Key points
- Familial hypercholesterolemia (FH) is an inherited condition that causes high blood levels of low-density lipoprotein (LDL) cholesterol.
- People with FH are more likely to have coronary artery disease or a heart attack.
- Finding and treating FH early, with medicines such as statins, is important to prevent coronary artery disease.

What it is
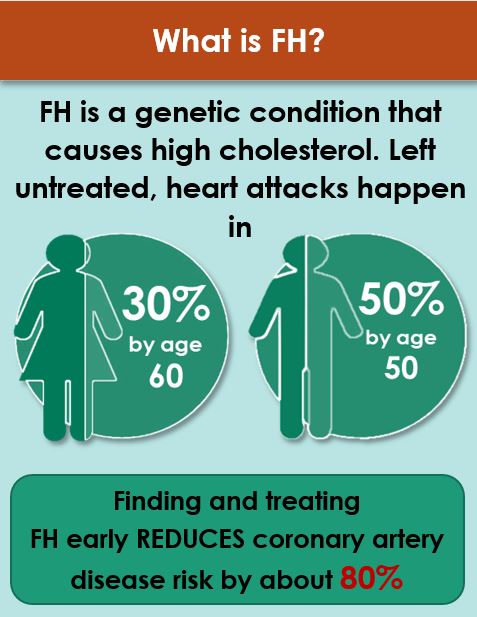
Familial hypercholesterolemia (FH) is a genetic disorder that affects about 1 in 311 people and increases the chance of having coronary artery disease at a younger age. People with FH have increased blood levels of low-density lipoprotein (LDL) cholesterol, sometimes called "bad cholesterol." Having too much LDL cholesterol in your blood increases your risk for developing coronary artery disease or having a heart attack. For people with FH, exercising and healthy eating habits are important, but often not enough to lower their cholesterol to a healthy level. Medicines, such as statins, are needed to help control cholesterol levels. If you have FH, finding and treating the disorder early can reduce your risk of coronary artery disease by about 80%. If your child is diagnosed with FH, statin therapy in childhood may be required, often starting by age 8-10.
Signs and symptoms
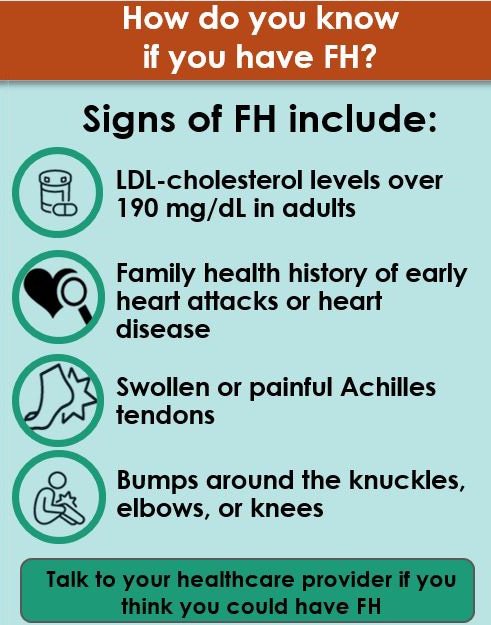
One of the main signs of FH is LDL cholesterol levels over 190 mg/dL in adults (and over 160 mg/dL in children). In addition, most people with FH have a family health history of early coronary artery disease or heart attacks. In some cases, elevated LDL levels are found through routine blood cholesterol screening. If you have a family health history of heart disease or FH and have not had your cholesterol screened, your healthcare provider may order lipid screening, which measures the amount of cholesterol and lipids (fats) in your blood.
Your healthcare provider may be able to detect physical signs of FH during a clinical exam, although not everyone with FH has these signs. These physical signs of FH occur when extra cholesterol builds up in different parts of the body:
- Bumps or lumps around your knees, knuckles, or elbows
- Swollen or painful Achilles tendon (the tendon at the back of your lower leg)
- Yellowish areas around your eyes
- A whitish gray color in the shape of a half-moon on the outside of your cornea (the clear outer layer at the front of your eye)
If your healthcare provider suspects you have FH, he or she may refer you for genetic counseling and testing for FH.
Causes
FH is mainly caused by inherited genetic changes (mutations) that affect how your body regulates and removes cholesterol from your blood. About 60-80% of people with FH have a specific genetic change. Genetic testing is available to check for these genetic changes.
Prevention
If you or a family member have FH or high LDL cholesterol, it is important to maintain a healthy lifestyle along with taking your medicine. Making healthy lifestyle changes for your family can benefit your children who may be at risk for FH and promote healthy habits that they will continue as adults. The following are steps that you can take as a family:
- Eating a healthy diet low in saturated fats, trans fats, salt (sodium), and drinks with added sugar, and high in fiber, fresh fruits, and vegetables.
- Being physically active.
- Not smoking.
- Limiting alcohol use.
- Checking and controlling your cholesterol and blood pressure.
- Managing your diabetes, if you have it.
Testing
Your healthcare provider may refer you for genetic counseling and testing for FH if they suspect that you have FH based on your blood cholesterol levels, family health history, and physical signs of FH.
Genetic testing for FH can confirm your diagnosis, help you better understand your risk for coronary artery disease and heart attacks, and inform your treatment. If genetic testing shows that you have a genetic change that causes FH, your family members can be tested for the same change to find out if they have FH.
Treatment
If you have FH, having a healthy lifestyle and being physically active are important, but often are not enough to lower your cholesterol to a healthy level. You will need to take cholesterol-lowering medicine to control your cholesterol levels. In most cases, you will need to take more than one type of cholesterol-lowering medicine to lower your LDL cholesterol to a healthy level. The most commonly prescribed medicines are statins.
Next steps
If you are concerned that you could have familial hypercholesterolemia or hereditary heart disease, collect your family health history of heart disease and talk to your healthcare provider.
Resources
- AHA: What is Familial Hypercholesterolemia?
- Family Heart Foundation: Familial Hypercholesterolemia
