Key points
- If you have high levels of lipoprotein (a) (Lp(a)), you are more likely to have a heart attack, a stroke, or aortic stenosis, especially if you have familial hypercholesterolemia or signs of coronary heart disease.
- High Lp(a) levels run in families.
- Current treatments for high Lp(a) are limited.
What it is
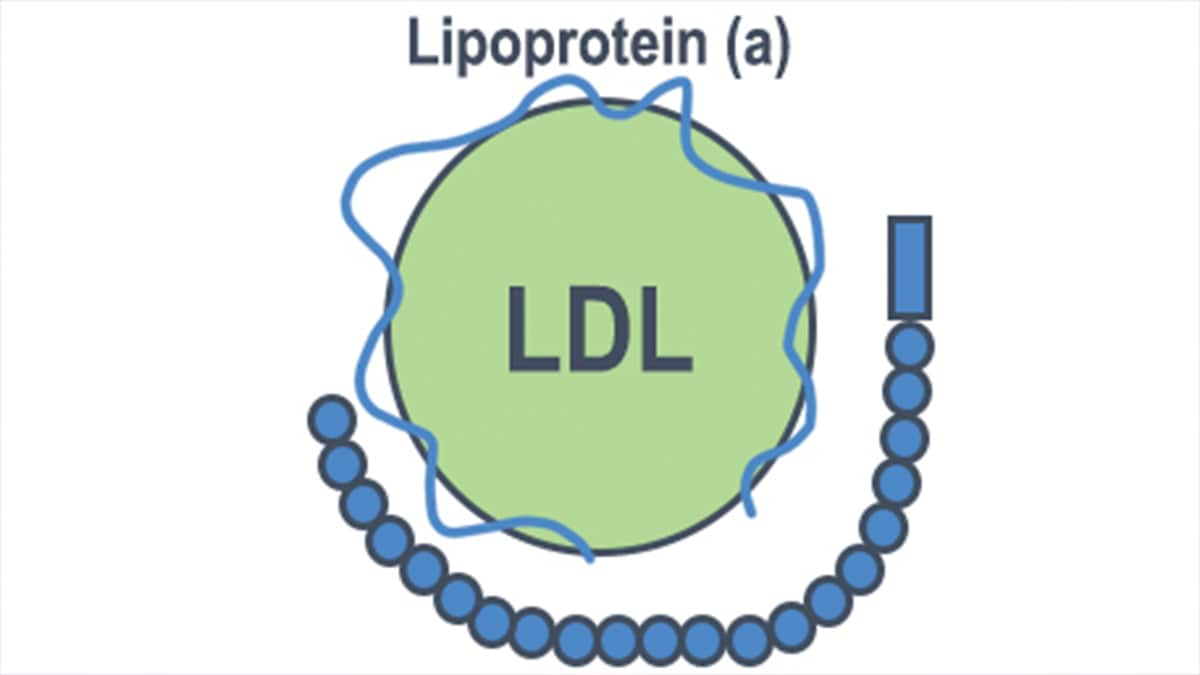
High levels of lipoprotein (a) (Lp(a), pronounced “L-P-little-A”) increase your likelihood of having a heart attack, a stroke, and aortic stenosis, especially if you have familial hypercholesterolemia (FH) or signs of coronary heart disease. Cholesterol travels through the blood on lipoproteins, which are made of protein and fat. Lipoproteins include low-density lipoprotein (LDL), high-density lipoprotein (HDL), and Lp(a).
Effects
High Lp(a) levels increase your likelihood of having a heart attack or stroke, especially if you have FH or signs of coronary heart disease. This is because:
- Like LDL-cholesterol, Lp(a)-cholesterol can build up in the walls of your blood vessels. This is more likely this is to happen if you have higher Lp(a) levels. These cholesterol deposits, called plaques, can decrease blood flow to your heart, brain, kidneys, lungs, legs, and other parts of your body. Plaques can grow over time or suddenly rupture, blocking blood vessels and leading to heart attacks or strokes.1
- Lp(a) can cause increased clotting, which can lead to rapidly formed blockages in blood vessels.1
- Lp(a) promotes inflammation which increases the likelihood that plaques will rupture.
