Vital Signs: Improvements in Maternity Care Policies and Practices That Support Breastfeeding — United States, 2007–2013
Weekly
October 9, 2015 / 64(39);1112-7On October 6, 2015, this report was posted as an MMWR Early Release on the MMWR website (http://www.cdc.gov/mmwr).
, PhD1; , PhD1; , MS2; , MPH1; , MLIS1; , PhD3; , PhD1
Abstract
Background: Although 80% of U.S. mothers begin breastfeeding their infants, many do not continue breastfeeding as long as they would like to. Experiences during the birth hospitalization affect a mother's ability to establish and maintain breastfeeding. The Baby-Friendly Hospital Initiative is a global program launched by the World Health Organization and the United Nations Children's Fund, and has at its core the Ten Steps to Successful Breastfeeding (Ten Steps), which describe evidence-based hospital policies and practices that have been shown to improve breastfeeding outcomes.
Methods: Since 2007, CDC has conducted the biennial Maternity Practices in Infant Nutrition and Care (mPINC) survey among all birth facilities in all states, the District of Columbia, and territories. CDC analyzed data from 2007 (baseline), 2009, 2011, and 2013 to describe trends in the prevalence of facilities using maternity care policies and practices that are consistent with the Ten Steps to Successful Breastfeeding.
Results: The percentage of hospitals that reported providing prenatal breastfeeding education (range = 91.1%–92.8%) and teaching mothers breastfeeding techniques (range = 87.8%–92.2%) was high at baseline and across all survey years. Implementation of the other eight steps was lower at baseline. From 2007 to 2013, six of these steps increased by 10–21 percentage points, although limiting non–breast milk feeding of breastfed infants and fostering post-discharge support only increased by 5–6 percentage points. Nationally, hospitals implementing more than half of the Ten Steps increased from 28.7% in 2007 to 53.9% in 2013.
Conclusions: Maternity care policies and practices supportive of breastfeeding are improving nationally; however, more work is needed to ensure all women receive optimal breastfeeding support during the birth hospitalization.
Implications for Public Health Practice: Because of the documented benefits of breastfeeding to both mothers and children, and because experiences in the first hours and days after birth help determine later breastfeeding outcomes, improved hospital policies and practices could increase rates of breastfeeding nationwide, contributing to improved child health.
Introduction
The American Academy of Pediatrics recommends that infants be exclusively breastfed (i.e., breast milk with no solids or other liquids except vitamin/mineral supplements or medications) for about the first 6 months of life, and that they continue to be breastfed for at least 12 months, with introduction of nutrient-rich complementary foods at about age 6 months (1). Eighty percent of infants in the United States begin breastfeeding (2); however, by age 6 months, just over half of all infants are receiving any breast milk, and only 21.9% exclusively breastfeed for the recommended first 6 months of life (2). These low rates of exclusive and continued breastfeeding have implications for public health: babies who are breastfed are at a reduced risk for ear, respiratory, and gastrointestinal infections; asthma; sudden infant death syndrome; and necrotizing enterocolitis (3,4). In addition, evidence suggests that breastfeeding is associated with a reduction in the risk for obesity and diabetes in children (3). Mothers who breastfeed have a reduced risk for breast and ovarian cancers, diabetes, and cardiovascular disease (3,5). The health effects for both mothers and infants from suboptimal breastfeeding rates contribute substantially to health care costs (6,7).
Sixty percent of mothers who stopped breastfeeding during the first year reported that they stopped earlier than they desired (8). Lactation is a time-sensitive physiologic process, and experiences in the first hours and days after birth affect a mother's ability to continue breastfeeding after she leaves the hospital (9). Recognizing this, in 1991, the World Health Organization (WHO) and United Nations Children's Fund (UNICEF) established the Baby-Friendly Hospital Initiative. To be designated as Baby-Friendly, a hospital must implement the Ten Steps to Successful Breastfeeding (Ten Steps) and comply with the International Code of Marketing of Breast-milk Substitutes, which requires hospitals to pay fair market value for infant formula and not promote items detrimental to breastfeeding (10). The Ten Steps outline evidence-based maternity care policies and practices that have been shown to increase rates of breastfeeding initiation, duration, and exclusivity (11,12). The American Academy of Pediatrics endorsed the Ten Steps in 2009.* In 2011 CDC produced a Vital Signs report showing hospital adherence to the Tens Steps in 2007 and 2009 (13); this report updates that information with additional data from 2011 and 2013.
