Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail.
Take-Home Lead Exposure Among Children with Relatives Employed at a Battery Recycling Facility — Puerto Rico, 2011
Please note: An erratum has been published for this article. To view the erratum, please click here.
Weekly
November 30, 2012 / 61(47);967-970The recycling of lead has increased during the past 20 years, with more workers and their families potentially being exposed to lead from recycling facilities, including facilities that recycle lead-acid batteries. During November 2010–May 2011, four voluntary blood lead screening clinics for children of employees of a battery recycling facility in Puerto Rico were conducted. A total of 227 persons from 78 families had blood lead tests. Among 68 children aged <6 years, 11 (16%) had confirmed blood lead levels (BLLs) ≥10 µg/dL, the BLL at which CDC recommended individual intervention to reduce BLLs in 2010 (1), and 39 (57%) children aged <6 years had venous or capillary BLLs ≥5 µg/dL, the reference value for elevated BLLs in children established by CDC in 2012 (2). To determine whether take-home lead exposure contributed to the children's BLLs of ≥10 µg/dL, vehicle and household environmental samples were collected and analyzed. Eighty-five percent of vehicle dust samples and 49% of home dust samples exceeded the U.S. Environmental Protection Agency (EPA) level of concern of ≥40 µg/ft2 (3.7 µg/m2). EPA began clean-up of employee homes and vehicles, focusing first on homes with children with BLLs ≥10 µg/dL. EPA also required that the company set up shower facilities, shoe washes, and clean changing areas at the battery recycling facility. Lastly, CDC assigned a case manager to provide education, environmental follow-up, and case management of all children with BLLs ≥5 µg/dL. On average, children's BLLs have decreased 9.9 µg/dL since being enrolled in case management.
The Puerto Rico Department of Health (PRDOH), CDC, and EPA conducted a child blood lead prevalence survey in Puerto Rico during 2010. Head Start, an early education program for low-income children, requires blood lead screening of all enrollees (3). As part of this survey, blood lead testing data from the island-wide Head Start program were reviewed. Three children with BLLs ≥10 µg/dL were found to have a common link: a relative employed by a local battery recycling facility. At the beginning of the investigation, approximately 150 persons were employed at this facility, the only known legal battery recycling smelter in the Caribbean. To learn whether additional children were affected, PRDOH and CDC conducted a voluntary blood lead screening clinic in November 2010 for the employees' children aged ≤7 years. Among 14 children tested, five had BLLs ≥10 µg/dL, and five had BLLs 5–9 µg/dL.
Three additional blood lead screening clinics for workers and their families were conducted during April–May 2011. Workers were invited to participate in the screening clinics via company announcements included with their paychecks. A total of 227 persons (approximately half of all company employees) from 78 families had blood lead tests; 126 were capillary specimens from children, and 101 were venous specimens from adults. All blood specimens initially were tested using the LeadCare II (Magellan Diagnostics; Billerica, Massachusetts) portable blood lead analyzer. Confirmatory venous blood specimens were collected from participants with capillary BLLs ≥10 µg/dL and were analyzed by a CDC laboratory using inductively coupled plasma mass spectroscopy.
Among 68 children aged <6 years, 11 (16%) had confirmed BLLs ≥10 µg/dL, and 28 (41%) had BLLs 5–9 µg/dL (Figure). Additionally, four (7%) of 56 children aged 6–17 years, and 44 (42%) of 105 adults aged 18–68 years also had confirmed BLLs ≥10 µg/dL. Among the children aged <6 years with BLLs ≥10 µg/dL, one (9%) had a BLL ≥25 µg/dL. Six pregnant and/or lactating women also were tested. All had venous BLLs ≤1.8 µg/dL.
Forty-eight (46%) adults tested in the April–May screening clinics were employees at the battery recycling facility. Forty-seven of the 48 employees tested were male. The most common job description was smelter worker (19 [40%]), average employee age was 30 years (range: 21–40 years), and average length of employment was 28 months (range: 1–96 months). The average employee BLL was 30.7 µg/dL (range: 3.2–72.0 µg/dL), and 33 (69%) had a BLL ≥25 on their initial test (Table 1). Employees continue to have blood lead testing by the company and by their private health-care providers.
