Key points
U.S. CDC in South Sudan and partners helped increase South Sudan's ability to provide quality healthcare services to communities. The initiatives expanded access to HIV treatment, trained healthcare workers on clinical best practices, and improved oversight of local HIV programs.
Background

After nearly five decades of conflict, South Sudan gained independence from Sudan in 2011, becoming the newest country in the world. Dr. Sudhir Bunga has served as the U.S. CDC’s Director in South Sudan since 2017. Early in his role, he realized that there were significant gaps in South Sudan’s local public health workforces.
Challenges
In 2017, multiple challenges limited South Sudan's ability to provide quality healthcare services to communities and rapidly respond to disease outbreaks. State and county-based structures that could coordinate with the Ministry of Health (MOH) were either not well-coordinated or not in place. Public health services were delivered out of healthcare facilities that lacked the necessary infrastructure and staff.
Long distances, limited transportation infrastructure, and insecurity related to ongoing conflicts made it difficult to access services at health facilities. These barriers also inhibited trainings for facility-based health workers on program guidelines and best practices in health service delivery.
To address these challenges, the CDC South Sudan country team worked closely with CDC headquarters. The team assessed how available resources could be used to strengthen health systems and build workforce capacity in South Sudan. CDC is a key implementing agency of PEPFAR. Together with global partners, PEPFAR aims to eliminate the global HIV pandemic by 2030. PEPFAR is the largest commitment by any nation to address a single disease in history.
The CDC South Sudan team thoughtfully leveraged PEPFAR resources to expand public health capacity within communities, in healthcare facilities, and subnationally.
The best place to fight HIV is in the community and by the community.
- Alfred Alunyo, CDC South Sudan Care and Treatment Advisor
Interventions
Establishing a community-based public health workforce
In 2019, CDC South Sudan helped establish the country's first community health cadre—the Community Outreach Volunteer (COV) intervention. CDC worked with the South Sudan Ministry of Health (MOH) and the International Center for AIDS Program at Columbia University.
The COV intervention brought HIV care and antiretroviral treatment (ART) to the doorsteps of people living with HIV. This model has expanded access to care and treatment in a country where multiple barriers prevented people from reaching healthcare facilities. COVs travel on foot or by bicycle to the communities or households of people living with HIV.
Volunteers are also recruited from the communities that they are intended to serve. This approach ensures greater community acceptance and minimizes travel distance to reach assigned households. It also cultivates an environment of trust. This has empowered some communities of people living with HIV to meet periodically and motivate each other as a community ART group.
Training health workers for healthcare service quality assurance

In South Sudan—a young nation with limited infrastructure for medical education—the number and quality of well-trained healthcare staff are inadequate to serve the nation's needs. Trained healthcare providers are largely concentrated in the capital city of Juba, resulting in lower quality of services at peripheral healthcare facilities. Regular refresher trainings would help providers enhance their knowledge and skills over time. However, in-service trainings across the country would be costly to organize due to physical access limitations and travel restrictions related to insecurity.
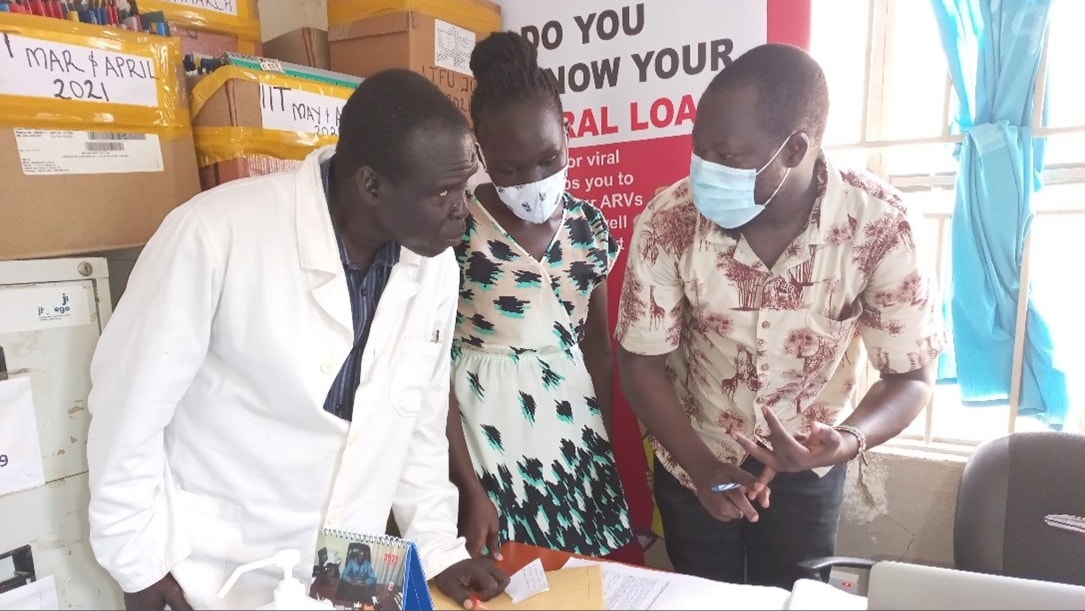
Since 2018, CDC has adopted and expanded Project ECHO (Extension for Community Healthcare Outcomes) in South Sudan to strengthen the capacity of healthcare providers to deliver high-quality HIV services for improved health outcomes. Project ECHO is a collaborative model of medical education and care management that helps clinicians provide expert-level care to patients wherever they live. The project has trained providers at 55 healthcare facilities in South Sudan on best practices in clinical care for HIV, tuberculosis (TB), Ebola, and COVID-19. Through Project ECHO, clinicians, nurses, counselors, laboratory technicians, and pharmacists receive tailored virtual training on disease surveillance, diagnostics, case management, care, treatment, and prevention. CDC has worked with ICAP to design and deliver the training courses.
