Key points
- The CDC Injury Center funds states, tribes, territories, non-governmental organizations, and university research programs to prevent suicide.
- These programs track and monitor suicide related outcomes, build implementation capacity, and implement and evaluate suicide prevention strategies with the best available evidence.

Background
Preventing suicide and self-harm is a priority across the United States. Prevention efforts in states and communities are built on seven key strategies from CDC's Suicide Prevention Resource for Action and informed by use of more near real-time data through syndromic surveillance in additional jurisdictions.
State snapshots
Select a funded state from the map or data table below to view a snapshot of the suicide prevention activities supported by the Injury Center. Each snapshot contains:
- Overall suicide prevention fiscal year (FY) 2023 funding, including program categories and recipient information
- Key suicide-related statistics
- Examples of how states are working to prevent suicide
Hover over the map to quickly view information about the funding and burden for each state. Use the filter to see which states are funded by each program.
Tribal suicide prevention
In FY20, the Injury Center began funding tribal organizations through CDC's umbrella cooperative agreement, Tribal Public Health Capacity Building and Quality Improvement Cooperative Agreement. This agreement allows tribal recipients to tailor, implement, and evaluate suicide prevention programs with the best available evidence to reduce suicide-related death and injury among American Indian and Alaska Native (AI/AN) populations.
The tribal recipients and their associated annual funding amounts are below:
- Southern Plains Tribal Health Board: $265,000
- Wabanaki Health and Wellness: $265,000
Examples of tribal suicide prevention efforts are described below.
Activities and progress
With CDC funding, states, tribes, territories, and other organizations are initiating and expanding suicide prevention activities. Examples of progress are highlighted below. These samples of activities are intended to illustrate the work and are not inclusive of all efforts.
Comprehensive Suicide Prevention (CSP)
The CSP program is funded through a cooperative agreement awarded to 17 recipients to implement and evaluate a comprehensive public health approach to suicide prevention, with attention to people who are at increased/higher risk of suicide. Each recipient uses data to identify populations with increased risk of suicide and assesses current programs addressing these populations in their jurisdictions to determine gaps in prevention. Some examples of these populations include youth, rural residents, Hispanic/Latino men, the LGBTQIA+ population, persons with disabilities, and veterans.
Based on this information and working with multi-sectoral partners, recipients select a combination of strategies and approaches with the best available evidence from CDC's Suicide Prevention Resource for Action to implement and evaluate. These selections address the multiple contributors to suicide at the individual, relationship, community, and societal levels.
All 17 recipients have chosen to implement strategies and approaches to create protective environments (e.g., reducing access to lethal means among people at risk of suicide), identify and support people at risk, and promote connectedness. All recipients are implementing at least three strategies, with some recipients implementing up to seven.
Fourteen CSP programs also use funds to support emergency department syndromic surveillance of nonfatal suicide-related outcomes (e.g., suicide attempts and suicidal ideation). Collecting these near real-time data can help states rapidly track and respond to changing patterns in suicidal behavior. This surveillance work builds upon CDC's previously funded Emergency Department Surveillance of Nonfatal Suicide-Related Outcomes program.
To learn more about each CSP recipient, open the state snapshot by clicking on the map or table above.
Veteran Suicide Prevention
CDC collaborates with the CDC Foundation to build the capacity of veteran serving organizations (VSOs) to evaluate their upstream suicide prevention activities. VSO recipients use CDC's Evaluation Framework, resources, and technical assistance to develop and implement evaluation plans and build their capacity for ongoing program evaluation.
Most VSOs follow either a community integration model, linking veterans with community services to address issues like housing or transportation, or a connectedness model, which focuses on helping veterans engage with like-minded communities to avoid feelings of isolation. In both approaches, the goal is to address small, day-to-day issues before they become significant problems.
Organizations take a holistic approach to veteran suicide prevention, working with community organizations to address the challenges veterans face before they turn into deeper problems. Because circumstances surrounding veteran suicide are complex, this organization develops and maintains relationships with veterans to help them balance their lives collectively, from education and employment to housing and transportation, among others.
The CDC Foundation understands that effective plans should include collaboration across sectors as part of an upstream public health approach to ending veteran suicide. For this purpose, a virtual meeting among VSOs, CDC, and CDC Foundation staff was held in June 2022 to increase understanding of the work and experiences of the VSO recipients and the integration of evaluation into suicide prevention efforts.
To learn more about each VSO recipient, open state snapshots by clicking on the map or table above.
