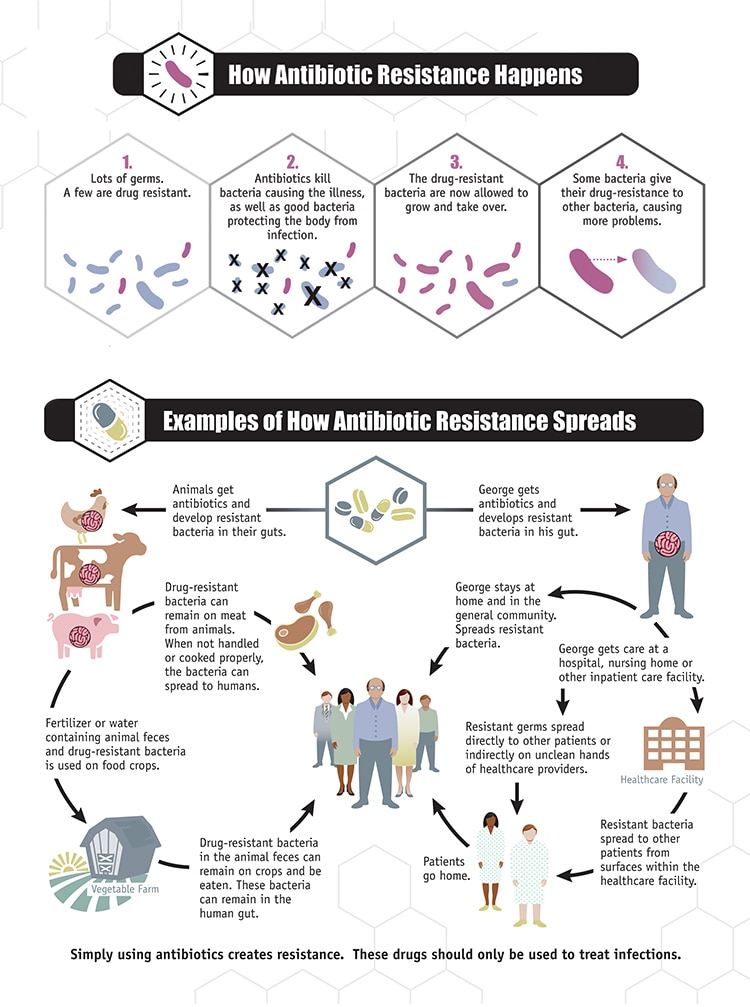
Antimicrobial resistance happens when bacteria develop the ability to defeat the drugs designed to kill them. That means the bacteria are not killed and continue to grow. Resistant infections can be difficult, and sometimes impossible, to treat.
Antimicrobial resistance is a major global public health threat. Illnesses that were once easily treatable with antibiotics and antifungals are becoming more difficult to cure and more expensive to treat. Common antimicrobial-resistant bacteria, such as Salmonella, can cause more severe health outcomes than bacteria that are not resistant.
How resistant infections affect people
Some resistant infections cause severe illness. People with these infections may
- Be more likely to be hospitalized and have higher medical expenses
- Take longer to get well
- Die from the infection
NARMS surveillance
NARMS scientists track and study changes in antimicrobial resistance among several bacteria, such as those transmitted commonly through food, water, animal contact, person-to-person contact, and environmental contamination.
NARMS data increase our understanding of
- Resistance trends
- New or emerging resistance
- Bacterial resistance genes
- Which resistant bacteria are making people sick
- Which groups of people are at risk and why
NARMS data are used to help guide efforts to prevent and reduce the spread of resistance and resistant bacteria. Organizations and groups using NARMS data include federal regulatory agencies, policymakers, consumer advocacy groups, health departments, industry, and the public.
Antibiotic use in food animals
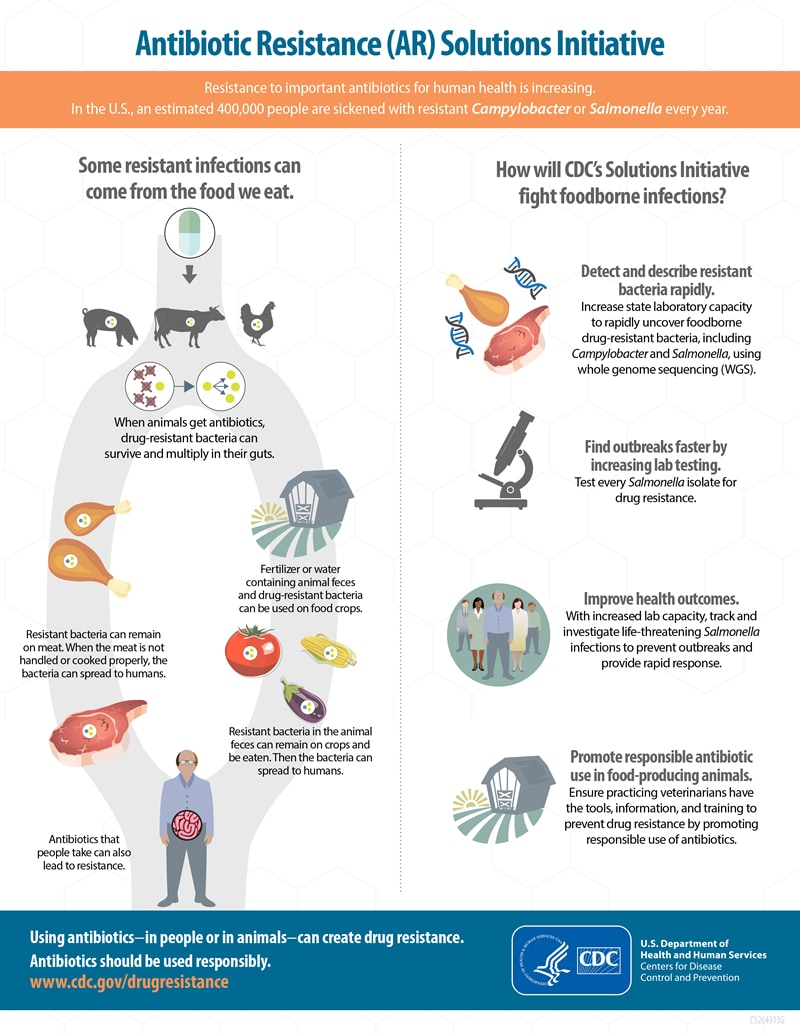
Food animals can carry bacteria, such as Salmonella and Campylobacter, that can make people ill. When animals are given antibiotics, resistant bacteria in their intestines can continue to survive and grow.
