Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail.
Progress Toward Measles Elimination — Western Pacific Region, 2009–2012
In 2005, the World Health Organization (WHO) Regional Committee for the Western Pacific Region (WPR) resolved that WPR should aim to eliminate measles* by 2012 (1). The recommended measles elimination strategies (2) in WPR include 1) achieving and maintaining high (≥95%) coverage with 2 doses of measles-containing vaccine (MCV) through routine immunization services and by implementing supplementary immunization activities (SIAs), when required; 2) conducting high-quality, case-based measles surveillance; 3) ensuring high-quality laboratory surveillance, with timely and accurate testing of specimens to confirm or discard suspected cases and detect measles virus for genotyping and molecular analysis; and 4) establishing and maintaining measles outbreak preparedness for rapid response and ensuring appropriate case management. This report updates the previous report (3) and describes progress toward eliminating measles in WPR during 2009–2012. During this period, measles incidence reached a historic low, decreasing by 83%, from 34.0 to 5.9 cases per million population. However, to achieve measles elimination in WPR, additional efforts are needed to strengthen routine immunization services in countries and areas with <95% coverage with the routine first (MCV1) or second dose of MCV (MCV2), to introduce a MCV2 dose in the four remaining countries and areas that do not yet have a routine 2-dose MCV schedule, and to use SIAs to close immunity gaps among measles-susceptible populations in countries and areas that have ongoing measles virus transmission.
Immunization Activities
Annual data on MCV coverage are reported from 36 of the 37 WPR countries and areas to WHO and the United Nations Children's Fund (UNICEF).† MCV1 coverage in WPR increased from 96% in 2009 to 98% in 2012. The number of countries with ≥95% MCV1 coverage increased from 12 (33%) in 2009 to 15 (42%) in 2012. MCV1 was administered at 8 months in one (3%), at age 9 months in six (17%),§ at age 10 months in one (3%), at age 12 months in 24 (67%), and at age >12 months in four (11%) (Table 1).
The number of countries and areas that provide routine MCV2 increased from 32 (89%) in 2009 to 33 (92%) in 2012, and the number reporting ≥95% MCV2 coverage increased from 10 (28%) in 2009 to 11 (31%) in 2012. Among the 33 countries and areas reporting MCV2 coverage in 2012, the scheduled age of MCV2 administration ranged from 12 months to 7 years. During 2009–2012, approximately 226 million children were vaccinated during 16 measles SIAs (Table 2); of these, seven (44%) SIAs included rubella vaccine, and 10 (63%) added at least one other child health intervention.
Surveillance Activities
During 2009–2012, measles case-based surveillance was conducted in all 37 WPR countries and areas, including 14 countries and two areas that report data individually, and 21 countries and areas of the Pacific Islands that report data as one epidemiologic block.¶ Measles surveillance data are reported monthly to WHO and supported by 385 laboratories participating in the WHO Global Measles and Rubella Laboratory Network** (4). Suspected measles cases were confirmed based on laboratory findings, an epidemiologic link, or clinical criteria.†† Key indicators of surveillance performance include 1) the number of suspected measles cases discarded as nonmeasles (target: ≥2 per 100,000 population); 2) the proportion of second-level administrative units with ≥1 nonmeasles discarded case per 100,000 population (target: ≥80%); 3) the percentage of suspected measles cases with adequate investigation that includes all essential data elements§§ (target: ≥80%); 4) the percentage of suspected measles cases with adequate specimens collected within 28 days of rash onset (target: ≥80%, excludes epidemiologically linked cases) (5); and 5) the percentage of specimens with laboratory results available within 7 days after receipt in the laboratory (target: ≥80%). The number of countries and areas with adequate data that met the target for suspected cases discarded as nonmeasles per 100,000 population increased from seven (50%) of 14 in 2009 to nine (64%) of 14 in 2012 (Table 3). From 2009 to 2012, suspected cases with adequate investigations increased from 38% to 89%, suspected cases with adequate specimens collected for laboratory testing increased from 79% to 93%, and the proportion of blood specimens received by the laboratory with results available within 7 days increased from 55% to 96% (Table 3).
