Key points
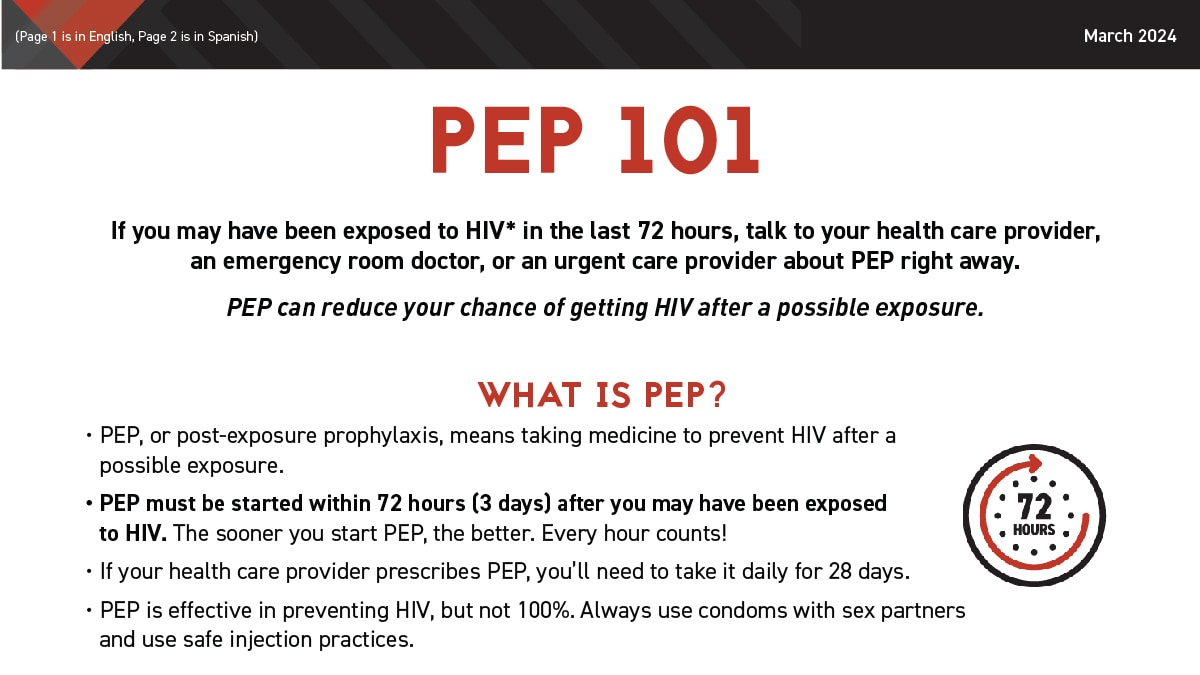
- PEP is medicine that prevents HIV after a possible exposure.
- PEP is for emergency situations only.
- PEP must be started within 72 hours (3 days) after exposure.

Overview
PEP (post-exposure prophylaxis) is medicine that prevents HIV after a possible exposure. PEP must be started within 72 hours (3 days) after a recent possible exposure to HIV.
Talk right away to your health care provider, an emergency room doctor, or an urgent care provider about PEP if you think you've recently been exposed to HIV:
- during sex (for example, if the condom broke),
- through sharing needles, syringes, or other equipment to inject drugs, or
- if you've been sexually assaulted.
PEP is safe but may cause side effects like nausea in some people. In almost all cases, these side effects can be treated and aren't life-threatening.
Use the locator below to find PEP services near you. Remember, the sooner you start PEP, the better. Every hour counts. If you're prescribed PEP, you'll need to take it daily for 28 days.
PEP is not the right choice for people who may be exposed to HIV frequently and is not a substitute for regular use of other HIV prevention methods like using condoms with sex partners and safe injection practices.
If you are a gay or bisexual man or a transgender woman with a history of at least one bacterial STI (syphilis, chlamydia, gonorrhea) in the last 12 months, talk to your health care provider about doxy PEP.
PEP and workplace exposures
If you think you've been exposed to HIV at work, see a health care provider, an emergency room doctor, or an urgent care provider right away.
- Report your exposure to the appropriate person at work and seek medical attention immediately.
- PEP must be started within 72 hours after an exposure. The sooner you start PEP, the better. Every hour counts.
- Careful practice of standard precautions can help reduce exposure while caring for patients with HIV.
Clinicians caring for workers who've had a possible exposure can call the PEPline (1-888-448-4911) for advice on managing occupational exposures to HIV. Exposed workers may also call the PEPline, but they should seek local medical attention first.
Paying for PEP
Depending on the reason you are prescribed PEP, you may qualify for free or low-cost PEP medicines.
Paying for PEP after a sexual assault
You may qualify for partial or total reimbursement for medicines and clinical care costs. Find resources available in your area.
Paying for PEP after a workplace exposure
Your workplace health insurance or workers' compensation will usually pay for PEP.
Paying for PEP for another reason
If you can't get insurance coverage, your health care provider can apply for free PEP through medication assistance programs run by manufacturers. These requests for assistance can be handled urgently in many cases to avoid a delay in getting medicine.