Methods
Since 2007, CDC has conducted the biennial Maternity Practices in Infant Nutrition and Care (mPINC) survey, under contract with Battelle, to characterize U.S. maternity practices related to breastfeeding. The mPINC survey is a census administered to all birth facilities in all states, the District of Columbia, and U.S. territories (states). The response rate for the mPINC surveys to date has exceeded 80%, with 2,665–2,742 facilities participating in each survey. Approximately 95% of participating facilities are hospitals, and the remainder are freestanding birth centers; in this report, the term "hospital" is used to refer to all facilities. For each survey cycle, the mPINC survey is sent to a member of the hospital staff who is identified during a screening telephone call as the person best able to answer questions about the hospital's routine maternity care and infant feeding practices. Respondents are encouraged to obtain input from other key staff in completing the survey. Each participating hospital receives an individualized report† showing how its practices compare with other hospitals nationally, in the same state, and of a similar size.
CDC identified 10 indicators in the mPINC survey consistent with WHO/UNICEF's Ten Steps to Successful Breastfeeding. These indicators are 1) existence of a model breastfeeding policy, 2) staff competency assessment, 3) prenatal breastfeeding education, 4) early initiation of breastfeeding, 5) teaching breastfeeding techniques, 6) limited provision of non–breastmilk fluids for healthy breastfed infants, 7) rooming-in, 8) teaching feeding cues, 9) limited use of pacifiers, and 10) post-discharge support. CDC calculated the percentage of hospitals implementing these steps in 2007 (baseline), 2009, 2011, and 2013 to describe trends in U.S. maternity care policies and practices that support breastfeeding and, among hospitals with complete data for all Ten Steps (n = 2,181–2,479), the percentage implementing more than half of the Ten Steps, nationally and by state. In the U.S. territories other than Puerto Rico, only one to three hospitals exist; because CDC does not share hospital identifiable information publicly, data from American Samoa, Guam, the Northern Mariana Islands, and the Virgin Islands are presented in aggregate as "island territories." In 2007, only one island territory hospital had data on all of the Ten Steps; therefore, the percentage of island territory hospitals implementing more than half of the Ten Steps is not presented for 2007. Thus a total of 52 states were included in the state-level analysis in 2007, and 53 states were included in all other survey years. No inferential statistics were calculated, as mPINC is a census, not a sample.
Results
At baseline and across survey years, most U.S. hospitals reported providing prenatal breastfeeding education (range = 91.1%–92.8%) and teaching mothers breastfeeding techniques (range = 87.8%–92.2%) (Table). Reported implementation of the eight other steps was lower at baseline. For six of these steps, substantial improvement in reported hospital implementation occurred from 2007 to 2013, including having a model breastfeeding policy (11.7% to 26.3%), assessment of staff competency (44.6% to 60.2%), early initiation of breastfeeding (43.5% to 64.8%), rooming-in (30.8% to 44.8%), teaching feeding cues (77.0% to 87.3%), and limiting use of pacifiers (25.3% to 45.0%). However, less progress occurred in limiting non–breast milk feeding of breastfed infants (20.6% to 26.4%), and in providing optimal post-discharge support (26.8% to 32.2%). Nationally, the percentage of hospitals reporting implementing more than half of the Ten Steps increased from 28.7% in 2007 to 53.9% in 2013, and this increase was reported across states. From 2007 to 2013 the number of states with ≥60% of hospitals implementing more than half of the steps increased from 4 to 21 (Figure). In contrast, the number of states with <20% of hospitals implementing more than half of the steps decreased from 15 to 0.
Conclusion and Comments
From 2007 to 2013, several key aspects of maternity care supportive of breastfeeding have shown consistent improvement. Individualized mPINC reports sent to each participating hospital compare the hospitals' maternity care policies and practices with recommended standards, describe the evidence behind these standards, and identify improvement opportunities. Dissemination of these individualized reports, as well as dissemination of surveillance data from the mPINC survey, including state reports§ and key publications (13), might have contributed to these improvements in maternity care practices. The Surgeon General's Call to Action to Support Breastfeeding,¶ the National Prevention Strategy,** and the addition of maternity care objectives to Healthy People 2020†† have also helped increase focus on the importance of maternity care in helping women establish breastfeeding.
