 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Two Cases of Visceral Leishmaniasis in U.S. Military Personnel --- Afghanistan, 2002--2004Visceral leishmaniasis (VL), a sand fly--borne parasitic disease also known as kala-azar (Hindi, for black sickness or fever), is a risk for persons who travel to or live in areas of the tropics, subtropics, and southern Europe where the disease is endemic (1). The World Health Organization estimates that approximately 500,000 new cases of this potentially fatal disease occur each year, >90% of which are acquired in parts of the Indian subcontinent, Sudan, and Brazil (1). A total of 21 cases of VL acquired in Afghanistan, all in the 1980s, have been reported previously (2--5). This report provides preliminary data about two cases of VL that have been diagnosed in U.S. military personnel deployed to Afghanistan in support of Operation Enduring Freedom, which began in 2001. U.S. health-care providers should consider VL in persons who were deployed to Southwest/Central Asia (or were in other areas where VL is endemic) who have persistent febrile illnesses, especially if associated with other clinical manifestations suggestive of VL (e.g., splenomegaly and pancytopenia) (1). Case ReportsPatients A and B were previously healthy men with febrile illnesses that began in December 2003, approximately 3 months and 14 months, respectively, after leaving Afghanistan (Table). They had been deployed during different periods (Table), in the same Special Forces unit of the U.S. Army. Both had traveled extensively in Afghanistan and had lived and worked with local Afghanis. Although they reportedly had used personal protective measures (e.g., permethrin-impregnated bed netting and insect repellent containing 30%--35% DEET), they had noted multiple insect bites. Both had used mefloquine for prophylaxis against malaria and ciprofloxacin for empiric treatment of occasional diarrheal illnesses. Neither patient had a history of blood transfusions or travel, since the mid-1990s, to other countries where VL is endemic. Both patients had classic manifestations of advanced cases of VL, including fever, cachexia, hepatosplenomegaly, pancytopenia, and hypergammaglobulinemia with hypoalbuminemia (1); both patients also had elevated aminotransferase levels. However, not all of these manifestations were present when the patients were evaluated initially; in addition, these manifestations are not specific for VL, and the results of the initial testing conducted to diagnose VL (e.g., light-microscopic examination of bone-marrow specimens) were negative. For these reasons, both patients were evaluated extensively for noninfectious diseases and for evidence of infection with nonleishmanial organisms (e.g., human immunodeficiency virus, cytomegalovirus, other viruses that cause hepatitis, and malaria parasites). In February 2004, both patients' cases of VL were diagnosed, and antileishmanial therapy was initiated (Table). Various criteria were considered when the cases of VL were diagnosed initially, including 1) clinical; 2) serologic (i.e., demonstration of antibody to rK39, a recombinant leishmanial polypeptide, by using antigen-impregnated nitrocellulose paper strips [InBios International, Inc., Seattle, Washington]) (6); and 3) parasitologic (i.e., demonstration of leishmanial parasites by light-microscopic examination of liver-biopsy specimens). Additional serologic and parasitologic evidence that the patients had VL became available later in their medical evaluations. For example, serum specimens from patients A and B showed marked reactivity to leishmanial antigens in indirect fluorescent antibody testing (titers of 1:1,024 and 1:2,048, respectively). Patient A. Fever (maximum documented temperature, 104º F [40º C]) was first noted by patient A in late December 2003 and rigors, flushing, sweats, and mild orthostasis in early January 2004. During the course of his illness, patient A experienced fluctuating temperatures and lost 13 pounds of body weight. No leishmanial parasites were noted on light-microscopic examinations or cultures of bone-marrow and liver-biopsy specimens, and no leishmanial DNA was detected by genus-specific polymerase chain reaction (PCR) analysis (7) of the bone-marrow specimen. The findings in the splenic region of a whole-body Positron Emission Tomography scan were suggestive of lymphoma, and surgical splenectomy was considered briefly. In February 2004, because of continuing concern that the patient had VL, the liver-biopsy specimen was reexamined by light microscopy; one definite and multiple probable leishmanial parasites were noted. The patient became afebrile after 1 week of antileishmanial therapy with a lipid formulation of amphotericin B (Table). Patient B. Abrupt onset of fever (maximum documented temperature, 104º F [40º C]), myalgia, and abdominal pain were noted by patient B in mid-December 2003 (Table). These and other symptoms (e.g., anorexia, with an unintentional loss of 25 pounds of body weight) worsened during the next 6 weeks. Leishmanial parasites were not found on light-microscopic examinations of