Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail.
Recurring Norovirus Outbreaks in a Long-Term Residential Treatment Facility --- Oregon, 2007
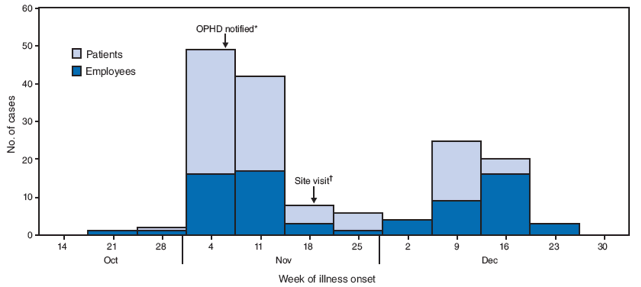
On November 9, 2007, the Oregon Public Health Division (OPHD) was notified of an outbreak of acute gastroenteritis in a long-term residential treatment facility. Two previous outbreaks caused by norovirus had occurred at the facility in March and July 2007. OPHD initiated an in-depth epidemiologic investigation, which included submitting archived and recent specimens from the three outbreaks to CDC for genotyping. This report summarizes findings of the outbreak investigation and laboratory testing. The overall attack rate for the most recent outbreak was approximately 14% among patients and 7% among employees. The outbreak was unusual in that it lasted 63 days, versus 24--27 days for the two previous outbreaks in 2007. Person-to-person transmission was suggested by a prolonged and dispersed epidemic curve and lack of illness in some wards, although all wards were served by one central kitchen. Barriers to conducting adequate hygiene (e.g., lack of handwashing stations) and multiple lapses in infection control (e.g., noncompliance with staff wellness policies) were identified. Timely and sustained implementation of comprehensive and effective infection control measures are needed to prevent and contain norovirus outbreaks in large institutional settings.
At the time of the third outbreak, the long-term treatment facility had 740 employees and approximately 690 adult patients in 22 wards in multiple buildings. Each ward houses 20--45 patients, and 1--6 patients live in each room. The median length of stay for patients is >12 months and patients' mobility outside and within the facility is restricted. Staffing in each ward often includes 4--5 physicians and social workers, 3--6 nurses, and 12--18 nursing aides. Housekeeping staff and approximately 27 nurses and nursing aides work from ward to ward as needed. A single kitchen prepares food solely for patients of the facility. Nursing aides often help serve the food to patients in each ward.
The first two norovirus outbreaks occurred in March and July of 2007, lasting 24 and 27 days, respectively (Table 1). Both outbreaks were thought to be transmitted primarily from person to person, and each affected eight wards. During the first two outbreaks, basic control measures were recommended by OPHD (1), including hand hygiene, asking ill employees to stay home until 72 hours after symptom resolution, segregating patients and employees on affected wards from unaffected wards, and using detergents registered by the U.S. Environmental Protection Agency (EPA) for thorough environmental surface disinfection.
For the third norovirus outbreak, infection control staff in the facility recorded daily information about patients and employees who had norovirus-like illnesses beginning on November 8 and retrospectively from the end of October. Demographic characteristics, onset dates and times, symptoms, and outcomes of the infection were recorded. A case was defined as acute onset of vomiting or diarrhea (three or more loose stools within any 24-hour period) in an employee or patient of the facility during October 26--December 27, 2007.
A notable increase in cases (23 patients and one employee) was observed on November 9 in three wards that had reported sporadic cases on November 6 and November 7, which prompted reporting the outbreak to OPHD (Figure). On November 9, the same basic control measures recommended during the first two outbreaks were recommended again.
Although similar foods were distributed to all wards, no kitchen staff reported norovirus-like illness and not all wards were infected, suggesting that the outbreak did not result from a common foodborne source. The outbreak lasted 63 days and affected 16 (73%) wards, 94 (14%) patients, and 51 (7%) employees. The median age among ill persons was 51 years (range: 19--85 years) for patients and 46 years (range: 21--60 years) for employees. No deaths were reported.
Infection control staff at the facility collected 25 stool specimens from 25 ill patients and employees in six wards with 10 or more reported cases for norovirus testing. OPHD investigators collected 20 environmental swab samples from surfaces of patient rooms, door knobs, bathrooms, dining tables, and work stations in these six wards on November 20, 2007. Stool and environmental specimens were tested at the Oregon State Public Health Laboratory for norovirus by real-time reverse transcription--polymerase chain reaction. To determine whether all three outbreaks were caused by the same norovirus strain, positive stool specimens from all three 2007 outbreaks were genotyped at CDC.