How resistant bacteria get into the food supply
Resistant bacteria that food animals carry can get into a variety of foods. Meat and poultry can become contaminated when the animals are slaughtered and processed. Fruits and vegetables can become contaminated when resistant bacteria from animal feces (poop) spreads to them through the environment, such as through irrigation water or fertilizers.
How people get infected with resistant bacteria from food animals
People can get infected with these bacteria in several ways, including
- Handling or eating raw or undercooked meat or poultry
- Coming into contact with food animals or their feces
- Eating raw fruits and vegetables that came into contact with animal feces in the environment, such as through irrigation water or fertilizer
- Consuming water, including recreational water, that came into contact with animal feces
The importance of using antibiotics responsibly in food animals
Antibiotics must be used responsibly in both people and animals to help prevent the development, persistence, and spread of resistant bacteria.
Antibiotics are valuable tools for reducing animal disease and suffering from bacterial infections, but decisions about which antibiotics to use in food animals and how to use them must also be made with consideration of human health and the environmental impact.
FDA has approved antibiotics for these uses in food animals:
- Disease treatment for animals that are sick.
- Disease control for a group of animals when some of the animals are sick.
- Disease prevention for animals that are at risk of becoming sick.
What you can do
You can reduce the chance of getting a resistant bacterial infection by following some recommendations for safe food handling and preparation.
- Follow the Clean, Separate, Cook, and Chill guidelines.
- Don't drink raw milk.
- Wash your hands after contact with human or animal feces, animals, or animal environments.
- Follow CDC's Traveler's Health recommendations for food and water safety when traveling internationally.
What CDC is doing
Preventing foodborne and other gastrointestinal illnesses reduces both susceptible and resistant infections. CDC activities that help prevent these infections include:
Tracking Resistance
- Tracking resistance in infections
- Estimating how many resistant infections occur
- Collaborating with domestic and international partners to monitor resistance and improve detection capacities
- Studying how resistance emerges and spreads
Identifying Sources of Infection
- Determining the sources of resistant infections that are commonly spread through food
- Investigating resistant infections to solve and stop outbreaks and improve prevention
- Developing better tools, such as whole genome sequencing, to accurately link cases of foodborne illness to outbreaks and identify sources of food contamination
Improving Food Safety
- Strengthening the ability of state and local health departments to detect, respond to, and report resistant infections
- Educating consumers and food workers about safe food handling and proper handwashing
- Identifying groups with a greater chance of infection and educating them about how to reduce the likelihood of illness
- Promoting the responsible use of antibiotics and antifungals in animals as well as people
Antibiotic use and healthcare
CDC estimates that U.S. doctors' offices and emergency departments prescribe about 47 million antibiotic courses each year for infections that don't need antibiotics. That's about 30% of all antibiotics prescribed in these settings.
Visit CDC's Be Antibiotics Aware website to learn how improving antibiotic use in hospitals can reduce rates of infection and antibiotic resistance, improve patient outcomes, and save hundreds of thousands of dollars.
Resources
CDC and antimicrobial resistance
Part of CDC's mission is to track the emergence of antimicrobial-resistant microorganisms and to limit their spread. This site gives information about what CDC is doing and what everyone can do to help combat antimicrobial resistance.
Campaign aiming to reduce the rising rate of antimicrobial resistance by promoting adherence to appropriate prescribing and usage guidelines.
Antimicrobial resistance, food, and food animals
Learn more about appropriate use of antibiotic and antifungal drugs in veterinary medicine and animal agriculture.
Antimicrobial resistance education
Antimicrobial resistance learning site for veterinary students
Open-source learning resource for antimicrobial use and antimicrobial resistance in animal agriculture and veterinary medicine. (University of Minnesota)
Animation of antimicrobial resistance
Video explaining how antimicrobial resistance emerges and proliferates among bacteria and how resistance complicates doctors' efforts to select the appropriate drugs to treat patients with infections. (FDA Center for Veterinary Medicine)
National Veterinary Accreditation Program: Learning module on antibiotic use in animals
Educational module with information on selection of antimicrobial agents for veterinary use, descriptions of antimicrobial susceptibility testing methods, lists of agencies involved in regulating antimicrobial agents, and more. (USDA)
