 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Social Support and Health-Related Quality of Life Among Older Adults --- Missouri, 2000Overall health can be influenced by multiple factors, including a person's psychological, behavioral, and social well-being. Studies have demonstrated an association between increased levels of social support and reduced risk for physical disease, mental illness, and mortality (1,2). Social support includes real or perceived resources provided by others that enable a person to feel cared for, valued, and part of a network of communication and mutual obligation (2). Social support can be critical for those older adults who rely on family, friends, or organizations to assist them with daily activities, provide companionship, and care for their well-being. The 1965 Older Americans Act recognized the need for social support by requiring that agencies on aging provide in-home services and group meals to foster social interactions (3). To examine how social support is related to health-related quality of life (HRQOL), CDC analyzed data from the 2000 Missouri Older Adults Needs Assessment Survey (MOANAS) of adults aged >60 years. This report describes the results of that analysis, which indicated that visits with friends or relatives, having close friends for emotional support, and the perception of help being available if sick or disabled were associated with better HRQOL and particularly with better mental health among older adults. Implementing effective prevention programs for older adults and encouraging interventions by agencies on aging can help improve HRQOL among older adults who have little social support. In 2000, the Missouri Department of Health and Senior Services conducted MOANAS, a statewide, stratified, random-digit--dialed telephone survey designed to collect health, social service, and needs assessment data on Missouri adults aged >60 years; blacks were oversampled. The CASRO response rate was 64%. MOANAS was approved by the Institutional Review Board at the state health department. Perceived levels of social support for respondents were determined by answers to questions regarding 1) the number of persons sharing their household, 2) how often they visited or were visited by friends or relatives during the preceding month, 3) the number of close friends who might provide emotional support, and 4) the availability of help if they became sick or disabled. HRQOL was assessed by answers to questions validated for such surveillance (4), beginning with, "How many days in the preceding 30 days," and ending with 1) "was your physical health, which includes physical illness or injury, not good?" 2) "was your mental health, which includes stress, depression, and problems with emotions, not good?" 3) "did you feel sad, blue, or depressed?" 4) "did you feel worried, tense, or anxious?" and 5) "did you feel very healthy and full of energy?" Activity limitation was assessed by asking, "Are you limited in any way in any activities because of any impairment or health problem?" To examine how different levels of social support were associated with differences in HRQOL, unadjusted and multivariable-adjusted mean days (i.e., adjusted for sex, age, race/ethnicity, marital status, annual household income, and activity limitation) were calculated. Unadjusted and adjusted mean days and their 95% confidence intervals (CIs) were calculated by using statistical software cross-tabulation and multivariate linear regression analyses to account for the complex survey design. Calculations were weighted to reflect age, sex, and race/ethnicity characteristics of the Missouri population. The final sample included 3,112 respondents. HRQOL varied significantly (p<0.05) by sex, age, marital status, education, annual household income, self-rated health, and activity limitation (Table 1). On average, when compared with men, women reported more mentally unhealthy days during the preceding 30 days (2.6 days versus 1.6 days); sad, blue, or depressed days (3.1 versus 1.9); and worried, tense, or anxious days (3.9 versus 2.0). When compared with those with college degrees, participants with less than a high school education reported more physically unhealthy days (9.5 days versus 2.7 days); sad, blue, or depressed days (4.3 versus 1.2); and worried, tense, or anxious days (4.6 versus 1.9). Persons with annual household income of <$15,000, when compared with those with annual household income of >$50,000, reported more physically unhealthy days (9.8 versus 2.7); sad, blue, or depressed days (4.3 versus 1.1); and fewer days with vitality (15.2 versus 24.3). Persons with activity limitations, when compared with those without activity limitations, reported more physically unhealthy days (12.3 versus 2.8); sad, blue, or depressed days (4.3 versus 1.8); worried, tense, or anxious days (5.3 versus 2.1); and fewer days with vitality (11.5 versus 23.1). Persons who lived alone reported similar HRQOL as those who lived with one or more persons (e.g., 2.5 mentally unhealthy days versus 2.1 days for those living with one person and 3.5 for those living with two or more persons) (Table 2). However, HRQOL varied significantly (p<0.05) by other social support characteristics. Older adults who almost never visited friends or relatives during the preceding 30 days reported more mentally