Key points
- Coarctation of the aorta (pronounced koh-ark-TEY-shun) is a type of congenital heart defect. Congenital means present at birth.
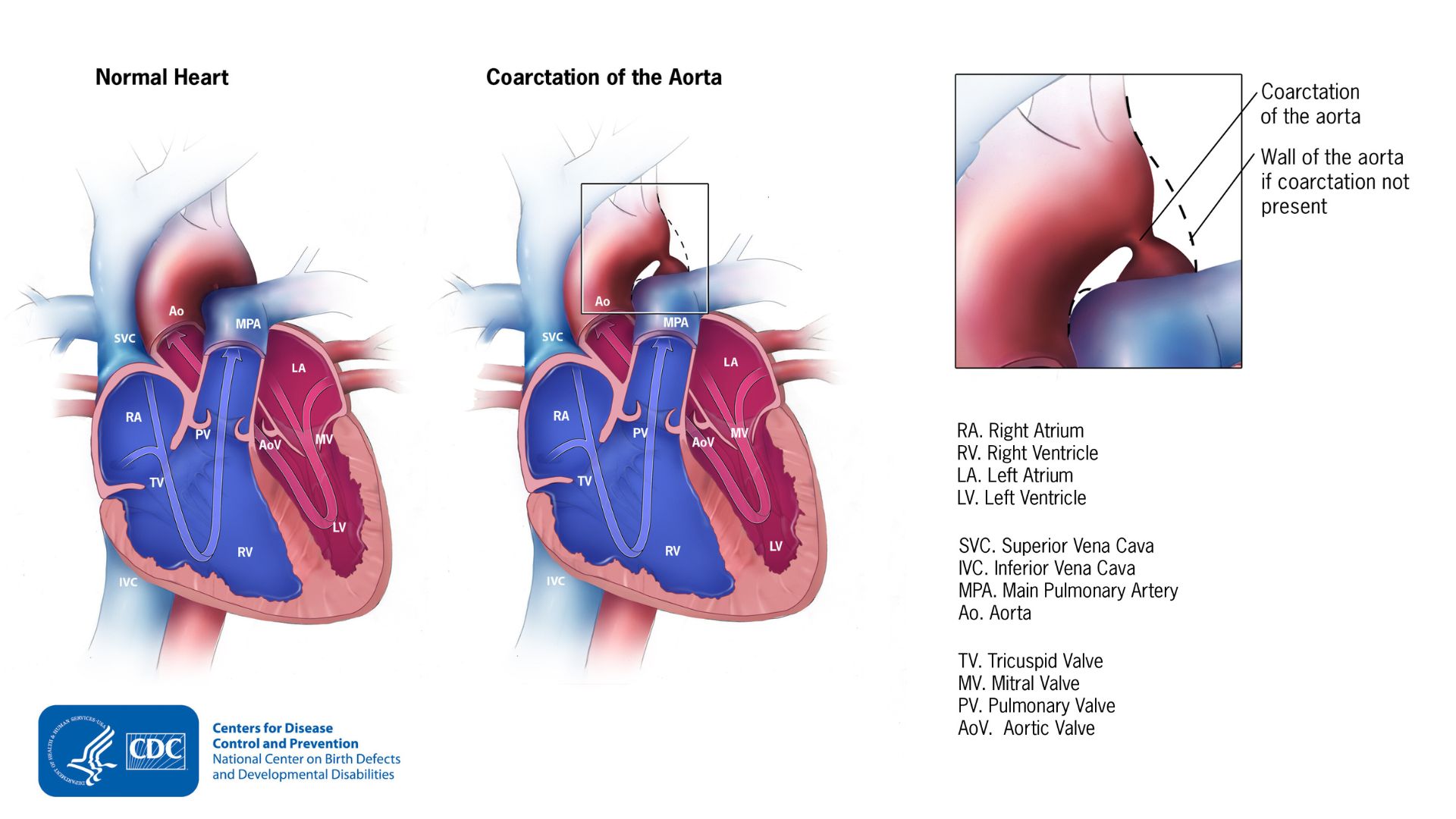
- It occurs when a part of the aorta is narrower than usual.
- People with coarctation of the aorta should follow-up regularly with a heart doctor throughout their lives.