Measles Disease Incidence and Measles Virus Genotypes
From 2009 to 2012, confirmed measles cases decreased 84%, from 54,291 to 8,524, and confirmed measles incidence per million population decreased 83%, from 34.0 to 5.9 (Table 1). In 2012, the highest confirmed measles incidence was reported from Malaysia (63.7 per million), the Philippines (15.9 per million), and New Zealand (12.3 per million) (Table 1). The highest number of confirmed cases was reported from China and decreased 88%, from 52,461 in 2009 to 6,183 in 2012 (Figure). During 2009–2012, the predominant measles virus genotypes detected in WPR were H1 in China, D9 in the Philippines, Malaysia, and Singapore; and D8 in Malaysia. Other measles virus genotypes that were identified and determined to have been related to measles virus importations from outside WPR included B3, D4, and G3.
Reported by
W. William Schluter, MD, Wang Xiaojun, MD, Jorge Mendoza-Aldana, MD, Youngmee Jee, MD, PhD, Sergey Diorditsa, MD, PhD, Expanded Programme on Immunization, World Health Organization Western Pacific Regional Office, Manila, Philippines. Alya Dabbagh, PhD, Mick Mulders, PhD, Dept of Immunization, Vaccines, and Biologicals, World Health Organization, Geneva, Switzerland. Div of Viral Diseases, National Center for Immunization and Respiratory Diseases; Christopher Gregory, MD, James L. Goodson, MPH, Global Immunization Div, Center for Global Health, CDC. Corresponding contributor: James L. Goodson, jgoodson@cdc.gov, 404-639-8170.
Editorial Note
In 2012, the WPR Regional Committee reaffirmed its commitment to eliminate measles and urged member states to interrupt all residual endemic measles virus transmission as rapidly as possible (6). To achieve elimination, intensified efforts are needed to identify and close gaps in population immunity, by increasing coverage with MCV2 to ≥95% in all countries and areas and by conducting high-quality SIAs in countries with sustained measles virus transmission (e.g., China, Malaysia, and the Philippines). In countries and areas with <95% MCV1 or MCV2 coverage, urgent action is needed to strengthen routine immunization services and to identify and implement targeted SIAs for measles-susceptible populations. In the four remaining countries and areas (Lao People's Democratic Republic, Papua New Guinea, Solomon Islands, and Vanuatu) that do not provide MCV2 in the routine childhood vaccination schedule, strategies are needed to increase MCV1 coverage, conduct periodic SIAs to provide a second opportunity for all birth cohorts to receive MCV, and prepare for introduction of routine MCV2.
The WPR Guidelines on Verification of Measles Elimination (7) were finalized in March 2013; progress toward measles elimination in WPR will be monitored by the Regional Verification Commission through annual progress reports from each country or area and from the Pacific Islands countries and areas reporting as one epidemiologic block. High-quality case-based measles surveillance is critical to the verification process. Despite overall improvement in measles surveillance performance, gaps persist, as reflected by the low proportion of second-level administrative units with one or more nonmeasles discarded case per 100,000 population. Additionally, incomplete investigations of suspected measles cases in some countries challenge efforts to rapidly identify and respond to outbreaks and to measure and document progress toward elimination. For example, in Vietnam, only six (0.8%) of the 771 suspected measles cases with specimens available for testing reported in 2012 were laboratory confirmed. However, 631 additional cases did not have specimens collected but were reported as clinically confirmed measles. The sensitivity of the measles surveillance system in other countries with discarded nonmeasles reporting rates of <2 per 100,000 population might be insufficient to rapidly detect and respond to outbreaks or to meet verification criteria.