A variety of other efforts are also likely contributing to the observed improvements in maternity care. As stated earlier, to be designated as Baby-Friendly, a hospital must implement the Ten Steps to Successful Breastfeeding and comply with the International Code of Marketing of Breast-milk Substitutes (10). In 2011, as part of the First Lady's Let's Move! in Indian Country campaign, the Indian Health Service committed to achieving Baby-Friendly designation for all 13 of its federal maternity hospitals, a goal that was recently achieved.§§ Under a cooperative agreement with CDC, the National Institute for Children's Health Quality led the Best Fed Beginnings project, which helped 89 hospitals from 29 states work toward Baby-Friendly designation. This effort recruited hospitals with a large number of annual births and which serve populations with lower breastfeeding rates. As of August 2015, 50 of these hospitals have been designated Baby-Friendly and approximately 155,000 additional babies are now born in Baby-Friendly hospitals each year.¶¶ Through funding agreements and technical assistance, CDC also supports state health departments in improving maternity care practices; currently 33 states are using CDC funds to improve maternity care practices that support breastfeeding.
Despite substantial improvement, as of 2013, implementation of several of these maternity care practices and policies was far from optimal. Just over one quarter of hospitals have a model breastfeeding policy, which is the foundation for many of the other steps. In addition, fewer than half of hospitals reported routinely keeping healthy infants with their mothers throughout the hospital stay, a practice that allows mothers to become more familiar with their babies' hunger cues, and increases opportunities for breastfeeding (12).
This report also describes two key indicators that were low at baseline and showed less progress: limiting the provision of fluids other than breast milk to healthy breastfed infants and the provision of optimal post-discharge support. The provision of non–breast milk fluids to healthy breastfed infants has been associated with suboptimal breastfeeding behaviors, shorter breastfeeding duration, and mothers being less likely to meet their own breastfeeding intentions (14,15). The percentage of hospitals that limited giving fluids other than breast milk to health breastfed infants increased from 20.6% in 2007 to 26.4% in 2013. In recognizing the provision of non–breast milk fluids to breastfed infants as a quality-of-care issue, in 2010, The Joint Commission, a major organization that accredits and certifies U.S. hospitals, added exclusive breast milk feeding during the newborn's entire hospitalization as a new quality of care measure. In 2014 The Joint Commission required reporting of this measure by all hospitals with ≥1,100 births per year, and as of January 2016, will require reporting by all hospitals with ≥300 births per year, thus encompassing approximately 80% of all birth hospitals.*** Reporting of this measure might help increase awareness of the importance of exclusive breastfeeding, and reduce hospital provision of non–breast milk fluids to breastfeeding infants when there is no medical indication for it.
From 2007 to 2013, the percentage of hospitals providing adequate post-discharge support increased by only 20%. Problems with breastfeeding, such as trouble getting the baby to latch, pain, and a perception of insufficient milk, are common among new mothers and are associated with shorter durations of breastfeeding (16). In a study of first-time mothers that assessed concerns with breastfeeding at several time points during the first 2 months of life, these problems were most pronounced at 3 and 7 days postpartum (16), which is after most women have left the hospital, but before they might be connected to other types of community support. These early breastfeeding problems can often be overcome with early support and management. To receive this support, however, mothers need to have a continuum of care that extends from the hospital to other providers and programs in the first few weeks postpartum.
The findings in this report are subject to at least three limitations. First, the survey is completed by a key respondent on behalf of each hospital and might not accurately reflect the hospital practices assessed. However, to ensure that the data obtained were of highest quality possible, CDC requested that the survey be sent to the person most knowledgeable about the hospital's maternity practices, and that it be completed in consultation with other knowledgeable persons. Second, although approximately 80% of hospitals participated in each survey, practices might differ between those that participated and those that did not. Third, the mPINC indicators included here are consistent with the Ten Steps to Successful Breastfeeding, but might not indicate implementation of each of the steps as required for Baby-Friendly designation.†††
The national improvements in maternity care supportive of breastfeeding from 2007 to 2013 are substantial; however, more work is needed to ensure that all women have access to evidence-based maternity care policies and practices supportive of breastfeeding. Currently, among the approximately four million babies born in the United States every year, only about 14% are born in Baby-Friendly hospitals, and as of August 2015, only 289 (9%) of the approximately 3,300 U.S. birth facilities were designated Baby-Friendly.§§§ Several CDC efforts are underway to continue supporting improvements in maternity care, including continuation of the mPINC survey, the EMPower breastfeeding project¶¶¶ to support up to 100 hospitals in achieving Baby-Friendly designation, and continued support of state health departments to support breastfeeding initiatives.
