At a glance
CDC established an office in Kenya in 1979. CDC works with the Ministry of Health (MOH) and other partners to build effective public health collaboration and partnerships to detect, prevent, and respond to global public health threats. CDC’s work aims to protect the health of Americans and public health around the world.

Key accomplishments
- Supported the establishment of Kenya’s National Influenza Center, which conducts surveillance for influenza, COVID-19 and other respiratory pathogens and responds to respiratory disease outbreaks.
- Played a pivotal role in enhancing laboratory standards, resulting in 89 laboratories achieving international accreditation.
- Supported training of over 1,500 global health leaders who graduated from the Field Epidemiology Laboratory Training Program (FELTP). FELTP graduates are the boots-on-the-ground for Kenya’s Ministry of Health, responding to over 80% of outbreaks detected in the country.
- Created a network of more than 20 sub-national Emergency Operations Centers (EOCs) who have responded to more than 100 disease outbreaks as of 2024.
- Supported cutting edge research and the launch of an Applied Science Hub, a pathogen-agnostic laboratory platform to advance molecular detection, strengthen public health preparedness and response capacity, and foster sustainable workforce development in Kenya.
- Supported a measles-rubella vaccination campaign in high-risk counties, resulting in the vaccination of over 5.3 million children.
Global health security

Surveillance systems
CDC conducts surveillance to better understand emerging health threats and how to prevent them. This strengthens Kenya's ability to rapidly detect and respond to disease outbreaks and other health threats. CDC enhances surveillance and health information systems by:
- Supporting the development and implementation of population, facility-based, rapid mortality, and event-based surveillance systems.
- Spearheading state-of-the-art and mobile data collection systems.
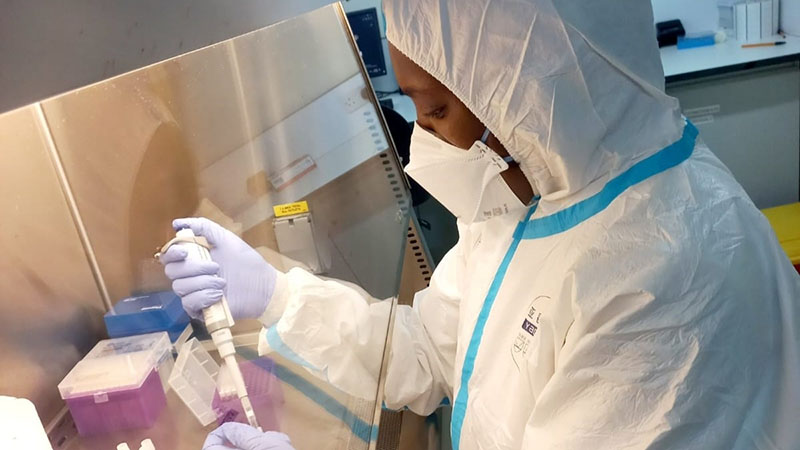
Laboratory systems strengthening
CDC strengthens laboratory systems in Kenya by helping to build the critical laboratory network necessary to assure health security. CDC provides ongoing support to select Kenya Medical Research Institute (KEMRI) laboratories, regional and county laboratories, and the national reference labs on diagnostics, outbreak detection and systems development. Ongoing technical assistance priorities include whole-genome sequencing and diagnostics capacity for endemic and emerging pathogens.
Workforce development
The CDC-supported FETLP is designed to build national, regional, and local capabilities to stop diseases at the source. Kenya’s FELTP implements all three programs—Advanced, Intermediate and Frontline. FELTP residents serve as first responders to prepare and respond to public health emergencies like COVID-19, monkeypox, yellow fever and Ebola.
Emergency response

