Key points
- Mucormycosis is a serious but rare fungal infection caused by a group of molds called mucormycetes.
- Mucormycosis mainly affects people with weakened immune systems.
- It most commonly affects the sinuses or the lungs.
- It can also occur on the skin after a cut, burn, or other type of skin injury.

Overview
Mucormycosis, sometimes called zygomycosis, is a rare but serious fungal infection caused by a group of molds called mucormycetes. These molds are common in the environment and most people are exposed to them every day without getting sick.
Usually, only people with weakened immune systems (lower ability to fight infections) get mucormycosis.
People can get exposed to mucormycetes different ways, causing different types of infections and symptoms. Murcormycosis can be deadly and requires treatment with antifungal medications. Mucormycosis is one of the most common diseases linked to mold outbreaks in healthcare settings.
Symptoms
Mucormycosis symptoms depend on which part of the body is affected. It can affect sinuses, brain, lungs, skin, stomach and intestines, or cause symptoms throughout the body. Mucormycosis most commonly affects the sinuses or the lungs and causes symptoms like cough, nasal congestion, and fever. Symptoms of skin infections include blisters and burns.
Causes and Risk
People with weakened immune systems can get mucormycosis from breathing in spores from mucormycetes. it can also be caused by eating something with the spores on it or from spores infecting a scrape or wound.
Some of these conditions that increase the risk for infection include:
- Cancer
- Organ or stem cell transplant
- Wounds or burns.
Mucormycetes are often found in soil and in decaying organic matter, such as leaves, compost piles, or rotten wood.
Mucormycosis does not spread from person to person.

Healthcare facilities
Outbreaks of invasive mold infections have occurred in healthcare facilities. Mold is found in all environments. Patients receiving medical care are more likely to have weakened immune systems and be at risk. Mold outbreaks have occurred through air filtration systems, water leaks, and in dampened hospital linens.
Testing and treatment
Healthcare providers test for mucormycosis by taking samples of affected tissue, fluid from the lungs, or nasal discharge. Samples are tested at a laboratory.
Antifungal medications are needed to treat mucormycosis. Sometimes surgery is needed to cut and remove infected tissues.
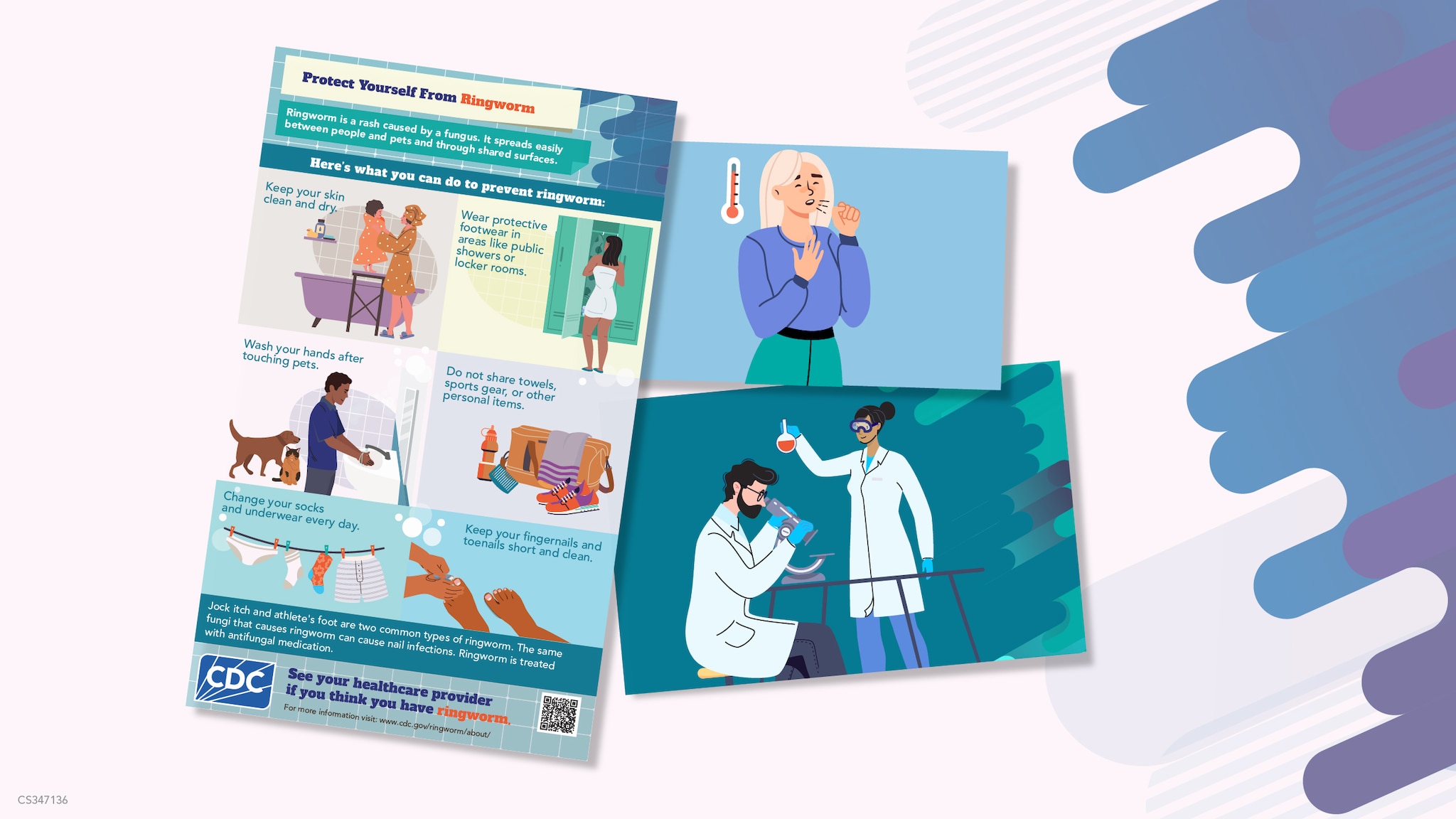
More on fungal diseases
Communication and Educational Materials
Webinars, Podcasts, and Clinical Tools