1Division of Nutrition, Physical Activity, and Obesity, National Center for Chronic Disease Prevention and Health Promotion, CDC; 2Battelle, Columbus, Ohio; 3Department of Nutrition for Health and Development, World Health Organization.
Corresponding author: Cria G. Perrine, cperrine@cdc.gov, 770-488-5183.
References
- Section on Breastfeeding. Breastfeeding and the use of human milk. Pediatrics 2012;129:e827–41.
- CDC. Breastfeeding among U.S. children born 2000–2012, CDC National Immunization Survey. Atlanta, GA: US Department of Health and Human Services, CDC; 2015. Available at http://www.cdc.gov/breastfeeding/data/NIS_data.
- Ip S, Chung M, Raman G, et al. Breastfeeding and maternal and infant health outcomes in developed countries. Evid Rep Technol Assess (Full Rep) 2007;153:1–186.
- Hauck FR, Thompson JM, Tanabe KO, Moon RY, Vennemann MM. Breastfeeding and reduced risk of sudden infant death syndrome: a meta-analysis. Pediatrics 2011;128:103–10.
- Schwarz EB, Ray RM, Stuebe AM, et al. Duration of lactation and risk factors for maternal cardiovascular disease. Obstet Gynecol 2009;113:974–82.
- Bartick M, Reinhold A. The burden of suboptimal breastfeeding in the United States: a pediatric cost analysis. Pediatrics 2010;125:e1048–56.
- Bartick MC, Stuebe AM, Schwarz EB, Luongo C, Reinhold AG, Foster EM. Cost analysis of maternal disease associated with suboptimal breastfeeding. Obstet Gynecol 2013;122:111–9.
- Odom EC, Li R, Scanlon KS, Perrine CG, Grummer-Strawn L. Reasons for earlier than desired cessation of breastfeeding. Pediatrics 2013;131:e726–32.
- DiGirolamo AM, Grummer-Strawn LM, Fein SB. Effect of maternity-care practices on breastfeeding. Pediatrics 2008;122(Suppl 2):S43–9.
- World Health Organization. International code of marketing of breast milk substitutes. Geneva, Switzerland: World Health Organization; 1981.
- Kramer MS, Chalmers B, Hodnett ED, et al.; PROBIT Study Group (Promotion of Breastfeeding Intervention Trial). Promotion of breastfeeding intervention trial (PROBIT): a randomized trial in the Republic of Belarus. JAMA 2001;285:413–20.
- World Health Organization. Evidence for the ten steps to successful breastfeeding. Geneva, Switzerland: World Health Organization; 1998.
- CDC. Vital signs: hospital practices to support breastfeeding—United States, 2007 and 2009. MMWR Morb Mortal Wkly Rep 2011;60:1020–5.
- Dewey KG, Nommsen-Rivers LA, Heinig MJ, Cohen RJ. Risk factors for suboptimal infant breastfeeding behavior, delayed onset of lactation, and excess neonatal weight loss. Pediatrics 2003;112:607–19.
- Perrine CG, Scanlon KS, Li R, Odom E, Grummer-Strawn LM. Baby-Friendly hospital practices and meeting exclusive breastfeeding intention. Pediatrics 2012;130:54–60.
- Wagner EA, Chantry CJ, Dewey KG, Nommsen-Rivers LA. Breastfeeding concerns at 3 and 7 days postpartum and feeding status at 2 months. Pediatrics 2013;132:e865–75.
* Available at http://www2.aap.org/breastfeeding/files/pdf/TenStepswosig.pdf ![]()
![]() .
.
† Available at http://www.cdc.gov/breastfeeding/pdf/mpinc/sample-benchmark-report.pdf ![]() .
.
§ Available at http://www.cdc.gov/breastfeeding/data/mpinc/state_reports.html.
¶ Available at http://www.surgeongeneral.gov/library/calls/breastfeeding/calltoactiontosupportbreastfeeding.pdf ![]()
![]() .
.
** Available at http://www.surgeongeneral.gov/priorities/prevention/strategy/healthy-eating.pdf ![]()
![]() .