CDC supported the design and provided equipment for the Kenya National Public Health Emergency Operations Center (EOC) established in 2013. CDC has trained MOH staff in public health emergency management, incident command systems, geographic information systems, risk communication, and through the Public Health Emergency Management Fellowship. The EOC and emergency response capacity built continues to support outbreaks in Kenya for ongoing monkeypox and cholera outbreaks.
HIV and TB
As a key implementer of the U.S. President's Emergency Plan for AIDS Relief (PEPFAR), CDC plays an essential role in the fight against HIV and TB. With unmatched scientific and technical knowledge and long-standing relationships with ministries of health, CDC is uniquely positioned to advance HIV, TB, and other global health security activities that keep Americans safe at home and abroad.
Through PEPFAR, CDC provides critical support to Kenya's public health infrastructure, improving the country's ability to prevent, detect, and respond to HIV, TB, and other infectious diseases and minimizing their risk from entering the U.S.
Immunization
CDC's Global Immunization Program supports the Government of Kenya and the region in developing national policies, strategies, action plans and projects to prevent and control vaccine preventable diseases. CDC Kenya assisted the Government of Kenya in preparing for and accelerating COVID-19 vaccination. CDC’s activities focus on maintaining polio-free status, achieving measles elimination and rubella control, and maintaining elimination of maternal and neonatal tetanus. CDC’s Immunization Program also enhances Kenya’s vaccine-preventable diseases laboratory systems by supporting diagnostics, outbreak detection, and sequencing for polio, measles, and rubella.
Malaria
Kenya’s entire population is at risk for malaria. CDC has collaborated with partners to support implementation of malaria prevention and control activities in Kenya. CDC has also collaborated with KEMRI since 1979 to establish one of the premier malaria research field stations in the world. CDC’s support has helped:
- Evaluate new or combination of existing malaria control interventions and tools
- Conduct surveillance on global threats to malaria treatment, prevention and control
- Advance laboratory methods to monitor and measure impact of malaria prevention, detection, control, and response efforts
Influenza
CDC’s Influenza Program Regional Hub in Kenya works with partners in the East Africa region (Kenya, Uganda, Tanzania, Ethiopia and South Sudan) to ensure public health surveillance and laboratory systems can detect and respond to influenza viruses with pandemic potential. CDC is regularly called upon to provide technical assistance for influenza outbreak investigations, and CDC facilitates specimen-sharing for selection and preparation of flu vaccines. This work is essential to ensuring data captures the diversity of influenza viruses spreading around the world and controlling emerging threats at the source before they reach U.S. borders.
Migration health
CDC’s Global Migration Health Africa Program, located in Kenya, works with local and international partners to address public health needs associated with population mobility. The program is responsible for the medical requirements for U.S. immigration to prevent importation of infectious diseases of public health significance into the United States.
Success story spotlight
Kenya: Fast detection, faster response to stop monkeypox
In July 2024, Kenya reported its first-ever clade Ib monkeypox case. The Kenya Ministry of Health (MOH) detected and responded to the case quickly, thanks to core public health capabilities built and enhanced in partnership with CDC.
Core public health capabilities prove their value
Kenya's response began as soon as a port health officer identified a traveler at the Kenya-Tanzania border who presented with the characteristic monkeypox rash. They had the ability to quickly report the suspected monkeypox case to the MOH because of a digital system built with CDC support. The system monitors for diseases of public health significance among international air travelers and truck drivers crossing into Kenya.
After the traveler was isolated, samples were collected and sent to multiple laboratories to confirm if the rash was due to monkeypox, including to the CDC-supported lab in Nairobi. When the test came back positive for monkeypox virus, results were shared with the Ministry of Health that same day. This swift action set even more wheels in motion.
Disease detectives trained by Kenya's CDC-supported Field Epidemiology and Laboratory Training Program (FELTP) launched into action. "We quickly deployed to investigate the confirmed monkeypox case, identify exposed persons, and monitor contacts for any symptoms that could indicate transmission," said Kenya FELTP resident Dr. Pius Mutuku.
Kenya also activated its CDC-supported Emergency Operations Centers (EOCs) to manage the response. In addition to the country's national EOC, CDC partnered with Kenya to create a network of more than 20 sub-national EOCs that can help control outbreaks closer to the source. As of 2024, these EOCs have responded to more than 100 disease outbreaks.
The right information at the right time saves lives
Critically, the country immediately launched a mass messaging campaign to educate the public about preventive measures and reduce stigma associated with monkeypox. As in many other places, monkeypox misinformation and disinformation is rapidly spreading in Kenya through social media and other platforms. To help combat this, Kenya partners and CDC staff worked together to:
- Hold a press briefing with media outlets to help inform the public
- Develop informational resources to help healthcare workers recognize the signs and symptoms of monkeypox, and take the appropriate infection prevention and control measures to keep themselves and their patients safe
- Share credible, reliable, and actionable messages with people and communities through social media, newspapers, radio, and television.
The messaging campaign had an immediate effect. After hearing about the risks, a second person recognized their own symptoms and sought medical attention at a port of entry along the Kenya-Uganda border. Quick action is critical to finding and stopping further spread of monkeypox.
While the monkeypox situation is still evolving, CDC will continue supporting Kenya as they tackle a disease threat they have never faced before.
"CDC Kenya is supporting the government of Kenya to ensure screening of all travelers at points of entry to prevent importation of diseases and supporting monkeypox response efforts to help keep people safe," said Dr. Maurice Ope of CDC's Kenya office. "A disease threat anywhere is a disease threat everywhere."

![[thumbnail] (hidden)](/global-health/media/images/2025/11/Kenya_thumbnail.jpg)