Continuing the Work to Prevent Veteran Suicide | CDC Foundation
CDC Foundation Grants Help Combat Veteran Suicide | CDC Foundation
Project Helping to Reduce Veteran Suicide Provides Evaluation Findings
Tribal Suicide Prevention
Through the Tribal Public Health Capacity Building and Quality Improvement cooperative agreement, CDC funds the Southern Plains Tribal Health Board and Wabanaki Health and Wellness tribal organizations to increase their capacity for comprehensive suicide prevention. In cooperation with partners and through a series of listening sessions, recipients use data to identify groups at increased risk of suicide in their communities. They assess gaps in prevention and choose at least one strategy/approach with the best available evidence from the CDC's Suicide Prevention Resource for Action (or from another resource, such as the Substance Abuse and Mental Health Services Administration's To Live To See The Great Day That Dawns to tailor based on the cultural context of their communities, for implementation and evaluation.
See below for some current examples of how these tribal organizations are working to prevent suicide.
- Southern Plains Tribal Health Board: With CDC funding, Southern Plains Tribal Health Board (SPTHB) supports suicide prevention among high school students from the United Keetoowah Band of Cherokee Indians in Oklahoma and Cherokee Nation. SPTHB developed partnerships with 16 external organizations and individuals. This includes a partnership with Northeastern State University's Center for Tribal Studies program that assessed the needs of students and helped the university get approval for funding two additional mental health counselors, doubling their staff size to four counselors. SPTHB also implemented a culturally specific program called American Indian Life Skills training at two high schools. The program focused on helping students recognize risk factors for suicide, identify suicide prevention resources, improve problem-solving and coping skills, and seek help when needed. Evaluation results indicated students' knowledge of suicide prevention and protective factors increased 35% compared to baseline. In addition, SPTHB has trained over 1,000 individuals across 39 suicide prevention trainings, including Question, Persuade, and Refer, Talk Saves Lives, and Suicide Prevention for Youth, over the course of this cooperative agreement.
- Wabanaki Public Health and Wellness: Wabanaki Public Health and Wellness (WPHW) used CDC funding to develop a culture-based, holistic approach to wellness for the Wabanaki Tribes of Maine (Passamaquoddy, Penobscot, Maliseet, and Mi'kmaq Tribes). The Tribal Public Health Capacity Building and Quality Improvement cooperative agreement funded interventions designed to strengthen cultural identity and community connectedness, which can protect against poor mental health, suicidal thoughts and behavior, substance use, and injuries. Some of the cultural activities, including making traditional regalia and participating in drum making in a group setting, helped to foster connectedness among elders and veterans. Through the Color Paper Project, which provides food and other essentials to elders in Passamaquoddy territories, Sipayik and Indian Township, 243 homes received daily assistance from support staff during the COVID-19 pandemic. WPHW also implemented activities to educate community members and provide access to services, including through suicide prevention gatekeeper trainings, a Veterans Affairs claims clinic, and support groups.
Other support to territories
CDC funding to US territories supported their capacity building to prevent suicide. In 2018, as a part of the hurricane response, CDC awarded Puerto Rico and the US Virgin Islands $920,000 and $230,000, respectively, to aid in their suicide prevention efforts.
CDC funded Puerto Rico and the US Virgin Islands to support gatekeeper trainings designed to help participants learn the warning signs of suicide and how to appropriately respond. This work prioritized suicide prevention training in healthcare settings; educated gatekeepers about suicidal ideation and behavior; supported suicide surveillance and partnerships; created a network of frontline professionals to be activated during natural disasters; and built capacity of these professionals to identify, manage, and refer persons with suicidal ideation and/or behavior during natural disasters.
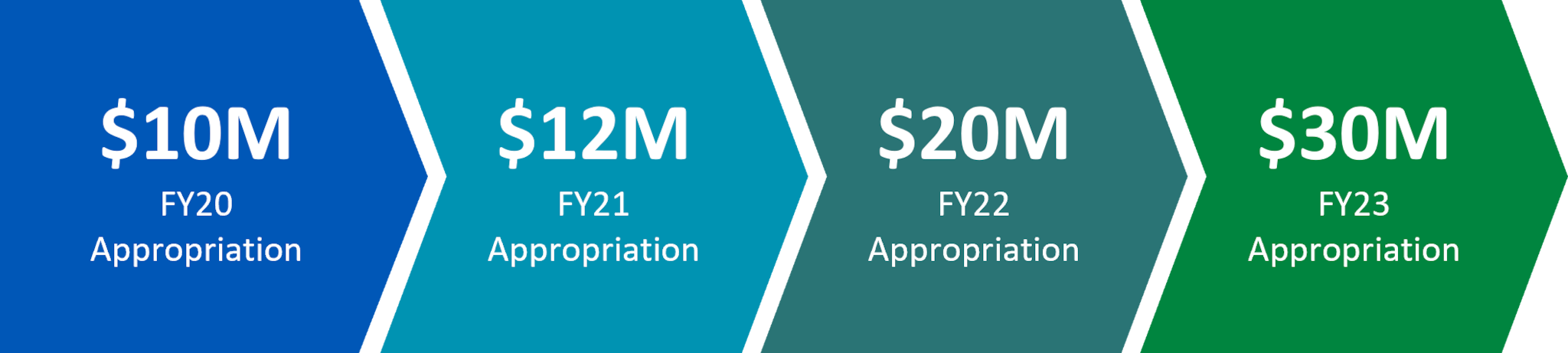
Funding over time
Congress directed an appropriation line to CDC for suicide prevention activities in 2020. The Injury Center used these appropriations to expand funding to a variety of state, territorial, tribal, and non-governmental organizations.