PRDOH and CDC notified EPA of potential for take-home lead exposure among children of workers of the facility. EPA initiated investigations into the recycling, transportation, treatment, storage, and disposal of lead under various authorities, including the Resource Conservation and Recovery Act, the Comprehensive Environmental Response, Compensation, and Liability Act (also known as Superfund), the Clean Air Act, and the Emergency Planning and Community Right to Know Act. These acts give EPA various authorities to protect human health and the environment.
To establish whether take-home lead exposure contributed to children's BLLs ≥10 µg/dL, EPA collected and analyzed household environmental samples for lead. Lead levels exceeding the EPA level of concern on wipe samples were common in employee homes and vehicles. Forty-eight employee homes and 43 associated vehicles were initially tested for lead beginning in April 2011. Lead in all 15 tap water samples collected in the homes was present at values below the EPA action level of <15 parts per billion. Eighty-five percent (136 of 159) of vehicle dust samples and 49% (209 of 428) of home dust samples exceeded the EPA level of concern (≥40 µg/ft2) (Table 2). In comparison, a study of dust floor composite samples collected during an island-wide, cross-sectional blood lead prevalence study in 2010 found only one (0.4%) of 235 households had a lead level exceeding the EPA level of concern on wipe samples (CDC, unpublished data, 2010). The high proportion of dust samples from employee vehicles and homes with elevated lead levels suggests that lead brought home by employees caused elevated BLLs among family members. Comparing the mean dust lead level in 18 households with a total of 24 children aged <6 years with BLLs ≥5 µg/dL with the mean dust lead level in 16 households with a total of 18 children aged <6 years with BLLs <5 µg/dL showed that the mean dust lead level in the 18 households was 179.2 µg/ft2, whereas the level in the 16 houses was 48.6 µg/ft2 (t=-3.00, p=0.007).
The initial findings were shared with the facility and employees during early 2011. Additional current and former employees sought or were contacted by EPA for lead testing of homes and vehicles. EPA began clean-up of employee homes and vehicles during May 2011, focusing first on homes with children with BLLs ≥10 µg/dL. As of October 30, 2012, EPA staff members and contractors had sampled 188 current and former employee homes and 268 vehicles. Of those homes and vehicles requiring decontamination, 147 (78%) homes and 148 (55%) vehicles had been decontaminated and cleared. Additional testing and decontamination is ongoing and expected to continue throughout 2012.
Reported by
Brenda Rivera García, DVM, John Rullán, MD, Puerto Rico Dept of Health. Maureen O'Neill, MURP, Geoff Garrison, MSE, Dennis Santella, Mark M. Maddaloni, DrPH, Pat Evangelista, MSE, Argie Cirillo, US Environmental Protection Agency. Gredia Huerta-Montanez, MD, Carter Consulting, Inc., Atlanta, GA. Kathleen Caldwell, PhD, Div of Laboratory Sciences, Timothy Dignam, PhD, Mary Jean Brown, ScD, Div of Emergency and Environmental Health Svcs, National Center for Environmental Health, CDC. Corresponding contributor: Timothy Dignam, tdignam@cdc.gov, 770-488-3622.
Editorial Note
Lead is easily recycled and can be recycled repeatedly. If recycled and refined in appropriate facilities, the recycled product is as pure as lead produced from ore. In the United States, approximately 70% of lead is derived from recycled materials (mostly scrap lead-acid batteries), and 80% of the recycled lead produced is used in lead-acid batteries (4). The cost of lead produced from ore has increased because of rising global demand. In 1999, lead cost $963 per metric ton. During 2009, lead cost $1,920 per metric ton (5). Because the production of recycled lead has increased, more workers and their families are potentially exposed to lead from recycling facilities than in the past. As of January 2012, a total of 15 recycled lead smelters are operating in the United States and Puerto Rico (6).