Project ECHO empowers frontline healthcare workers by providing ongoing professional opportunities directly at their fingertips—whether on their desktops or mobile phones.
- Dr. Onyekachi Ukaejiofo, ICAP
Connecting national and local HIV program sites
Travel restrictions within and outside of Juba have affected the mobility of CDC staff and partners. To support MOH with overseeing local program implementation, Dr. Bunga designed and proposed a new workforce model to serve as the subnational "eyes and ears" for the PEPFAR program in South Sudan. This field team would report to the MOH and receive technical oversight and mentorship directly from CDC. The proposal received wide interagency agreement and approval for implementation.
Since May 2018, CDC and IntraHealth International (IHI) have recruited, trained, and mentored 54 field officers to provide direct oversight, supervision and mentorship to local TB and HIV programs across the 25 PEPFAR-supported counties in the country. CDC and partners have provided extensive one-on-one mentorship and hands-on training to support the field officers.
Impact
Community Outreach Volunteer (COV) program
The COV intervention has led to significant reductions in missed appointments and treatment interruptions in nearly 100 PEPFAR-supported healthcare facilities. In Eastern Equatoria, the rate of missed appointments and treatment interruptions decreased to zero between January and March 2023. ART coverage among people living with HIV (PLHV) nearly tripled, from 12% to 33%, between 2017 and 2023.
Today, most ART refills occur within the community with the support of these volunteers. The COV intervention has evolved significantly, growing from 100 volunteers in 2019 to approximately 1,200 volunteers in 2023. This expansion aims to guarantee uninterrupted access to ART and care services for 55,000 PLWH who are in treatment.
One day, the community health worker cadre will form the backbone of a robust primary health care system in South Sudan.
- Dr. Bunga
Project ECHO
Project ECHO is reducing variations in clinical practice. It is improving the quality of care across healthcare facilities, and ensuring easier and quicker dissemination of guidelines and adaptations. Since 2019, nearly 200 sessions have been completed. Close to 3,500 healthcare workers across South Sudan have been trained through Project ECHO.
Project ECHO NextGen, an advanced, year-long training, was recently launched in 2023. ECHO NextGen will develop the ability of healthcare facilities to respond to infectious disease outbreaks, contributing to overall human resources for health development in clinical healthcare.
Field officers
Establishing field officer positions gave South Sudan's PEPFAR program much-needed visibility into challenges occurring within project sites and demographics at program locations. Field officers have significantly improved PEPFAR program implementation by:
- Facilitating the timely identification and resolution of issues at project sites.
- Supporting timely data reporting.
- Providing hands-on mentorship to providers in person.
- Helping to maintain supply levels at sites.
- Conducting regular performance reviews.
Since the field officers were established, data quality assessments (an exercise to periodically review records and registers to assess the completeness, accuracy, and timeliness of data) have been implemented and routinized. Completeness of HIV data reporting has increased from less than 50% to 100%.
The field officers have significantly contributed to improved quality of care, data quality, and accountability.
- Alex Bolo, CDC South Sudan Senior Strategic Information Advisor
Looking ahead
Even in a complex operating environment with resource constraints, health and public health program management capabilities can be strengthened. CDC's investments toward expanding workforces are seen as a necessary and well-directed priority by South Sudan's government counterparts and donor-development partners. Some initiatives will be sustained and funded to a larger scale by other agencies and organizations in South Sudan.
The work has just begun, has found early but strong roots, and will continue to sustain with good oversight, mentorship, and most importantly, the right kind of champions leading it both within CDC and the host country.
