At a glance

Summary
FluVaxView webpage report posted online October 1, 2020
To reduce the risk of influenza (flu) illness, hospitalization and death, the Centers for Disease Control and Prevention (CDC) recommends routine annual flu vaccination for all people ≥6 months who do not have contraindications1. CDC analyzed data from two telephone surveys, the National Immunization Survey-Flu (NIS-Flu) and the Behavioral Risk Factor Surveillance System (BRFSS), to estimate flu vaccination coverage for the U.S. population during the 2019–20 flu season. Vaccination coverage with ≥1 dose of flu vaccine was 63.7% among children 6 months through 17 years, an increase of 1.2 percentage points from the 2018–19 flu season, and flu vaccination coverage among adults ≥18 years was 48.4%, an increase of 3.1 percentage points from the prior season. Half (51.8%) of persons six months and older were vaccinated during the 2019–20 season, an increase of 2.6 percentage points from the prior season. Flu vaccination coverage has increased for both children and adults over the past two flu seasons. However, racial/ethnic disparities in flu vaccination coverage persisted. Non-Hispanic black children had lower flu vaccination coverage than children in all other racial/ethnic groups, while Hispanic adults and non-Hispanic black adults had lower flu vaccination coverage than non-Hispanic white adults. Interpretation of the estimates in this report should take into account limitations of the surveys, including reliance on self- or parental-report of vaccination status and low response rates, as well as level of consistency with findings from other surveys and data sources.
Getting a flu vaccine will be more important than ever this fall and winter, because it is likely that flu viruses and the virus that causes COVID-19 will both be spreading in the United States. Flu vaccination could help prevent or reduce the severity of flu illness, and reduction of outpatient illnesses, hospitalizations, and intensive care unit admissions could alleviate stress on the U.S. health care system. September and October are good times to get vaccinated; however, as long as flu viruses are circulating, vaccination should continue. To avoid missed opportunities for vaccination, providers should offer vaccination during routine health care visits and hospitalizations. Guidance for vaccine planning during the COVID-19 pandemic is available at https://www.cdc.gov/vaccines/pandemic-guidance/index.html.
Methods
For this report CDC analyzed data from the NIS-Flu for children 6 months through 17 years and the BRFSS for adults ≥18 years to estimate national- and state-level flu vaccination coverage for the 2019–20 flu season. The analyses included data collected from interviews completed during September (BRFSS) or October (NIS-Flu) 2019 through June 2020 and report on vaccinations received between July 1, 2019 and the time of interview or by May 31, 2020 for those interviewed in June.
The NIS-Flu is a national random-digit-dialed cellular telephone survey of households.2 Respondents ≥18 years knowledgeable about the child's vaccinations (hereafter referred to as "parent" in this report) were asked if their child had received a flu vaccination since July 1, 2019, and, if so, in which month; this information was parent-reported and not verified by medical records. For the 18.2% of respondents who indicated their child had been vaccinated but had a missing month of vaccination, month was imputed from other survey respondents with non-missing month of vaccination, matched for week of interview, age group, state of residence, and race/ethnicity. Respondents who indicated the child received a flu vaccination were also asked the kind of place at which the child was vaccinated. The range of the Council of American Survey and Research Organizations (CASRO) response rates for the NIS-Flu for the 2019–20 season was 19.6%–21.6%. The estimates for children are based on n=153,533 completed NIS-Flu interviews.
BRFSS is a state-based random-digit-dialed cellular and landline telephone survey which collects information on a variety of health conditions and risk behaviors from one randomly selected adult ≥18 years in a household. BRFSS includes survey questions asking whether the respondent had received a flu vaccination in the past 12 months, and if so, in which month and year. Responses to the flu vaccination status questions were not verified by medical records. Respondents who did not have either a yes or no response to the flu vaccination status question were excluded from the analysis; this included 0.4% who reported they did not know, 0.1% who refused to answer the question, and 6.8% who most likely ended the interview before the flu question was asked. For 6.6% of BRFSS participants who indicated they had been vaccinated but had a missing month and year of vaccination, the month of vaccination was imputed from other survey respondents with non-missing month of vaccination matched for week of interview, age group, state of residence, and race/ethnicity. Information on high-risk conditions was missing for 1.2% of adults; these respondents were not included in the estimates by risk condition. Estimates are not available for the entire 2019-20 influenza season from the District of Columbia; BRFSS calls in the District of Columbia did not occur during January-June 2020. In addition, calls in New Jersey did not occur during September 2019-April 2020, and estimates are based on interview data from May–June, 2020. The median state BRFSS response rate for a complete or partially complete interview was 49.4% for September–December 2019 and 48.3% for January–June 2020. The estimates for adults are based on n=286,116 completed BRFSS interviews.
