 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Epidemic Malaria Transmission -- Armenia, 1997The dissolution of the Former Soviet Union (FSU) has resulted in the disruption of the health infrastructure in many of the republics, as indicated in part by increases in infectious diseases that were previously controlled (e.g., diphtheria, typhoid, and hepatitis A). In 1994, the Ministry of Health (MOH) of Armenia (1995 population: 3.5 million) detected the first locally acquired case of malaria since the 1940s; the number of imported cases (15) was approximately twice the annual average during 1986-1989 (seven). In 1995, although no locally acquired cases were reported, the number of imported cases increased to 502. In 1996 and 1997, the total (locally acquired and imported) number of reported cases of malaria was 347 and 841, respectively. This report summarizes surveillance for malaria in Armenia during 1996-1997. Cases were initially identified based on clinical suspicion; confirmation was based on microscopic examination of blood smears by the national laboratory. All cases were caused by Plasmodium vivax. Local clinics and hospitals gathered data and reported this information to the regional public health offices, which in turn reported to the national level. From 1996 to 1997, the incidence rate (IR) for all reported cases of malaria increased from nine to 22 per 100,000 population (Table_1). Locally acquired cases accounted for 567 (67%) of the 841 cases reported in 1997. Although 30 (37%) of 81 districts recorded malaria cases, seven (9%) reported locally acquired infections. In 1997, the Masis district registered 527 (63%) of the total and 505 (89%) of the locally acquired cases (IR=592 and 567 cases per 100,000 population, respectively) (Figure_1). The seasonal peak for locally acquired cases occurred in September (132 {23%}); 416 (73%) cases were reported during July-October (Figure_2). To identify possible vectors, the MOH took a convenience sample of mosquitos using standard trapping techniques. Anopheles maculipennis was identified as the most common vector species captured (98%). Reported by: V Davidiants, MD, National Information and Analytic Center; M Mannrikian, MD, Sanitary Epidemiologic Svcs; G Sayadian, MD, Health Care System; A Parunakian, MD, Republican Sanitary and Epidemiologic Svc; B Davtian, MD, Ararat Regional Health Dept, Ministry of Health, Armenia. World Health Organization, European Region, Copenhagen. Capacity Development Br, Div of International Health, Epidemiology Program Office; Malaria Section, Epidemiology Br, Div of Parasitic Diseases, National Center for Infectious Diseases; and an EIS Officer, CDC. Editorial NoteEditorial Note: The World Health Organization (WHO) estimates that malaria causes 300 to 500 million illness episodes and 1.5 to 2.7 million deaths worldwide each year (1). From 1945 to 1986, FSU-wide malaria eradication efforts (including mosquito vector control, case detection and treatment, and chemoprophylaxis) curtailed transmission in Armenia, one of the 15 Newly Independent States of the FSU. During 1988-1995, severe financial constraints and the war with Azerbaijan contributed to cessation of vector-control activities in Armenia (which had included the use of mosquito-larvivorous fish {Gambusia affinis}, insecticide spraying, and the reduction of mosquito breeding sites). These circumstances, combined with an eroding health infrastructure, may have hindered new malaria cases from being diagnosed, treated, and reported properly during this period. Displaced persons returning from the war with Azerbaijan during the cease-fire accounted for many of the imported cases in 1995; the resurgence of locally transmitted malaria probably resulted from persons with imported cases transmitting infection to the increased density of vectors. In December 1992, the MOH and CDC, with the support of the U.S. Agency for International Development, began restructuring the health information systems (HIS) in Armenia. The reform began with the development of an emergency surveillance system designed to detect acute health risks (2,3). By 1996, through additional training and technical support, the MOH adopted a countrywide, comprehensive, and sustainable HIS reform program *. The prompt detection of this malaria epidemic highlights the success of this Armenian HIS reform. The magnitude of the increase in malaria may be underestimated because surveillance relied on clinical suspicion. Because few cases were seen until recently, physicians may not have suspected malaria and submitted blood smears for laboratory confirmation. The next steps for malaria control and prevention in Armenia should focus on surveillance, clinical practice, public education, and environmental control. Enhanced surveillance will include 1) initiating active, case-based surveillance; 2) establishing a regional surveillance network because malaria is endemic in neighboring countries; and 3) conducting epidemiologic and entomologic studies to characterize the affected population, determine risk factors for acquisition and transmission, and target interventions. Improving clinical practice will require continuing medical education for physicians in the early diagnosis and treatment of malaria and improved microscopic diagnostic capabilities for rapid and accurate diagnosis. Such capabilities will be essential if P. falciparum malaria emerges, because treatment recommendations depend on the species detected. Community health education about recognizing malaria symptoms should be provided. Vector control should be conducted in the Masis district, especially during the peak transmission season (July to October). Efforts led by WHO are under way to institute some of these control measures during the next malaria season; additional control measures may be taken if resources become available. References
* Armenian Prikaz (administrative directive) no. 550, July 30, 1996. Table_1 Note: To print large tables and graphs users may have to change their printer settings to landscape and use a small font size.
TABLE 1. Number of locally acquired and imported cases of malaria and incidence rates
(IR)*, by year -- Armenia, 1986-1997+
======================================================================================
Locally acquired Total
--------------- ------------
Year No. (IR) Imported No. (IR)
---------------------------------------------------------
1986 0 9 9
1987 0 7 7
1988 0 8 8
1989 0 3 3
1994 1 (<0.1) 15 16 ( 0.4)
1995 0 502 502 (13.3)
1996 149 ( 3.9) 198 347 ( 9.2)
1997 567 (15.0) 274 841 (22.2)
---------------------------------------------------------
* Per 100,000 population.
+ Surveillance data were not available for 1990-1993.
======================================================================================
Return to top. Figure_1 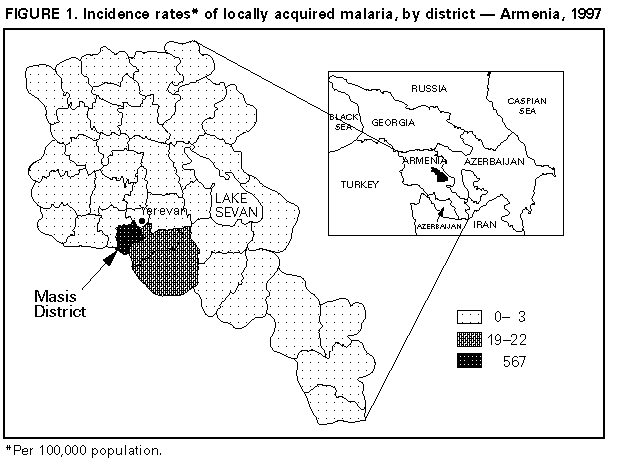 Return to top. Figure_2 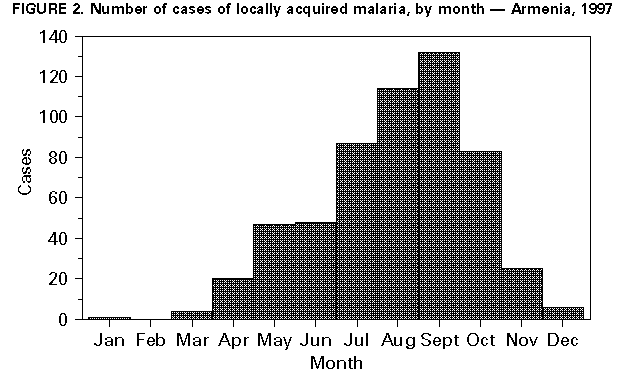 Return to top. Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Page converted: 10/05/98 |
|||||||||
This page last reviewed 5/2/01
|