Lead is a well-documented neurotoxin. In children, lead exposure is associated with decreased intelligence, impaired neurobehavioral development, attention deficit/hyperactivity disorder, anemia, increased dental caries, decreased growth, and impaired hearing (7). Recent research suggests that adverse health effects of BLLs <10 µg/dL in children extend beyond cognitive function to include cardiovascular, immunologic, and endocrine effects. No minimal blood lead threshold for adverse effects has been identified (2,7). In January 2012, CDC's Advisory Committee on Childhood Lead Poisoning Prevention recommended that CDC eliminate the use of the term "blood lead level of concern" (2). The committee recommended that a reference value based on the 97.5th percentile of the National Health and Nutrition Examination Survey–generated BLL distribution in children aged 1–5 years (currently 5 µg/dL) be used to identify children with elevated BLLs. In this investigation, 39 (57%) children aged <6 years had venous or capillary BLLs ≥5 µg/dL. In adults, moderate and low levels of exposure can increase blood pressure, decrease fertility, be nephrotoxic, cause cognitive dysfunction and adverse female reproductive and birth outcomes, and possibly have a carcinogenic effect (7,8).
Elevated BLLs among children caused by lead dust from battery recycling brought home by employees have been reported previously (9). One study reported that 42% of 91 children aged <6 years whose parents worked at a lead recycling smelter in Memphis, Tennessee, had BLLs ≥25 µg/dL (9). The apparent source of exposure was lead dust carried home on work clothing. A more recent study found that six children were exposed to lead dust in family vehicles and on child car seats (10). The sources of the lead dust were believed to be household contacts who worked in high-risk lead exposure occupations.
In the current investigation, lead brought into the home via contaminated work clothing and vehicles are the likely high dose sources of lead exposure. The percentage of children aged <6 years with BLLs ≥10 µg/dL found in this Puerto Rican community is markedly higher than that found during a population-based, cross-sectional blood lead prevalence study conducted during 2010. In that study, 440 children aged <7 years were tested for blood lead, and only three (0.7%) children had BLLs ≥10 µg/dL (CDC, unpublished data, 2010).
The findings in this report are subject to at least two limitations. First, environmental sampling is ongoing and not completed for all children with BLLs ≥5 µg/dL. Second, the persons tested were volunteers and might not be representative of all employees and their families.
To limit further lead contamination of employees' homes and vehicles, EPA required that the company set up shower facilities, shoe washes, and clean changing areas at the battery recycling facility. CDC, with support from PRDOH and EPA, has assigned a case manager to provide education, environmental follow-up, and case management of all children with BLLs ≥5 µg/dL. During 2012, CDC provided funding to state and local health departments to help ensure that infants and children with elevated BLLs receive medical and environmental follow-up. Outreach and education at the facility also has been provided by staff members of the PRDOH, CDC, and the Agency for Toxic Substances and Disease Registry. Lastly, CDC's National Institute for Occupational Safety and Health has been working closely with EPA and has begun a health hazard evaluation at the facility to assess employee exposure to lead.
References
- CDC. Preventing lead poisoning in young children. Atlanta, GA: US Department of Health and Human Services, CDC; 2005. Available at http://www.cdc.gov/nceh/lead/publications/prevleadpoisoning.pdf
 . Accessed November 20, 2012.
. Accessed November 20, 2012. - CDC. Low level lead exposure harms children: a renewed call for primary prevention. Atlanta, GA: US Department of Health and Human Services, CDC; 2012. Available at http://www.cdc.gov/nceh/lead/acclpp/final_document_030712.pdf
 . Accessed November 20, 2012.
. Accessed November 20, 2012. - Administration for Children and Families. Lead screening. Washington, DC: US Department of Health and Human Services, Administration for Children and Families, Office of Head Start; 2009. Available at http://eclkc.ohs.acf.hhs.gov/hslc/standards/IMs/2008/resour_ime_007_031208.html
 . Accessed November 20, 2012.
. Accessed November 20, 2012. - International Lead and Zinc Study Group. End uses of lead. Lisbon, Portugal: International Lead and Zinc Study Group; 2012. Available at http://www.ilzsg.org/static/enduses.aspx?from
 . Accessed November 20, 2012.
. Accessed November 20, 2012. - US Geological Survey. Historical statistics for mineral and material commodities in the United States. Denver, CO: US Geological Survey; 2011. Available at http://minerals.usgs.gov/ds/2005/140
 . Accessed November 20, 2012.
. Accessed November 20, 2012. - Environmental Protection Agency. National emissions standards for hazardous air pollutants from secondary lead smelting. 40 CFR Part 63. Federal Register 2012;77(3). Available at http://www.epa.gov/airtoxics/lead2nd/fr05ja12.pdf

 . Accessed November 20, 2012.