What it is
Coarctation of the aorta occurs when a baby's aorta doesn't form correctly as the baby develops during pregnancy. The aorta is tube that carries oxygen-rich blood from the heart to the rest of the body. Babies with this condition have a part of their aorta that is narrower than usual.
The narrowing, or coarctation, blocks normal blood flow to the body. This can back up flow into the left ventricle of the heart. As a result, the muscles in this ventricle work harder to get blood out of the heart.
If the narrowing is severe enough and it is not diagnosed, the baby may have serious problems soon after birth. For this reason, coarctation of the aorta is considered a critical congenital heart defect (critical CHD).
Occurrence
About 1 in 1,724 (about 2,060) babies in the United States are born with coarctation of the aorta each year.
Coarctation of the aorta often occurs with other congenital heart defects.
Signs and symptoms
The narrowing of the aorta is usually located after arteries branch to the upper body. In infants, coarctation in this region can lead to:
- Normal or high blood pressure and pulsing of blood in the head and arms
- Low blood pressure and weak pulses in the legs and lower body
In babies with a more severe form of coarctation of the aorta, early signs may include:
- Pale skin
- Irritability
- Heavy sweating
- Difficulty breathing
Older children and adults with coarctation of the aorta often have high blood pressure in the arms.
Complications
If the coarctation is very severe, enough blood may not be able to get through to the lower body. The extra stress on the heart can cause the walls of the heart to become thicker in order to pump harder. This eventually weakens the heart muscle. If the aorta is not widened, the heart may weaken enough that it leads to heart failure.
Risk factors
The causes of coarctation of the aorta among most babies are unknown. Some babies have heart defects because of changes in their genes or chromosomes. A combination of genes and other risk factors may increase the risk for coarctation of the aorta. These factors can include things in a mother's environment, what she eats or drinks, or the medicines she uses.
In some babies with coarctation, some tissue from the wall of ductus arteriosus blends into the tissue of the aorta. The ductus arteriosus is a blood vessel that helps the blood bypass the lungs during pregnancy. The ductus arteriosus normally closes after birth. The extra tissue may tighten and narrow the aorta when the ductus arteriosus closes normally after birth.
Diagnosis
Coarctation of the aorta is usually diagnosed after the baby is born. How early in life the defect is diagnosed usually depends on how mild or severe the symptoms are.
Coarctation of the aorta is a critical CHD. However, newborn screening with pulse oximetry might be less likely to detect this condition.
Detection of the defect is often made during a physical exam. The pulse will be noticeably weaker in the legs or groin than it is in the arms or neck. A heart murmur—an abnormal whooshing sound caused by disrupted blood flow—may be heard through a doctor’s stethoscope. Older children and adults with coarctation of the aorta often have high blood pressure in the arms.

Once suspected, the healthcare provider might request one or more tests to confirm the diagnosis. The most common test is an echocardiogram, which is an ultrasound of the heart. It will show the location and severity of the coarctation and whether any other heart defects are present. Other tests to measure the function of the heart may be used including:
- Chest x-ray
- Electrocardiogram (EKG)
- Magnetic resonance imaging (MRI)
- Cardiac catheterization
Treatment and recovery
No matter what age the coarctation is diagnosed, the narrow aorta will need to be widened once symptoms are present. This can be done with a procedure called balloon angioplasty or through surgery.
A balloon angioplasty uses a thin, flexible tube, called a catheter. The catheter is inserted into a blood vessel and directed to the aorta. When the catheter reaches the narrow area of the aorta, a balloon at the tip is inflated. This helps to expand the blood vessel.
Sometimes a mesh-covered tube (stent) is inserted to keep the vessel open. The stent is often used to initially widen the aorta or re-widen it if the aorta narrows again after surgery.
During surgery to correct a coarctation, the narrow portion is removed. The aorta is reconstructed or patched to allow blood to flow normally through the aorta.
What to expect long-term
Even after surgery, children with a coarctation of the aorta often have high blood pressure that is treated with medicine. Children and adults with coarctation of the aorta should follow up regularly with a cardiologist (or heart doctor) to:
- Monitor their progress
- Check for other health conditions that might develop as they get older