Flu vaccination coverage estimates from both surveys were calculated using Kaplan-Meier survival analysis using month of reported flu vaccination to determine cumulative flu vaccination coverage. Coverage estimates for all persons ≥6 months were determined using combined state-level monthly estimates weighted by the age-specific populations of each state.3 All estimates were weighted and analyzed using SAS and SAS-callable SUDAAN statistical software to account for the complex survey designs. For simplified graphical display, only four racial/ethnic groups are displayed (Hispanic, non-Hispanic white only, non-Hispanic black only, and non-Hispanic all other races or multiple races); a more detailed racial/ethnic breakdown of estimates is included as a table weblink in the report. Differences between groups and between 2019–20 and prior season (2018–19) estimates were determined using t-tests with significance at p<0.05. Increases or decreases noted in this report were statistically significant differences.
Results
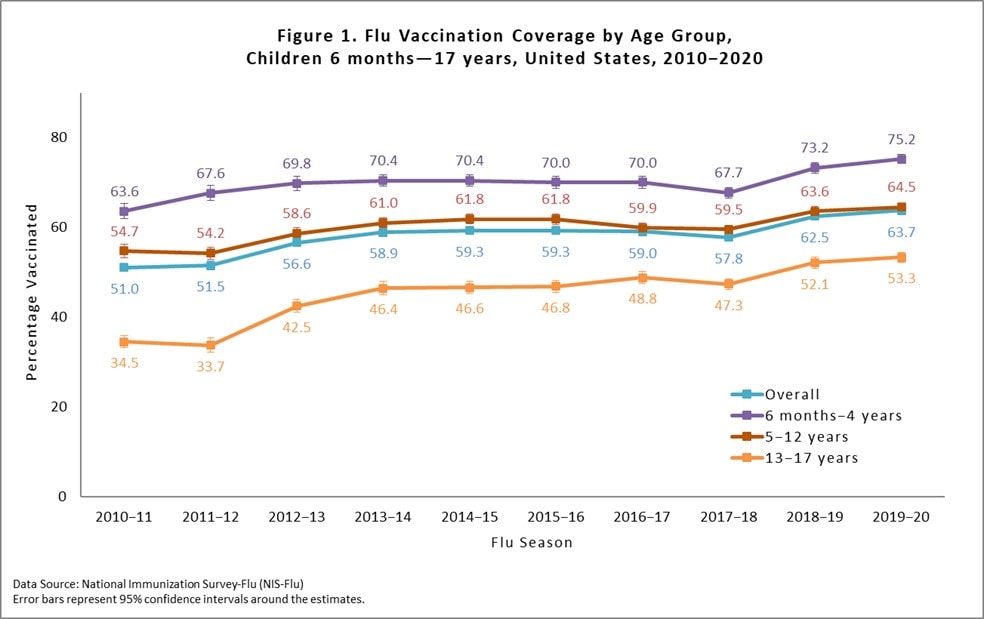
Among children 6 months through 17 years, the percentage receiving ≥1 dose of flu vaccine during the 2019–20 season was 63.7%, which was 1.2 percentage points higher than coverage in the 2018–19 season (62.5%; Figure 1). Flu vaccination coverage increased 2.0 percentage points among children 6 months–4 years, but coverage did not significantly increase among children 5–12 or children 13–17 years compared with the 2018–19 season (Figure 1). As observed in previous flu seasons, flu vaccination coverage was lower for older compared with younger children.
There was large between-state variability in flu vaccination coverage among children, ranging from 51.5% (Mississippi) to 78.3% (Rhode Island; Figure 2). See the interactive FluVaxView application for additional state-level estimates by age-groups and multiple flu seasons.

Flu vaccination coverage for Hispanic children and non-Hispanic black children during the 2019–20 season did not show statistically significant changes compared with the 2018–19 season, while non-Hispanic white children and children in the non-Hispanic other race/ethnicity group had increases in coverage (Figure 3). Significant differences in flu vaccination coverage were observed between racial/ethnic groups. Non-Hispanic black children had lower flu vaccination coverage than children in all other racial/ethnic groups. Children in the other race/ethnicity group had higher flu vaccination coverage than non-Hispanic black, non-Hispanic white, and Hispanic children. In addition to the previous comparisons, non-Hispanic white children had lower flu vaccination coverage than Hispanic children. No other statistically significant pair-wise differences were observed. Flu vaccination coverage estimates for more detailed racial/ethnic groups (Asian, American Indian/Alaska Native, other or multiple races) is provided as a table weblink in the "Additional Flu Vaccination Coverage Estimates" section of this report.