The WHO Global Vaccine Action Plan calls for the elimination of rubella and congenital rubella syndrome in five of the six WHO regions by 2020 (8). In April 2012, the Measles and Rubella Initiative launched the 2012–2020 Global Measles and Rubella Strategic Plan to integrate rubella with measles elimination efforts (9). Rubella-containing vaccine is not provided in six WPR countries and areas; five of these countries (Cambodia, Lao People's Democratic Republic, Papua New Guinea, Solomon Islands, and Vietnam) are eligible for financial support offered by the GAVI Alliance to conduct a wide-age-range SIA using combined measles-rubella vaccine followed by the introduction of rubella vaccine in their national routine immunization programs. In addition to contributing to rubella elimination, these SIAs would provide a unique opportunity to boost population immunity to measles and contribute momentum to achieve and sustain measles elimination in WPR.
References
- World Health Organization, Regional Committee for the Western Pacific. Resolution WPR/RC56.R8: measles elimination, hepatitis B control, and poliomyelitis eradication. Manila, Philippines: World Health Organization; 2005. Available at http://www2.wpro.who.int/rcm/en/archives/rc56/rc_resolutions/wpr_rc56_r08.htm.
- World Health Organization, Regional Office for the Western Pacific. Western Pacific Region measles elimination field guide (2013 version). Manila, Philippines: World Health Organization; 2013 (in press).
- World Health Organization. Progress towards the 2012 measles elimination goal in the WHO's Western Pacific Region, 1990–2008, Wkly Epidemiol Rec 2009;84:271–9.
- Featherstone DA, Rota PA, Icenogle J, et al. Expansion of the global measles and rubella laboratory network 2005-09. J Infect Dis 2011;204(Suppl 1):S491–8.
- World Health Organization. Framework for verifying elimination of measles and rubella. Wkly Epidemiol Rec 2013;88:89–99.
- World Health Organization, Regional Committee for the Western Pacific. Resolution WPR/RC63.5: elimination of measles and acceleration of rubella control. Hanoi, Vietnam: World Health Organization; 2012. Available at http://www.wpro.who.int/about/regional_committee/63/resolutions/wpr_rc63_r5_measles_elimination_03oct.pdf.
- World Health Organization, Regional Office for the Western Pacific. Western Pacific Region guidelines on verification of measles elimination (2013 version). Manila, Philippines: World Health Organization; 2013 (in press).
- World Health Organization. Global vaccine action plan: report by the Secretariat. Geneva, Switzerland: World Health Organization; 2012. Available at http://apps.who.int/gb/ebwha/pdf_files/wha65/a65_22-en.pdf.
- World Health Organization. Global measles and rubella strategic plan: 2012–2020. Geneva, Switzerland: World Health Organization; 2012. Available at http://www.who.int/immunization/newsroom/Measles_Rubella_StrategicPlan_2012_2020.pdf.
* Measles elimination is defined as the absence of endemic measles virus transmission in a defined geographic area (e.g., region or country) for ≥12 months in the presence of a well-performing surveillance system.
† The Pitcairn Islands, with a population of approximately 50 persons, does not report immunization coverage data to WHO/UNICEF.
§ Papua New Guinea also provides a supplementary dose of MCV at age 6 months.
¶ The epidemiologic block of the Pacific Islands countries and areas includes American Samoa, Cook Islands, Fiji, French Polynesia, Guam, Kiribati, the Marshall Islands, the Federated States of Micronesia, Nauru, New Caledonia, Niue, the Commonwealth of the Northern Mariana Islands, Palau, the Pitcairn Islands, Samoa, Solomon Islands, Tokelau, Tonga, Tuvalu, Vanuatu, and Wallis and Futuna.
** This network includes one WHO global specialized laboratory in Japan, three regional reference laboratories (in Melbourne, Australia; Beijing, China; and Hong Kong, China), 19 national or subnational laboratories, and 31 provincial and 331 prefecture-level laboratories in China.
†† Cases that meet the WHO clinical case definition of measles for which no adequate specimen was collected and cannot be epidemiologically linked to a laboratory-confirmed case of measles.
§§ Essential data elements include name or identifier, date of birth or age, sex, place of residence, vaccination status or date of last vaccination, date of rash onset, date of notification, date of investigation, date of specimen collection, and place of infection or travel history.