. Accessed November 20, 2012. - Agency for Toxic Substances and Disease Registry. Toxicological profile for lead. Atlanta, GA: US Department of Health and Human Services, CDC; 2007. Available at http://www.atsdr.cdc.gov/toxprofiles/tp.asp?id=96&tid=22. Accessed November 20, 2012.
- Kosnett MJ, Wedeen RP, Rothenberg SJ, et al. Recommendations for medical management of adult lead exposure. Environ Health Perspect 2007;115:463–71.
- Baker EL, Folland DS, Taylor TA, et al. Lead poisoning in children of lead workers: home contamination with industrial dust. N Engl J Med 1977;296:260–1.
- CDC. Childhood lead poisoning associated with lead dust contamination of family vehicles and child safety seats—Maine, 2008. MMWR 2009;58:890–3.
What is already known on this topic?
Lead exposure in children is associated with decreased intelligence, impaired neurobehavioral development, attention deficit/hyperactivity disorder, anemia, increased dental caries, decreased growth, and impaired hearing. The recycling of lead has increased during the past 20 years, with more workers and their families being potentially exposed to lead from recycling facilities.
What is added by this report?
Among employees of a lead recycling facility in Puerto Rico who agreed to be tested, the average blood lead level (BLL) was 30.7 µg/dL (range: 3.2–72.0 µg/dL), and 33 (69%) had BLLs ≥25 on their initial test. Among employees' children aged <6 years, 16% had confirmed BLLs ≥10 µg/dL, the BLL at which CDC recommends individual interventions to reduce BLL. Dust wipe and vacuum sampling indicated that employees were inadvertently contaminating their vehicles and homes with lead dust.
What are the implications for public health practice?
Employees of lead recycling facilities and their families are at risk for lead exposure. Surveillance for lead exposures, interventions that minimize the transport of lead dust out of lead processing facilities, and proper exposure controls within the occupational environment are needed.
FIGURE. Blood lead levels (BLLs) among children aged <6 years from battery recycling employee families tested for blood lead (N = 68), by age group — Puerto Rico, April and May 2011
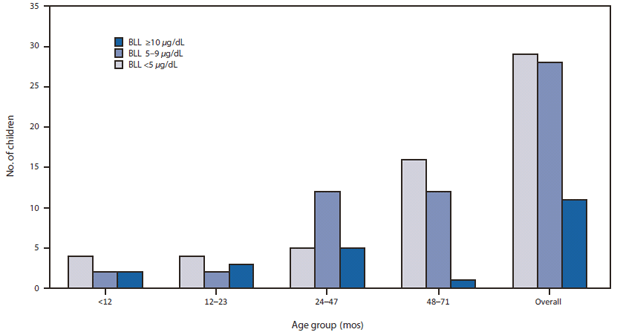
Alternate Text: The figure above shows blood lead levels (BLLs) among children aged <6 years from battery recycling employee families tested for blood lead (N = 68), by age group, in Puerto Rico, during April and May 2011. Among 68 children aged <6 years, 11 (16%) had confirmed BLLs ≥10 μg/dL, and 28 (41%) had BLLs 5-9 μg/dL.
Use of trade names and commercial sources is for identification only and does not imply endorsement by the U.S. Department of
Health and Human Services.
References to non-CDC sites on the Internet are
provided as a service to MMWR readers and do not constitute or imply
endorsement of these organizations or their programs by CDC or the U.S.
Department of Health and Human Services. CDC is not responsible for the content
of pages found at these sites. URL addresses listed in MMWR were current as of
the date of publication.
All MMWR HTML versions of articles are electronic conversions from typeset documents.
This conversion might result in character translation or format errors in the HTML version.
Users are referred to the electronic PDF version (http://www.cdc.gov/mmwr)
and/or the original MMWR paper copy for printable versions of official text, figures, and tables.
An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S.
Government Printing Office (GPO), Washington, DC 20402-9371;
telephone: (202) 512-1800. Contact GPO for current prices.
**Questions or messages regarding errors in formatting should be addressed to
mmwrq@cdc.gov.


