 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Foodborne Outbreak of Group A Rotavirus Gastroenteritis Among College Students --- District of Columbia, March--April 2000On March 31, student health services at a university in the District of Columbia (DC) notified the DC health department that an increased number of students had become ill with acute gastroenteritis beginning March 29. Some ill students reported eating tuna or chicken salad sandwiches from dining hall A on campus. On March 31, the DC health department initiated an outbreak investigation. This report summarizes results of the investigation, which indicated that group A rotavirus transmitted by food was the cause of the outbreak. Telephone interviews were conducted with students who reported illness to student health services, with additional ill students who were identified during interviews, and with healthy controls selected randomly from the university registry of students residing on campus. A case of gastroenteritis was defined as three or more episodes of diarrhea and/or two or more episodes of vomiting within a 24-hour period in a student with onset on or after March 20. Controls and case-patients whose illness onset occurred during March 27--31 were questioned about food history, residence and dining hall, source of water, use of a public access computer or sports equipment at the university gym, and attendance at social or athletic events. Electronic records of student meal attendance were available for 49 case-patients with illness onset during March 27--31 and for 55 control subjects. Twenty-three (79%) of 29 employees of dining hall A were interviewed to identify their work duties and determine whether they were ill. Stool specimens were collected during March 29--April 10 from six ill students and 21 dining hall A employees. Samples were screened for bacterial and parasitic pathogens at a commercial laboratory and for viral pathogens at CDC. The outbreak among students began March 27 and peaked at 19 cases on March 31 (Figure 1). A total of 108 students (55 were identified by telephone interviews and 53 were self-reported) had gastrointestinal symptoms during March 26--April 11; 85 (79%) had illness that met the case definition. The attack rate among students residing on campus was 5% (77 of 1641), with no significant differences in attack rates by sex, occupancy of residence hall, or grade level. Eight case-patients resided off campus (attack rate: 0.02%). Among the 83 case-patients for whom a complete list of symptoms was reported, 77 (93%) had diarrhea, 75 (90%) abdominal pain or discomfort, 69 (83%) loss of appetite, 67 (81%) nausea, 64 (77%) fatigue, 56 (67%) vomiting, 49 (59%) headache, 48 (58%) chills, 48 (58%) subjective or low-grade fever, and 42 (51%) myalgia. Sore throat, cough, and/or congestion were reported by six case-patients with onsets on or after April 2. The median duration of illness was 4 days (range: 1--8 days). Nine (11%) case-patients received intravenous fluids to treat dehydration. Of those who completed the telephone interview, 40 (91%) of 44 case-patients and 27 (68%) of 40 controls ate at least one deli sandwich from campus dining hall A during March 27--30 (p=0.017; odds ratio [OR]=4.8; 95% confidence interval [CI]=1.3--22.1). During March 27--30, four (8%) of 49 case-patients ate four or more meals at dining hall B compared with 18 (33%) of 55 controls (p=0.005; OR=0.2; 95% CI=0.04--0.6). Food histories of employees were not recorded; however, six employees reported illness. Stool specimens of students and employees were negative for bacterial and parasitic pathogens and for Norwalk-like viruses. Using electron microscopy, enzyme immunoassay, and reverse transcriptase-polymerase chain reaction (RT-PCR), nine (33%) of 27 specimens were positive for group A rotavirus. Rotavirus positive stool specimens from four students and three employees were identified as genotype combination P[4],G2 by RT-PCR. Two of the three P[4],G2-positive employees were line cooks who reported having symptoms of gastroenteritis on March 27 and April 2, respectively, while the third positive employee, a deli server, reported no illness. Reported by: M Fletcher, PhD, ME Levy, MD, Bur of Epidemiology and Disease Control, District of Columbia Dept of Health. DD Griffin, Oak Ridge Institute for Science and Education, Oak Ridge Associate Univs, US Dept of Energy. Viral Gastroenteritis Section, Respiratory and Enterovirus Br, Div of Viral and Rickettsial Diseases, National Center for Infectious Diseases, CDC. Editorial Note:Group A rotavirus is the most common cause of childhood diarrhea worldwide, infecting >90% of children by age 3 years (1). Because rotavirus immunity develops early in life, disease among older children and adults is uncommon (1). Although the role of rotavirus in diarrhea outbreaks in adults has not been well studied, it has been documented as the cause of adult diarrheal outbreaks in hospitals (2), nursing homes (3), isolated communities (4), and in travelers (5). Also, parents of children infected with rotavirus have been reported to experience acute gastroenteritis (6). However, the rotavirus G and P protein-type combinations, the proteins that elicit an immune response in humans, were not characterized in most of these reports. The rapid increase and gradual decline of the campus outbreak suggest that the infection was foodborne during the first week and was spread person-to-person during the following week. During the first week, illness was associated with eating sandwiches at dining hall A and was associated inversely with eating frequently at dining hall B. The employee who prepared sandwich fillings did not report illness and tested negative for rotavirus. None of the three deli servers who assembled and served sandwiches reported illness; however, one was rotavirus P[4],G2 positive. It is unknown whether the deli server who tested positive was infected before the outbreak among students. This rotavirus serotype G2 outbreak was unusual for two reasons; food was implicated as the source of infection and the adults affected should have been immune. During April 2000, a gastroenteritis outbreak among adults in Japan also was caused by foodborne transmission of group A rotavirus serotype G2 (7). These adults should not have been susceptible to severe rotavirus illness. G2 strains often are found combined with serotype P[4]1B (8). The G and P neutralization antigens of serotype G2 strains may allow G2 strains to escape immunity induced by the more common G1, G3, and G4 strains. In addition, G2 has been associated with more severe dehydration during diarrheal episodes in children than other common strains (9). These outbreaks of rotavirus gastroenteritis in adults in the United States and Japan raise questions about the persistence of immunity to rotavirus and the virulence of G2 strains. Investigators and clinicians should consider rotavirus as a possible cause of acute gastroenteritis in adults. References
Figure 1 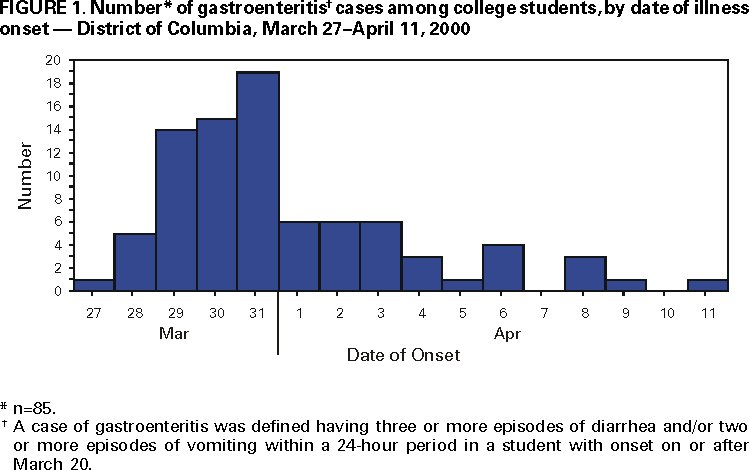 Return to top. Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Page converted: 12/21/2000 |
|||||||||
This page last reviewed 5/2/01
|