What is already known on this topic?
The World Health Organization (WHO) Regional Committee for the Western Pacific Region (WPR) has resolved to eliminate measles by 2012. Substantial progress had been made in reducing the burden from measles by most countries in the region by 2008. The number of reported measles cases in WPR (excluding China) decreased 86%, from 106,172 (255.6 per million population) in 2000 to 14,724 (32.6 per million population) in 2008.
What is added by this report?
This report updates the previous report that summarized progress during 1990–2008 and describes progress toward measles elimination in WPR during 2009–2012. During this period, measles incidence in the region reached a historic low, decreasing by 83%, from 34.0 to 5.9 cases per million population. In China, a nationwide measles vaccination campaign was implemented in 2010 and reported confirmed measles cases decreased 88%, from 52,461 in 2009 to 6,183 in 2012.
What are the implications for public health practice?
Despite the progress to date, achieving measles elimination in WPR will require additional efforts. These include 1) introducing a routine second dose of measles-containing vaccine (MCV) in the four remaining countries and areas that do not yet have a routine 2-dose MCV schedule; 2) strengthening routine immunization services in countries and areas with <95% coverage with the routine first or second dose of MCV; and 3) closing immunity gaps through supplementary immunization activities in measles-susceptible populations in countries and areas that have ongoing measles virus transmission.
FIGURE. Confirmed measles cases,* by month of rash onset — World Health Organization Western Pacific Region (WPR), 2009–2012
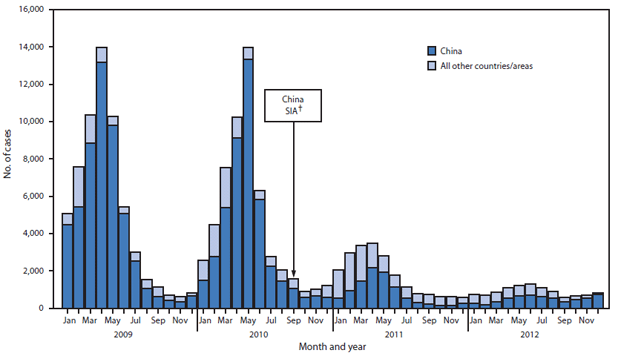
Abbreviation: SIA = supplementary immunization activity.
* Confirmed measles cases reported by countries and areas to World Health Organization. A case of measles is confirmed by serology when measles-specific immunoglobulin M antibody is detected in a person who was not vaccinated in the previous 30 days. A case of measles is confirmed by epidemiologic linkage when linked in time and place to a laboratory-confirmed measles case but lacks serologic confirmation. During 2009–2012, a case of measles meeting the case definition but without a specimen collected could be reported as clinically confirmed.
† SIA conducted in China in which approximately 100 million children aged 8–179 months were vaccinated against measles, with targeted age group varying by province.
Alternate Text: The figure above shows confirmed measles cases, by month of rash onset for the World Health Organization's Western Pacific Region during 2009-2012. The highest number of confirmed cases was reported from China and decreased 88%, from 52,461 in 2009 to 6,183 in 2012.
Use of trade names and commercial sources is for identification only and does not imply endorsement by the U.S. Department of
Health and Human Services.
References to non-CDC sites on the Internet are
provided as a service to MMWR readers and do not constitute or imply
endorsement of these organizations or their programs by CDC or the U.S.
Department of Health and Human Services. CDC is not responsible for the content
of pages found at these sites. URL addresses listed in MMWR were current as of
the date of publication.
All MMWR HTML versions of articles are electronic conversions from typeset documents.
This conversion might result in character translation or format errors in the HTML version.
Users are referred to the electronic PDF version (http://www.cdc.gov/mmwr)
and/or the original MMWR paper copy for printable versions of official text, figures, and tables.
An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S.
Government Printing Office (GPO), Washington, DC 20402-9371;
telephone: (202) 512-1800. Contact GPO for current prices.
**Questions or messages regarding errors in formatting should be addressed to
mmwrq@cdc.gov.


