 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Reducing Childhood Asthma Through Community-Based Service Delivery --- New York City, 2001--2004Since 1980, asthma prevalence, hospitalization, and mortality have been increasing in the United States (1). Because of concern about asthma-related morbidity among children in Central Harlem, New York City (NYC), the Harlem Children's Zone Asthma Initiative (HCZAI) was established in 2001 to reduce asthma-related morbidity through improved surveillance, health-care use, and health-care service delivery for children aged <12 years living in a 60-block radius of Central Harlem known as the Harlem Children's Zone Project*. Families of children with asthma or asthma-like signs† or physical findings consistent with asthma are invited to participate in the program. This report summarizes preliminary data collected during 2001--2004 on the effectiveness of the program in reducing asthma-related morbidity; data indicate decreased parental/guardian reports of school absences among children enrolled in the program, both for any reason and because of asthma. In addition, emergency department and unscheduled physician office visits for treatment of asthma decreased from 35% to 8% after 18 months of the program, indicating improved asthma management and appropriate use of health-care services by program enrollees. The effectiveness of HCZAI underscores the utility of community-based public health programs in reducing asthma morbidity. Potential participants in HCZAI are identified through screening of all children aged <12 years who live or attend school in the Harlem Children's Zone Project or participate in any Harlem Children's Zone, Inc., program (2). Screening consists of a written survey completed by a parent/guardian and a physical examination of the child conducted by a physician or nurse (6). Participation rates for the various sites ranged from 66% to 100%, with 88% of parents/guardians consenting to physical examination of their children. Because of the large number of children identified with asthma or asthma-like signs, participation is prioritized for children with recent symptoms. Over time, all eligible children may enroll and participate in the program. As part of HCZAI, a pediatric asthma team (including four community workers, a social worker, a nurse, and three physicians) offers medical, educational, environmental, social, and legal services to families of enrolled children. Among participants, monitoring of 13 selected indicators (Table 1) of asthma symptoms and management strategies is conducted via home visits by community workers who interview the parents/guardians of enrolled children at 3-month follow-up intervals (7,8). Prevalence estimates for item responses were calculated by using statistical software. To assess changes in the prevalence of asthma symptoms and management strategies over time, chi-squared tests on five degrees of freedom were calculated; significance levels were replicated by using repeated measures models in statistical software. As of September 2004, a total of 3,132 children had been screened; of these, 982 (31.4%) had asthma or asthma-like signs, and 314 (10.0%) were enrolled in HCZAI (Table 2). Program enrollees were more likely than nonenrollees to have health insurance (87.0% versus 67.8%). Approximately 32.3% of children enrolled in the program had a household member who smoked at the time of screening, compared with 20.8% of children not enrolled and 16.4% of children without asthma or asthma-like signs. Preliminary data are available on the effectiveness of HCZAI in reducing asthma morbidity, as measured for all 13 selected asthma symptoms and management strategies at six 3-month follow-up time points (18 months) (Table 1). Because children were enrolled sequentially, data are not yet available for 18 months of follow-up for all 314 enrolled children. School absences reported by the parents/guardians of enrollees declined during the preceding 14 days, both for any reason (from 34.4% to 16.0% in 18 months) and because of asthma (from 23.3% to 8.0% in 18 months). In addition, emergency department and unscheduled physician office visits for treatment of asthma decreased from 35.0% to 8.0% in 18 months, indicating