bone-marrow and buffy-coat specimens but were prevalent in a liver-biopsy specimen. During February 3--17, 2004, the patient was administered 6 doses of a lipid formulation of amphotericin B (Table). Although his symptoms improved during and after the course of therapy, they worsened in late February. He was rehospitalized on March 5, with a temperature of 102º F (39º C). Leishmanial parasites and DNA were detected by light-microscopic examination and genus-specific PCR of a liver-biopsy specimen; the test results were negative for a bone-marrow specimen. In addition, for the liver specimen, the results of PCR analysis specific for the Leishmania donovani-L. infantum species complex were positive, whereas the PCR results for L. major were negative. On March 19, a 28-day course of antileishmanial therapy was begun with the pentavalent antimonial compound sodium stibogluconate (Pentostam®; GlaxoSmithKline, United Kingdom) (dose: 20 mg/kg/d, intravenously) (1). Reported by: O Myles, MD, G Wortmann, MD, Walter Reed Army Medical Center, District of Columbia. R Barthel, National Naval Medical Center, Bethesda; C Ockenhouse, MD, R Gasser, MD, P Weina, MD, Walter Reed Army Institute of Research, Silver Spring, Maryland. S Patel, MD, N Crum, MD, H Groff, MD, Naval Medical Center San Diego, California. BL Herwaldt, MD, Div of Parasitic Diseases, National Center for Infectious Diseases, CDC. Editorial Note:The term "leishmaniasis" includes three primary clinical syndromes: VL, cutaneous leishmaniasis (CL), and mucosal leishmaniasis (1). In visceral infections, leishmanial parasites replicate in the reticuloendothelial system (e.g., spleen, liver, and bone marrow). The infection can remain asymptomatic or subclinical or can become clinically manifest, with an acute, subacute, or chronic course. In the classic kala-azar syndrome of VL, patients have potentially life-threatening disease, typically after an incubation period of weeks to months, with fever, marked cachexia, hepatosplenomegaly, pancytopenia, and hypergammaglobulinemia with hypoalbuminemia (1). The two patients whose cases are described in this report had classic manifestations of advanced VL; however, their cases are unusual in certain respects. For example, for patient B, a long period (i.e., 14 months) elapsed between the end of his deployment in Afghanistan and the self-reported onset of his illness, and his symptoms recurred after treatment with a lipid formulation of amphotericin B. The possibility that he has underlying or concurrent illnesses is being considered. Although CL is common in Afghanistan, including an ongoing epidemic in Kabul with an estimated 200,000 cases (1,8,9), only 21 cases of VL attributed to exposures in Afghanistan have been reported previously (2--4). Additional cases might have occurred that were not diagnosed or reported (10). The possibility cannot be excluded that foci of VL previously considered limited to border regions of neighboring countries might have expanded into Afghanistan. The first three reported VL cases in Afghanistan, described in 1982 (2), occurred in children aged 4--5 years who lived in Kabul or Badghis Province. The cases were confirmed by demonstration of leishmanial parasites in bone-marrow specimens (2). Although the etiologic agent of these cases of what commonly is called "infantile VL" was not determined, L. infantum is considered the probable etiologic agent of VL in Afghanistan (4). PCR data obtained for patient B suggest that the U.S. soldiers were infected with organisms in the L. donovani-L. infantum species complex; the PCR method used cannot distinguish L. infantum from L. donovani. U.S. health-care providers should consider the possibility of VL in persons who have been in areas where VL is endemic and have persistent, febrile illnesses, especially if associated with other clinical signs suggestive of VL (1). Persons deployed previously to Southwest/Central Asia who have questions about their general health or leishmaniasis can contact the Deployment Health Clinical Center of the Department of Defense, telephone 866-559-1627 or at http://www.pdhealth.mil. For evaluation, treatment, and referral of military health-care beneficiaries with suspected or confirmed cases of leishmaniasis, clinicians should contact the Infectious Disease Service of either Walter Reed Army Medical Center (District of Columbia), telephone 202-782-1663/6740, or Brooke Army Medical Center (San Antonio, Texas), telephone 210-916-5554/1286. Diagnostic support can be obtained by contacting the director of the leishmaniasis diagnostic laboratory at Walter Reed Army Institute of Research (Silver Spring, Maryland), telephone 301-319-9956. Acknowledgments This report is based in part on contributions from D Hack, MD, Walter Reed Army Medical Center; P McEvoy, MD, R Neafie, MS, Armed Forces Institute of Pathology, District of Columbia. M Lim, MD, Naval Medical Center San Diego, California. References
Table 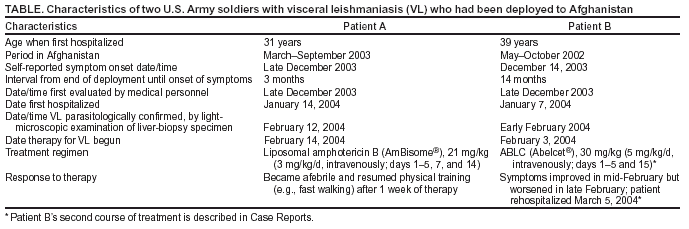 Return to top.
Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Page converted: 4/1/2004 |
|||||||||
This page last reviewed 4/1/2004
|