.
†† Available at http://www.healthypeople.gov/2020/topics-objectives/topic/maternal-infant-and-child-health/objectives![]() .
.
§§ Available at http://www.ihs.gov/newsroom/pressreleases/2014pressreleases/all13ihsobstetricfacilitiesdesignatedbabyfriendly![]() .
.
¶¶ Available at http://www.nichq.org/sitecore/content/breastfeeding/breastfeeding/solutions/best-fed-beginnings![]() .
.
*** Available at http://www.jointcommission.org/assets/1/23/jconline_June_24_2015.pdf ![]()
![]() .
.
††† Available at https://www.babyfriendlyusa.org/get-started/the-guidelines-evaluation-criteria![]() .
.
§§§ Available at https://www.babyfriendlyusa.org/find-facilities/designated-facilities–by-state![]() .
.
¶¶¶ Available at http://empowerbreastfeeding.org![]() .
.
|
Key Points |
|
FIGURE. Percentage of hospitals implementing more than half of the Ten Steps to Successful Breastfeeding,* by state or jurisdiction — Maternity Practices in Infant Nutrition and Care (mPINC) Survey, United States, 2007–2013
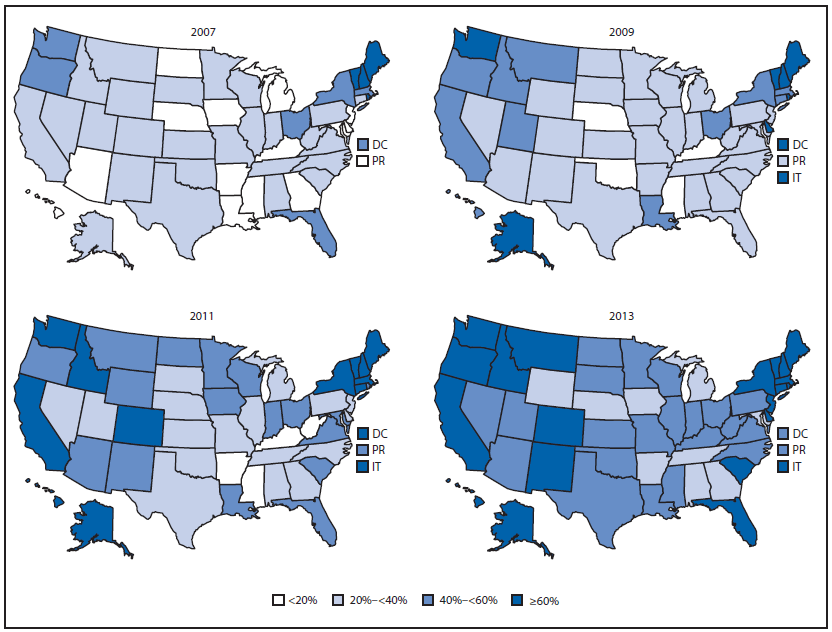
Abbreviations: DC = District of Columbia; IT = Island Territories, including American Samoa, Guam, Northern Mariana Islands, and Virgin Islands; PR = Puerto Rico.
* These are mPINC indicators consistent with the Ten Steps to Successful Breastfeeding as described in the table.
Alternate Text: The figure above contain four maps of the United States showing the percentage of U.S. hospitals implementing more than half of the Ten Steps to Successful Breastfeeding, by state or jurisdiction, in 2007, 2009, 2011, and 2013.
Use of trade names and commercial sources is for identification only and does not imply endorsement by the U.S. Department of
Health and Human Services.
References to non-CDC sites on the Internet are
provided as a service to MMWR readers and do not constitute or imply
endorsement of these organizations or their programs by CDC or the U.S.
Department of Health and Human Services. CDC is not responsible for the content
of pages found at these sites. URL addresses listed in MMWR were current as of
the date of publication.
All MMWR HTML versions of articles are electronic conversions from typeset documents.
This conversion might result in character translation or format errors in the HTML version.
Users are referred to the electronic PDF version (http://www.cdc.gov/mmwr)
and/or the original MMWR paper copy for printable versions of official text, figures, and tables.
An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S.
Government Printing Office (GPO), Washington, DC 20402-9371;
telephone: (202) 512-1800. Contact GPO for current prices.
**Questions or messages regarding errors in formatting should be addressed to
mmwrq@cdc.gov.


