Acinetobacter in Healthcare Settings
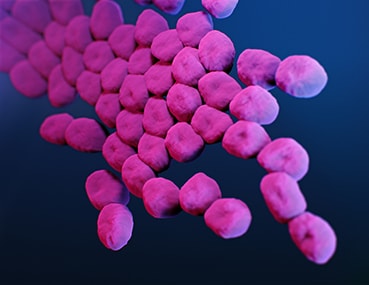
Acinetobacter is a group of bacteria (germs) commonly found in the environment, like in soil and water. While there are many types, the most common cause of infections is Acinetobacter baumannii, which accounts for most Acinetobacter infections in humans.
Acinetobacter baumannii can cause infections in the blood, urinary tract, and lungs (pneumonia), or in wounds in other parts of the body. It can also “colonize” or live in a patient without causing infections or symptoms, especially in respiratory secretions (sputum) or open wounds.
See CDC’s report
Antibiotic Resistance Threats in the United States, 2019
These bacteria are constantly finding new ways to avoid the effects of the antibiotics used to treat the infections they cause. Antibiotic resistance occurs when the germs no longer respond to the antibiotics designed to kill them. If they develop resistance to the group of antibiotics called carbapenems, they become carbapenem-resistant. When resistant to multiple antibiotics, they’re multidrug-resistant. Carbapenem-resistant Acinetobacter are usually multidrug-resistant.
How common are these infections?
In 2017, carbapenem-resistant Acinetobacter caused an estimated 8,500 infections in hospitalized patients and 700 estimated deaths in the United States [Source: 2019 AR Threats Report].
Who is at risk?
Acinetobacter infections typically occur in people in healthcare settings. People most at risk include patients in hospitals, especially those who:
- are on breathing machines (ventilators)
- have devices such as catheters
- have open wounds from surgery
- are in intensive care units
- have prolonged hospital stays
In the United States, Acinetobacter infections rarely occur outside of healthcare settings. However, people who have weakened immune systems, chronic lung disease, or diabetes may be more susceptible.
How is it spread?
Acinetobacter can live for long periods of time on environmental surfaces and shared equipment if they are not properly cleaned. The germs can spread from one person to another through contact with these contaminated surfaces or equipment or though person to person spread, often via contaminated hands.
How can you avoid getting an infection?
Patients and caregivers should:
- keep their hands clean to avoid getting sick and spreading germs that can cause infections
- wash their hands with soap and water or use alcohol-based hand sanitizer, particularly before and after caring for wounds or touching a medical device
- remind healthcare providers and caregivers to clean their hands before touching the patient or handling medical devices
- allow healthcare staff to clean their room daily when in a healthcare setting
In addition to hand hygiene, healthcare providers should pay careful attention to recommended infection control practices, including rigorous environmental cleaning (e.g., cleaning of patient rooms and shared equipment), to reduce the risk of spreading these germs to patient.
How are these infections treated?
Acinetobacter infections are generally treated with antibiotics. To identify the best antibiotic to treat a specific infection, healthcare providers will send a specimen (often called a culture) to the laboratory and test any bacteria that grow against a set of antibiotics to determine which are active against the germ. The provider will then select an antibiotic based on the activity of the antibiotic and other factors, like potential side effects or interactions with other drugs.
Unfortunately, many Acinetobacter germs are resistant to many antibiotics, including carbapenems, which makes them difficult to treat with available antibiotics.
What is CDC doing to address Acinetobacter infections?
CDC tracks the germ, and the infections it can cause, through its Emerging Infections Program. Additionally, CDC works closely with partners, including public health departments, other federal agencies, healthcare providers, and patients, to prevent healthcare infections and to slow the spread of resistant germs.