unhealthy days (5.1 versus 1.9); sad, blue, or depressed days (5.7 versus 2.1); worried, tense, or anxious days (5.7 versus 2.6); and fewer vitality days (15.8 versus 20.2) than those who visited friends or relatives at least several times a week. Persons who reported having no close friends for emotional support reported more physically unhealthy days (8.1 versus 5.5 for those with three or more friends), mentally unhealthy days (4.8 versus 1.9), days with depressive symptoms (5.3 versus 2.0), days with symptoms of anxiety (6.6 versus 2.7), and significantly fewer days with vitality (16.2 versus 20.1) than those with three or more friends (Table 2). In addition, those who perceived that help was available, although only for a short time, had fewer physically unhealthy days (5.3 versus 8.3); sad, blue, or depressed days (2.2 versus 6.2); or worried, tense, or anxious days (3.4 versus 6.9) than those who perceived no help available. Reported by: CL Keyes, PhD, Rollins School of Public Health; B Michalec, MA, Dept of Sociology, Emory Univ, Atlanta, Georgia. R Kobau, MPH, H Zahran, MD, MM Zack, MD, EJ Simoes, MD, Div of Adult and Community Health, National Center for Chronic Disease Prevention and Health Promotion, CDC. Editorial Note:The findings in this report suggest an association between perceived social support and HRQOL among older, community-dwelling, adults. Increased levels of perceived social support generally corresponded to fewer reported mentally unhealthy days and more vitality days. Differences by demographic subgroups were consistent with findings from previous studies and indicated that older adults with less education or lower annual household income are particularly vulnerable to impaired HRQOL (4,5). The existence and amount of social support are different from its quality and type. Social support can include perceived emotional support, instrumental support (e.g., direct assistance such as transportation), and informational support (e.g., sharing knowledge about resources). The measures of social support used in this study included emotional and instrumental support. However, additional study is needed to further examine how perceptions of support and different types of support affect HRQOL. Living alone was not associated with worse HRQOL, suggesting that household size might not be an adequate measure of social isolation. These findings extend research demonstrating that living alone is not necessarily detrimental to mental health (6). Having three or more close friends was associated with better HRQOL, compared with having one or two friends. A greater number of friends might offer a broader range of support and balance in terms of benefits and costs of social exchange (7). The findings in this report are subject to at least six limitations. First, MOANAS excluded persons without telephones or with mobile phones only and those in institutions (e.g., hospitals or nursing homes). Second, MOANAS might have excluded the severely impaired because time and functional capacity are required to participate. Third, the cross-sectional design of the survey precludes determining whether perceived social support affects HRQOL or vice versa; no causation can be inferred from the data in this report. Fourth, the study did not assess the quality of social support; more social support might not lead to better HRQOL if negative interactions (e.g., arguing) occur (1,2). Fifth, these findings are based on participants' self-assessments of physical, mental, and emotional health and perceptions of social support and might be subject to bias. Finally, social support variables are related to both health status and activity limitation; controlling for activity limitation alone might not adequately control for health status. Social support can promote health by providing persons with positive experiences, socially rewarding roles, or improved ability to cope with stressful events (1,2). Social support is critical for older adults who are at increased risk for disability associated with chronic disease or social isolation after the loss of a partner. Certain programs might help older adults who have little social support and who report worse HRQOL. For example, the Program to Encourage Active, Rewarding Lives for Seniors (operated by the University of Washington Health Promotion Research Center) was determined to reduce depressive symptoms and improve health status among community-dwelling older adults with minor depression (8). The Senior Wellness Project, a health promotion and disease management program, uses peer mentors to provide participants with social interaction, encouragement, and support in attaining their health goals (9). Finally, state and area agencies on aging have programs designed to reduce social isolation and improve HRQOL (3). Acknowledgments This report is based, in part, on data contributed by the Div of Chronic Disease Prevention and Health Promotion, Missouri Dept of Health and Senior Svcs. This study was supported under a cooperative agreement from CDC through the Association of Teachers of Preventive Medicine, Atlanta, Georgia. References
Table 1 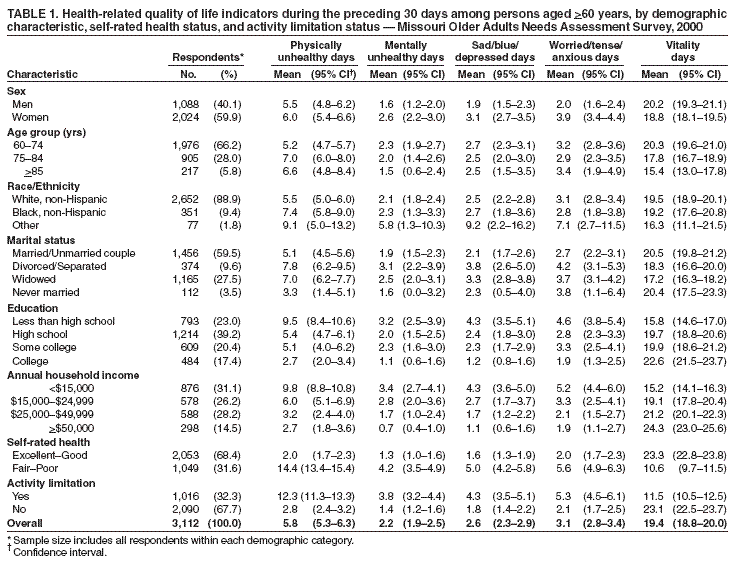 Return to top. Table 2 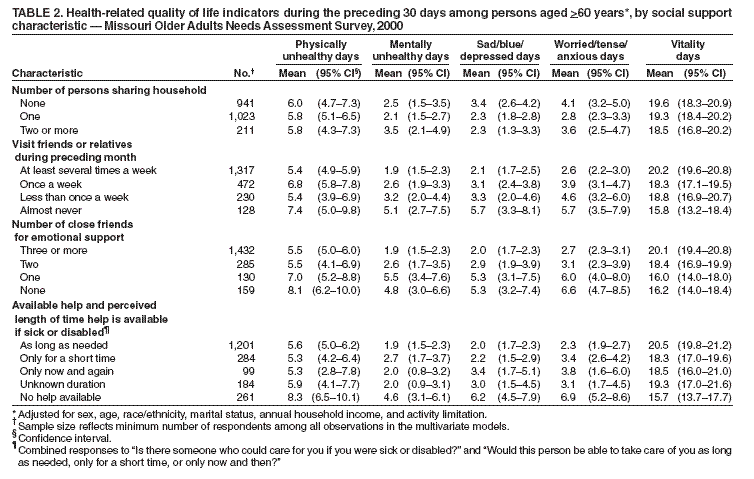 Return to top.
Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Date last reviewed: 5/5/2005 |
|||||||||
|