Of the 25 stool specimens collected during the third outbreak, 15 (60%) from five of the six wards were positive for a norovirus GII.4 variant that was different from all previously named GII.4 variants. Stool specimens from the previous two norovirus outbreaks were positive for GII.6 and GII.4 Minerva, respectively. One of the 20 environmental specimens collected from one ill patient's room was positive for norovirus GII; no sequencing was done for this specimen. Results for other environmental specimens were negative.
Because most patients in the facility were unable to give reliable information regarding potential risk factors, risk factor assessment was limited to employees. All employees in the six wards with 10 or more cases were asked to complete a printed questionnaire anonymously. The questionnaire included information on illness status, onset dates and times, duration and outcomes of illness, and potential risk factors (e.g., length of employment at the facility, previous infection in the 2007 norovirus outbreaks, cleaning vomitus, use of gloves and masks when cleaning vomitus, and hand hygiene behaviors). Questionnaires were distributed from the nursing station of each ward, beginning November 20, 2007. Completed questionnaires were collected at the nursing stations. On January 3, 2008, 1 week after the illness onset of the last case, all completed questionnaires were sent to OPHD for data entry and analysis. Pearson chi-square testing was used to compare attack rates between different exposure groups. Variables associated with illness with p<0.2 in bivariate analyses were included in a multivariate binomial regression model to assess independent associations with illness.
From among 242 employees on surveyed wards, 146 (60%) completed surveys were returned, and 51 (35%) respondents reported illnesses meeting the case definition. The symptom profile included diarrhea (100%), nausea (82%), cramps (76%), fatigue (65%), vomiting (61%), and headache (61%). The median duration of vomiting or diarrhea was 3 days (range: 1--12). Two (4%) of the ill employees reported seeing a physician. Among surveyed ill employees, 94% went to work while ill, and 8% vomited at work.
A total of 29 employees reported cleaning up vomitus at work, including in patient rooms (55%), hallways (45%), and bathrooms (48%). Of the 29 employees, 97% reported wearing gloves, 17% reported wearing masks, and none reported wearing gowns when cleaning up vomitus. Employees who reported having cleaned up vomitus were more likely to contract illness than those who did not (adjusted risk ratio [aRR] = 1.6) (Table 2). Shorter length of employment in the facility was also associated with an increased risk of illness (aRR = 1.6).
During a site visit on November 20, 2007, OPHD interviewed the infection control staff and identified major barriers or lapses in infection control. First, staff shortages and restrictions on sick-leave days made it difficult to ask ill employees to stay at home for the period recommended by OPHD guidelines and to restrict employees from working across wards (1). Second, most patients cleaned their own rooms (without EPA-registered disinfectants) because of a lack of housekeeping staff. Third, the number of handwashing stations was insufficient in most wards, and no handwashing sinks were available in dining areas or patient rooms.
Reported by: PR Cieslak, MD, LE Lee, MPH, Oregon Public Health Div, Portland. E Papafragkou, PhD, Div of Viral Diseases, National Center for Immunization and Respiratory Diseases; N An, MD, PhD, EIS Officer, CDC.
Editorial Note:
Although norovirus outbreaks are common in health-care settings (2), recurrences within a short period in a single facility are rare. This facility experienced a substantial increase in norovirus activities in 2007 compared with previous years, with three norovirus outbreaks reported in 2007, one reported in 2006, and none reported during 2003--2005. Statewide in Oregon, no increase in norovirus outbreaks in similar settings was observed during 2006--2007. Each of the three outbreaks at the facility in 2007 was caused by different norovirus variants, indicating that the recurrences of outbreaks likely resulted from repeated introduction of different norovirus variants.
Although all wards were served by a common food supply, prolonged transmission occurred only within certain wards, suggesting that this third outbreak, similar to the two previous outbreaks, likely resulted from to person-to-person transmission rather than a foodborne source. Because of the patients' long-term residency and lack of mobility outside and within the facility, employees or visitors were more likely to have contributed to the introduction of new infection and dissemination across wards. In fact, the six unaffected wards were administratively separate from the other 16 wards; neither patients nor employees transferred from the 16 affected wards to the six unaffected wards. In this facility, employees are required to use their limited sick leave days (approximately 12 days/year) when furloughed. This administrative policy and the concurrent shortage of staff might account for the number of infected employees reporting to work while sick. Barriers to conducting adequate hygiene (e.g., lack of handwashing stations), multiple lapses in infection control (e.g., noncompliance with staff wellness policies), and permitting employee mobility between affected and unaffected wards likely contributed to the recurrent and sustained outbreaks.