improved asthma management and appropriate use of health-care services by program enrollees. Reported use of asthma management strategies (e.g., using a spacer device§ and having an asthma action plan) by parents/guardians of enrolled children increased substantially over time (Table 1). Reported by: SW Nicholas, MD, VE Hutchinson, MD, B Ortiz, MD, S Klihr-Beall, MA, Dept of Pediatrics, Harlem Hospital Center; B Jean-Louis, PhD, K Shoemaker, MPP, C Singleton, MSW, J Credell, R Swaner, MPA, Harlem Children's Zone, Inc.; RD Vaughan, DrPH, ME Northridge, PhD, LF Cushman, PhD, E Polley, C Golembeski, Harlem Health Promotion Center, Columbia Univ, New York. Editorial Note:Since 2001, HCZAI has documented both a high prevalence (>30%) of childhood asthma or asthma-like signs among children in the Harlem Children's Zone Project and has substantially decreased asthma symptoms and increased asthma management strategies for enrolled children during the first 18 months of follow-up. Nonetheless, 668 children with asthma or asthma-like signs identified through screening have yet to be enrolled in HCZAI, and children aged <12 years in other Harlem Children's Zone Project schools remain to be screened for asthma and potentially enrolled. An expanded program model is planned for ensuing years. Based on findings from a qualitative evaluation involving parents/guardians of children enrolled in HCZAI and the pediatric asthma team, at least three limitations were documented. First, some families did not believe their child's diagnosis of asthma was correct, or they believed that it was outdated. Thus, they were unwilling to enroll their children in HCZAI. Second, other nonparticipants cited problems with scheduling of home visits or reported that socioeconomic needs and lack of housing precluded enrollment in HCZAI. Third, monitoring effectiveness proved burdensome for some staff and clients and failed to capture the full extent of client needs and service provision. To be more effective in reducing asthma morbidity among children in Central Harlem, additional activities will be implemented in HCZAI. These include 1) building closer working alliances with other community organizations and agencies, particularly the NYC Department of Education and the NYC Department of Health and Mental Hygiene; 2) developing protocols for situations in which family and mental health problems preclude participation in HCZAI; and 3) expanding community education regarding asthma to enhance health literacy through existing Harlem Children's Zone, Inc., programs (2). Previous research has indicated that an individualized, home-based, comprehensive environmental intervention decreased exposure to indoor allergens, resulting in reduced asthma-related morbidity (9). By incorporating HCZAI into an ongoing, community-building initiative and linking it to programs targeted to meet children's medical, educational, environmental, social, and legal needs, positive outcomes will be sustained throughout their lifetimes. Additional information about HCZAI is available at http://www.hcz.org. References
* Partners of this ongoing health intervention are Harlem Children's Zone, Inc. (2) and the Department of Pediatrics at Harlem Hospital Center (3,4). The Harlem Health Promotion Center, one of 33 Prevention Research Centers funded by CDC (5), provides translational research support to better document, monitor, and inform HCZAI during its efforts to address the asthma epidemic in Central Harlem. † For children with asthma, a parent/guardian indicated that the child had ever been told by a doctor or nurse that the child had asthma. For children with asthma-like signs, a health-care provider indicated that the child's chest radiograph was not clear, or peak expiratory flow rate for children aged >6 years was correctly performed and abnormal. § A spacer device (e.g., AeroChamber®, Optichamber®, or InspirEase ®) helps deliver inhaled medications deep into the lungs for effective relief of asthma symptoms. Table 1 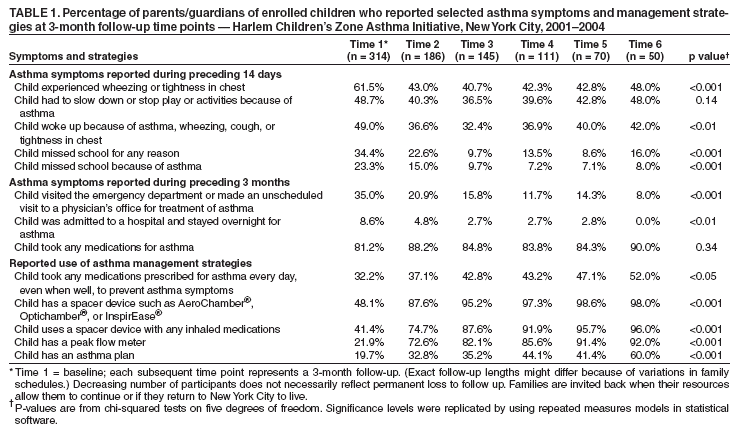 Return to top. Table 2 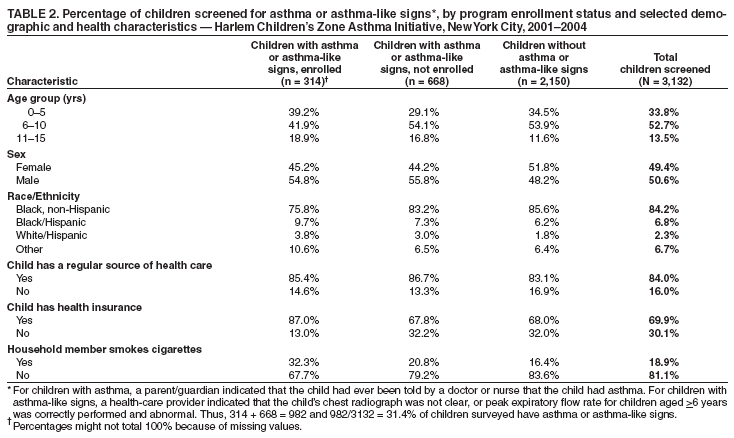 Return to top.
Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Page converted: 1/13/2005 |
|||||||||
This page last reviewed 1/13/2005
|