Key points
- Hypoplastic (pronounced hi-puh-PLAS-tik) left heart syndrome or HLHS is one type of congenital heart defect.
- Congenital means present at birth.
- HLHS prevents normal blood flow through the heart.
- Surgical repairs for HLHS are not a cure.
- People with this condition should schedule routine checkups with a heart doctor to stay as healthy as possible.

What it is
HLHS occurs when the left side of the heart does not form correctly during pregnancy. HLHS affects normal blood flow through the heart. A baby born with HLHS will need surgery soon after birth. HLHS is considered a critical congenital heart defect (critical CHD).
What is affected
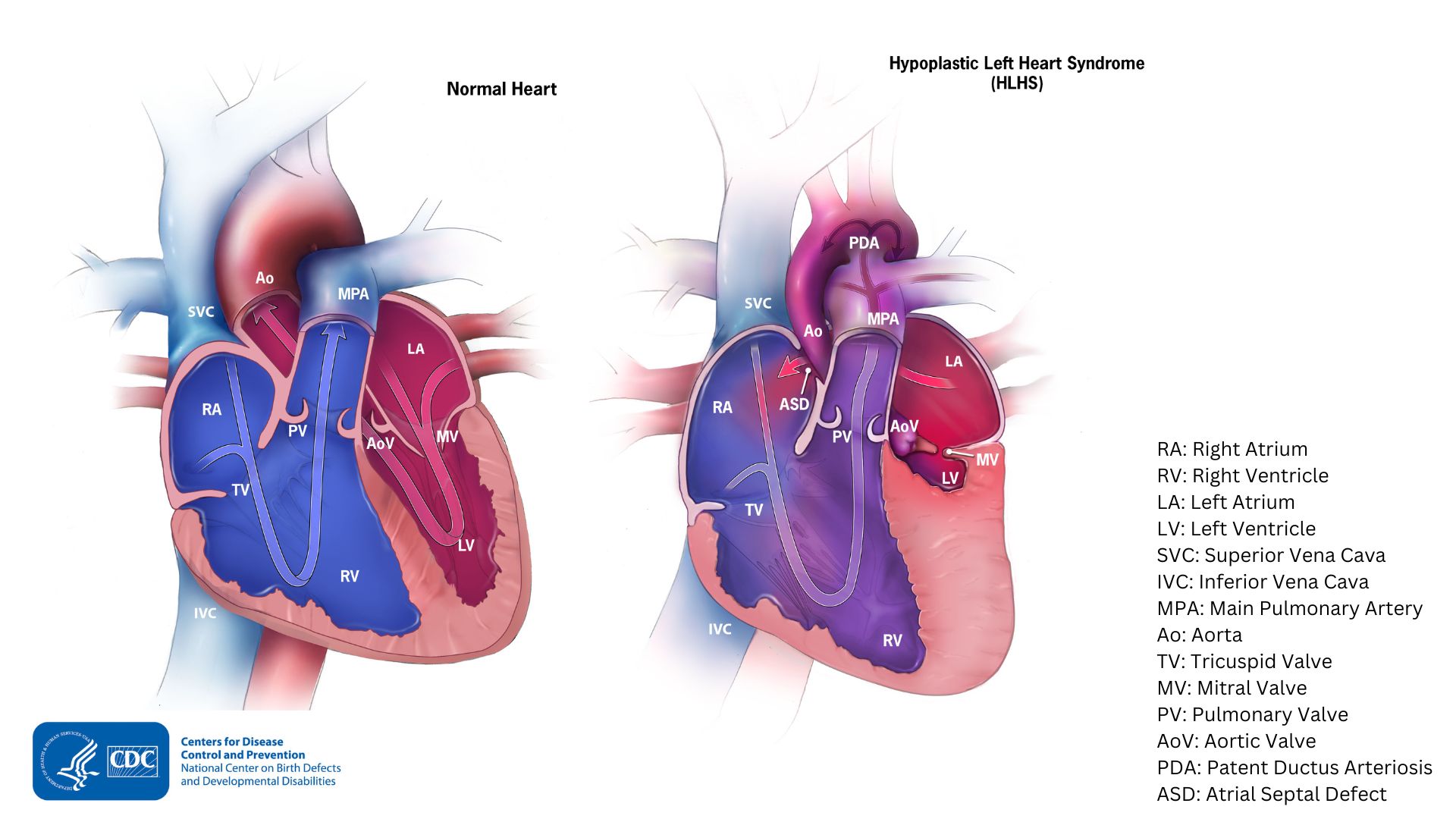
HLHS affects a number of structures on the left side of the heart that do not fully develop:
- The left ventricle is underdeveloped and too small
- The mitral valve is not formed or is very small
- The aortic valve is not formed or is very small
- The ascending portion of the aorta is underdeveloped or is too small
Often, babies with HLHS also have an atrial septal defect, a hole between the upper chambers (atria) of the heart.
How it works
During pregnancy, a fetus has two small openings between the left and right sides of the heart. These openings are called the patent ductus arteriosus (PDA in image above) and the foramen ovale. These openings in the heart usually close a few days after birth.
In babies with HLHS, the left side of the heart cannot pump oxygen-rich blood to the body properly. Oxygen-rich blood bypasses the left side of the heart through the patent ductus arteriosus and the foramen ovale. This issue occurs during the first few days of life. The right side of the heart then pumps blood to both the lungs and the rest of the body. When these openings close, it is harder for oxygen-rich blood to get to the rest of the body.
Occurrence
About 1 in 3,846 (about 925) babies in the United States are born with HLHS each year.
Signs and symptoms
HLHS might not cause trouble for the first few days of life while the PDA and the foramen ovale remain open. However, they may quickly develop signs and symptoms after these openings close, including:
- Problems breathing
- Fast heart rate
- Weak pulse
- Ashen or bluish skin color
Risk factors
The causes of HLHS among most babies are unknown. Some babies have heart defects because of changes in their genes or chromosomes. A combination of genes and other risk factors may increase the risk for HLHS. These factors can include things in a mother's environment, what she eats or drinks, or the medicines she uses.
Diagnosis
HLHS may be diagnosed during pregnancy or soon after a baby is born.
During pregnancy
During pregnancy, screening tests (prenatal tests) check for birth defects and other conditions. An ultrasound, a tool that creates pictures of the baby, may detect HLHS. If a healthcare provider suspects HLHS, they can request a fetal echocardiogram to confirm the diagnosis. A fetal echocardiogram is a more detailed ultrasound of the baby's heart. This test can show problems with the structure of the heart and how the heart is working with this defect.

