At a glance
Occupational HIV transmission is extremely rare. Only 58 cases of confirmed occupational HIV transmission to health care personnel have been reported in the United States. An additional 150 possible transmissions have also been reported to CDC.*

Preventing occupational HIV transmission
- Always follow Standard Precautions. Assume that all body fluids are potentially infectious.
- Use gloves, goggles, and other barriers when coming in contact with blood or body fluids.
- Wash hands and other skin surfaces immediately after contact with blood or body fluids.
- Be careful when handling and disposing of sharp instruments.
- Use safety devices to prevent needle-stick injuries.
- Dispose of used syringes or other sharp instruments in a sharps container.
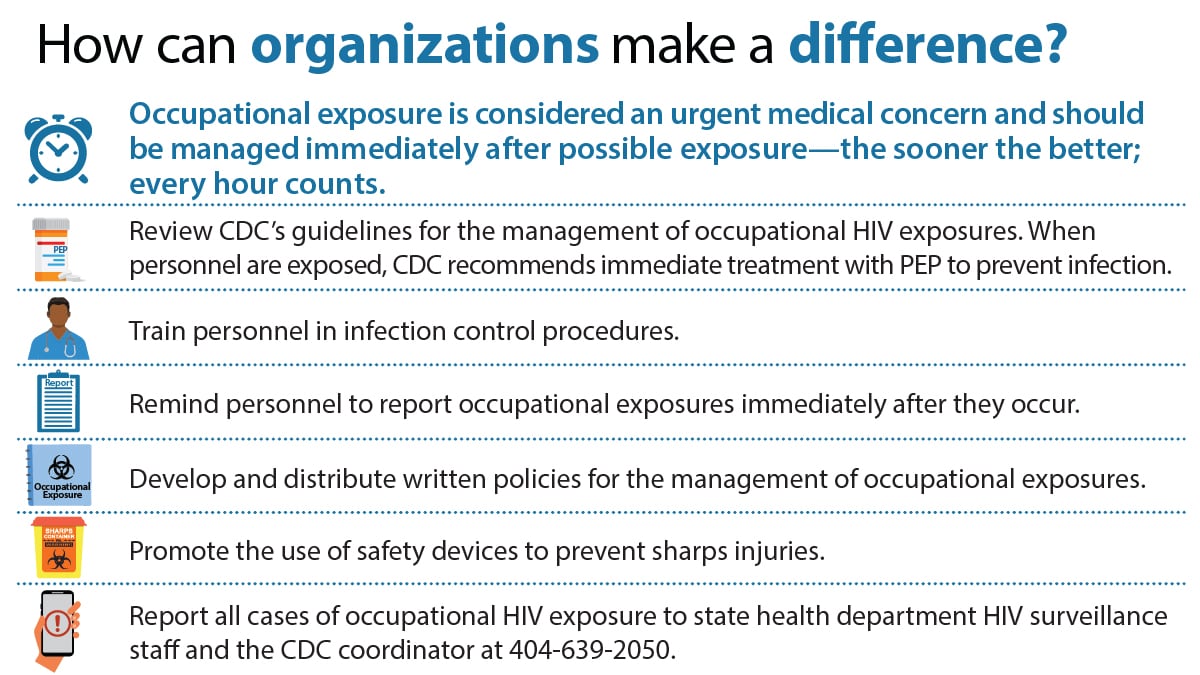
Managing occupational HIV exposures
- If you are exposed to HIV at work, report your exposure to the appropriate person. Then, see a doctor or visit an emergency room right away.
- Post-exposure prophylaxis (PEP) can reduce your chance of getting HIV infection. It must be started within 72 hours (3 days) after you may have been exposed to HIV. The sooner you start PEP, the better. Every hour counts!
- Clinicians caring for personnel who've had a possible exposure can call the PEPline 1-888-448-4911, 11 am to 8 pm EST, seven days a week, for advice on managing the exposure.
- Clinicians who administer PEP should tell patients about possible side effects and follow patients closely to make sure they take their medicine correctly.
* Based on the most recent data available in December 2013. Of these, only 1 confirmed case has been reported since 1999.