Because of its role in inflammation, high Lp(a) can also lead to narrowing of the aortic valve, called aortic stenosis.1 Chronic inflammation leads to calcium build up on the valve, causing stiffness. This can result in reduced blood flow if the valve is unable to open completely. In some cases, people with aortic stenosis need surgery or a procedure to replace the aortic valve.
Risk factors
High Lp(a) levels run in families. If one of your family members has high Lp(a), talk to your healthcare provider about having your Lp(a) levels checked. Likewise, if you have high Lp(a), your healthcare provider may recommend that your children, siblings, or parents have their Lp(a) levels checked.
How do I know if I have high Lp(a)?
High Lp(a) levels, defined as greater than 50 mg/dL (125 nmol/L),2 are common. Median Lp(a) levels vary by race and sex.3 High Lp(a) is seen in people of all races and ethnicities but appears to be more common in Black people.3 Many people with high Lp(a) have no symptoms. However, your healthcare provider may suspect that you have high Lp(a) if you have any of the following risk factors:
- Poor circulation in your legs (called peripheral arterial disease)
- Heart attack, stroke, or coronary artery disease before age 55 (in men) or age 65 (in women) without known risk factors, such as high LDL, smoking, diabetes, or obesity
- Female family members who had a heart attack or stroke before age 65
- Male family members who had a heart attack or stroke before age 55
- Familial hypercholesterolemia
- Certain types of aortic stenosis
Your healthcare provider can diagnose high Lp(a) by measuring your blood Lp(a) level and reviewing your personal and family health history. Lp(a) is not routinely included when you get your cholesterol checked. Your healthcare provider has to order the blood test for Lp(a) separately. About a third of people with FH also have high Lp(a) levels, and current recommendations state that people with FH should have their Lp(a) level checked.
Treatment
Lp(a) levels cannot be controlled by healthy eating and exercising. Lipoprotein apheresis is the only therapy approved by the Food and Drug Administration (FDA) for treating high Lp(a) levels, and it is only approved for people with FH who have LDL≥100 mg/dL, Lp(a)≥60 mg/dL, and coronary or other artery disease. Apheresis is a treatment like dialysis in which a machine removes Lp(a) and LDL-cholesterol from the blood.
If you have high Lp(a) levels, you should take steps to lower your LDL-cholesterol if it is high. Some studies4 suggest that medications called statins might slightly raise Lp(a) levels but are still recommended due to their effects in lowering LDL-cholesterol and reducing the risk of heart attacks, strokes, and peripheral arterial disease. If you have FH, coronary artery disease, or peripheral arterial disease, your healthcare provider might recommend also taking a medication called PCSK9 inhibitors to further lower your LDL level. While a healthy lifestyle will not lower Lp(a) levels, it does impact LDL levels, so people with high Lp(a) should keep a healthy weight, not smoke, choose healthy foods and drinks, and get regular physical activity. Managing conditions such as diabetes and high blood pressure is also important for people with high Lp(a).
- Reyes-Soffer G, Ginsberg HN, Berglund L, Duell PB, Heffron SP, Kamstrup PR, et al. Lipoprotein(a): A Genetically Determined, Causal, and Prevalent Risk Factor for Atherosclerotic Cardiovascular Disease: A Scientific Statement From the American Heart Association. Arterioscler Thromb Vasc Biol 2022; 42(1):e48-e60.
- Grundy SM, Stone NJ, Bailey AL, Beam C, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/ APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;139:e1082– e1143.
- Patel AP, Wang M, Pirruccello JP, Ellinor PT, et al. Lp(a) (Lipoprotein[a]) Concentrations and Incident Atherosclerotic Cardiovascular Disease. Arteriosclerosis, Thrombosis, and Vascular Biology 2021;41:465–474.
- Tsimikas S. A Test in Context: Lipoprotein(a) Diagnosis, Prognosis, Controversies, and Emerging Therapies. Journal of the American College of Cardiology. 2016;69(6):692-711.