Facility employees who cleaned up vomitus were at higher risk for illness. This is consistent with previous reports of norovirus transmission through aerosolized vomitus (3). Gloves were worn by 97% of surveyed employees who cleaned vomitus, but they rarely wore gowns or aprons and masks while cleaning vomitus. Masks have been shown to reduce the risk for norovirus infection among nursing home employees (4). To reduce the risk for norovirus transmission through aerosolized vomitus, OPHD recommends the following steps: 1) remove vomitus and fecal material carefully to limit aerosolization (e.g., soaking up vomitus or diarrhea with paper towels or other disposable cloths with minimal agitation and removing those in impervious bags), 2) thoroughly clean surfaces and disinfect with freshly made 5,000 ppm hypochlorite solution or other EPA-registered norovirus disinfectants, and 3) wear appropriate personal protective equipment (PPE) (e.g., gloves, masks, and gowns) when cleaning vomitus or feces (1,5).
The findings in this report are subject to at least four limitations. First, illness among patients and employees might have been underreported. Second, the employee survey was anonymous; an employee could have submitted multiple questionnaires containing differing responses to health status or other questions. Third, only limited information regarding employee characteristics was collected. The difference in attack rate between short-term and long-term employees cannot be fully explained by hand hygiene or practices of cleaning vomitus. Finally, because only six wards were surveyed and the response rate was relatively low, the findings might not be generalizable to all employees of the facility.
Norovirus is infectious at low doses (as few as 10 viral particles), and long-term or cross-strain immunity is limited. Norovirus is transmitted readily in health-care settings with close contacts between ill and well persons, which makes rapid implementation of effective control measures important (6,7). The findings of this report highlight the importance of timely implementation of standard infection control practices (8) and targeted norovirus control measures as recommended by CDC for the use of masks (9), and by OPHD to prevent and control norovirus outbreaks in large residential treatment facilities (1,5). In addition, when inconsistent use of PPE is identified, CDC recommends thorough evaluation of workplace programs, such as a review of workplace policies and practices, training, selection of PPE, and disposal of used PPE. In response to this outbreak, OPHD officials worked with facility administrators to increase staff capacity and emphasize the importance of employees staying home while ill. In addition, patient rooms are now cleaned by housekeeping staff using EPA-registered products.
Acknowledgments
The findings in this report are based, in part, on contributions by K Hedberg, MD, WE Keene, PhD, M Schmidt, PhD, E Debess, DVM, H Purcell, MPH, J Terry, PhD, Oregon Public Health Div, Portland; R Obrien, W Lockett, A Melendy, Oregon Dept of Human Services, Portland; and S Lyss, MD, and E Weiss, MD, Office of Workforce and Career Development, CDC.
References
- Oregon Public Health Division. Guidelines for controlling person-to-person transmission of norovirus in nursing homes and similar settings. Available at http://www.oregon.gov/DHS/ph/acd/outbreak/control.pdf.
- van Duynhoven YT, de Jager CM, Kortbeek LM, et al. A one-year intensified study of outbreaks of gastroenteritis in The Netherlands. Epidemiol Infect 2005;133:9--21.
- Chadwick PR, McCann R. Transmission of a small round structured virus by vomiting during a hospital outbreak of gastroenteritis. J Hosp Infect 1994;26:251--9.
- Friesema IH, Vennema H, Heijne JC, et al. Norovirus outbreaks in nursing homes: the evaluation of infection control measures. Epidemiol Infect 2009;May 11:1--12 [Epub ahead of print].
- Chadwick PR, Beards G, Brown D, et al. Management of hospital outbreaks of gastro-enteritis due to small roundstructured viruses. J Hosp Infect 2000;45:1--10.
- Wu HM, Fornek M, Schwab KJ, et al. A norovirus outbreak at a long-term-care facility: the role of environmental surface contamination. Infect Control Hosp Epidemiol 2005;26:802--10.
- Cheng FW, Leung TF, Lai RW, Chan PK, Hon EK, Ng PC. Rapid control of norovirus gastroenteritis outbreak in an acute paediatric ward. Acta Paediatr 2006;95:581--6.
- CDC. 2007 Guideline for isolation precautions: preventing transmission of infectious agents in healthcare settings. Atlanta, GA: US Department of Health and Human Services, CDC; 2007. Available at http://www.cdc.gov/ncidod/dhqp/pdf/guidelines/Isolation2007.pdf.
- CDC. "Norwalk-like viruses." Public health consequences and outbreak management. MMWR 2001;50(No. RR-9).