Other projects
In addition to funding and supporting the suicide prevention programs outlined above, the Injury Center collaborates with the following groups on suicide prevention initiatives.
- Core State Injury Prevention Program (Core SIPP)
- Approximately $4 million in COVID-19 funding was divided evenly amongst 22 of 23 Core State Violence and Injury Prevention Program (Core SVIPP) recipients to help states address suicide and ACEs prevention, including enhancing virtual implementation of prevention resources.
- Approximately $4 million in COVID-19 funding was divided evenly amongst 22 of 23 Core State Violence and Injury Prevention Program (Core SVIPP) recipients to help states address suicide and ACEs prevention, including enhancing virtual implementation of prevention resources.
- Injury Control Research Centers (ICRCs)
- The Injury Center funds Injury Control Research Centers (ICRCs) to conduct research, training, and outreach to study and implement ways to prevent injuries and violence.
- The Injury Center funds Injury Control Research Centers (ICRCs) to conduct research, training, and outreach to study and implement ways to prevent injuries and violence.
- POLARIS
- CDC has a wide variety of research, data, and information that can inform evidence-based policy. CDC developed POLARIS to centralize policy-relevant tools, training, and resources on various health topics.
- CDC has a wide variety of research, data, and information that can inform evidence-based policy. CDC developed POLARIS to centralize policy-relevant tools, training, and resources on various health topics.
- Prevention Institute
- Through a cooperative agreement with CDC, the Prevention Institute updated content in CDC's Suicide Prevention Resource for Action and developed modules that provide a foundation for activities like virtual tools during periods of infrastructure disruption.
- Through a cooperative agreement with CDC, the Prevention Institute updated content in CDC's Suicide Prevention Resource for Action and developed modules that provide a foundation for activities like virtual tools during periods of infrastructure disruption.
- Safe States Alliance
- Safe States Alliance was funded approximately $950,000 to address ACEs and suicide prevention activities during the pandemic. In collaboration with the American Foundation for Suicide Prevention (AFSP) and the National Action Alliance for Suicide Prevention (Action Alliance), they created a variety of resources, including community suicide prevention messages, workforce trainings, and web resources. Some of these resources include the National Mental Health and Suicide National Response to COVID 19, two online hubs to help injury and violence prevention practitioners adapt to the changing landscape (INsiders and COVID-19 IVP Resource Hub), and over 150 suicide prevention education programming events to a virtual format for a national audience.
- Safe States Alliance was funded approximately $950,000 to address ACEs and suicide prevention activities during the pandemic. In collaboration with the American Foundation for Suicide Prevention (AFSP) and the National Action Alliance for Suicide Prevention (Action Alliance), they created a variety of resources, including community suicide prevention messages, workforce trainings, and web resources. Some of these resources include the National Mental Health and Suicide National Response to COVID 19, two online hubs to help injury and violence prevention practitioners adapt to the changing landscape (INsiders and COVID-19 IVP Resource Hub), and over 150 suicide prevention education programming events to a virtual format for a national audience.
- Suicide, Overdose, and ACEs Prevention Capacity Assessment Tool (SPACECAT)
- SPACECAT allows agencies to consider their capacity as it relates to ACEs, overdose, and suicide, in the context of the ecological framework.
- SPACECAT allows agencies to consider their capacity as it relates to ACEs, overdose, and suicide, in the context of the ecological framework.
- Violence Prevention in Tribal Communities
- 12 Indian Health Service Regional Tribal Health Boards received $1 million in COVID-19 response funding to support improving capacity and prevention for intimate partner violence, suicide, and ACEs, including assessing behavioral health needs, creating communication toolkits, and improving data and surveillance.
- 12 Indian Health Service Regional Tribal Health Boards received $1 million in COVID-19 response funding to support improving capacity and prevention for intimate partner violence, suicide, and ACEs, including assessing behavioral health needs, creating communication toolkits, and improving data and surveillance.
Resources
Connect with a trained crisis counselor. 988 is confidential, free, and available 24/7/365.
- Call or text 988
- Chat at 988lifeline.org
Visit the 988 Suicide and Crisis Lifeline for more information at 988lifeline.org.