After the baby is born
Doctors might notice the signs and symptoms listed above. They might also detect a heart murmur when listening to a baby's heart with a stethoscope. A murmur is an abnormal "whooshing" sound caused by blood not flowing properly. If a murmur is heard or other symptoms are present, the healthcare provider might request additional tests to confirm the diagnosis. The most common test is an echocardiogram, which is an ultrasound of the heart.
HLHS can also be detected with newborn pulse oximetry screening. Low levels of oxygen in the blood can be a sign of a critical CHD like HLHS.

Treatments
Treatments for HLHS might include the following:
Medicines
Some people with HLHS will need medicines to:
- Strengthen the heart muscle
- Lower their blood pressure
- Help the body get rid of extra fluid
Nutrition
Some babies with HLHS become tired while feeding and do not eat enough to gain weight. To make sure babies have a healthy weight gain, a special high-calorie formula might be prescribed. Some babies become extremely tired while feeding and might need to be fed through a feeding tube.
Surgery
Soon after a baby with HLHS is born, multiple surgeries done in a particular order are needed. These surgeries will help increase blood flow to the body and bypass the poorly functioning left side of the heart. The surgeries help the right ventricle become the main pumping chamber for blood to reach the body.
These surgeries do not cure HLHS but help restore heart function. Sometimes medicines are given to help treat symptoms of the defect before or after surgery. Surgery for HLHS usually is done in three separate stages:
1. Norwood procedure. This surgery usually is done within the first 2 weeks of a baby’s life. Surgeons create a “new” aorta and connect it to the right ventricle. They also place a tube from either the aorta or the right ventricle to the vessels supplying the lungs (pulmonary arteries). Thus, the right ventricle can pump blood to both the lungs and the rest of the body. This can be a very challenging surgery. After this procedure, an infant’s skin still might look bluish because oxygen-rich and oxygen-poor blood still mix in the heart.
2. Bi-directional Glenn Shunt procedure. This surgery usually is performed when an infant is 4 to 6 months of age. This procedure creates a direct connection between the pulmonary artery and the superior vena cava. The superior vena cava is a vessel that returns oxygen-poor blood from the upper part of the body to the heart. This new connection reduces the work of the right ventricle by allowing blood from the body to flow to the lungs.
3. Fontan procedure. This surgery is usually done between 18 months and 3 years of age. Doctors connect the pulmonary artery and the inferior vena cava. The inferior vena cava is the vessel that returns oxygen-poor blood from the lower part of the body to the heart. This allows the rest of the blood coming back from the body to go to the lungs. Once this procedure is complete, oxygen-rich and oxygen-poor blood no longer mix in the heart. As a result, an infant’s skin will no longer look bluish.
What to expect long-term
Surgical repairs for HLHS are not a cure. Infants with HLHS may have lifelong complications. They will need routine checkups with a heart doctor to monitor their progress.
If the HLHS defect is very complex, or the heart becomes weak after the surgeries, a heart transplant may be needed. Infants who receive a heart transplant will need to take medicines for the rest of their lives. These medications may prevent their body from rejecting the new heart.
- Stallings EB, Isenburg JL, Rutkowski RE et al; for the National Birth Defects Prevention Network. National population-based estimates for major birth defects, 2016–2020. Birth Defects Res. 2024;116(1):https://doi.org/10.1002/bdr2.2301