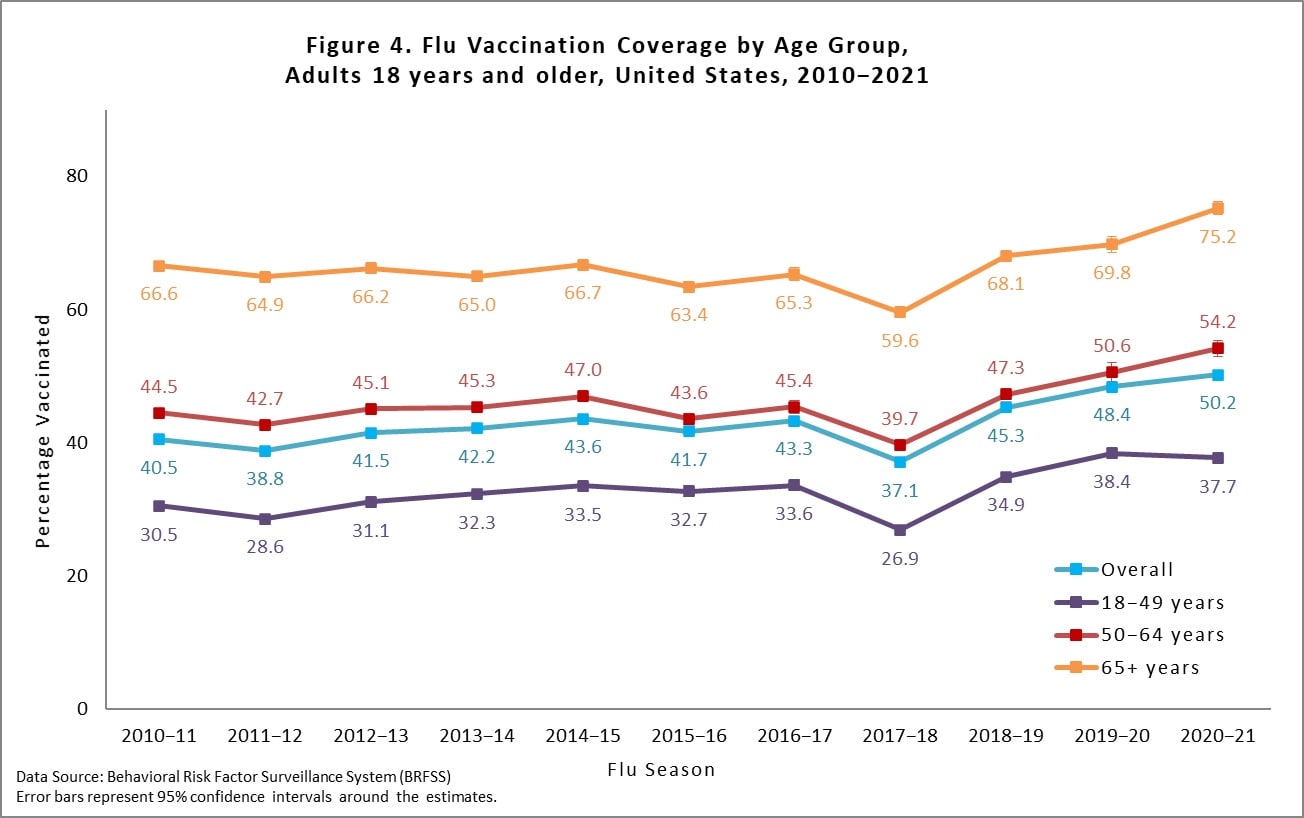
Overall, among adults ≥18 years, flu vaccination coverage was 48.4%, 3.1 percentage points higher than coverage during the 2018–19 season (45.3%; Figure 4). Flu vaccination coverage for 2019–20 was higher for every age group compared with the 2018–19 season (Figure 4). As observed in previous seasons, flu vaccination coverage was higher for older adults compared with younger adults.
There was large between-state variability in flu vaccination coverage among adults, ranging from 41.4% in Idaho to 56.8% in Massachusetts and Rhode Island (Figure 5). See the interactive FluVaxView application for additional state-level estimates by age-groups and multiple flu seasons.

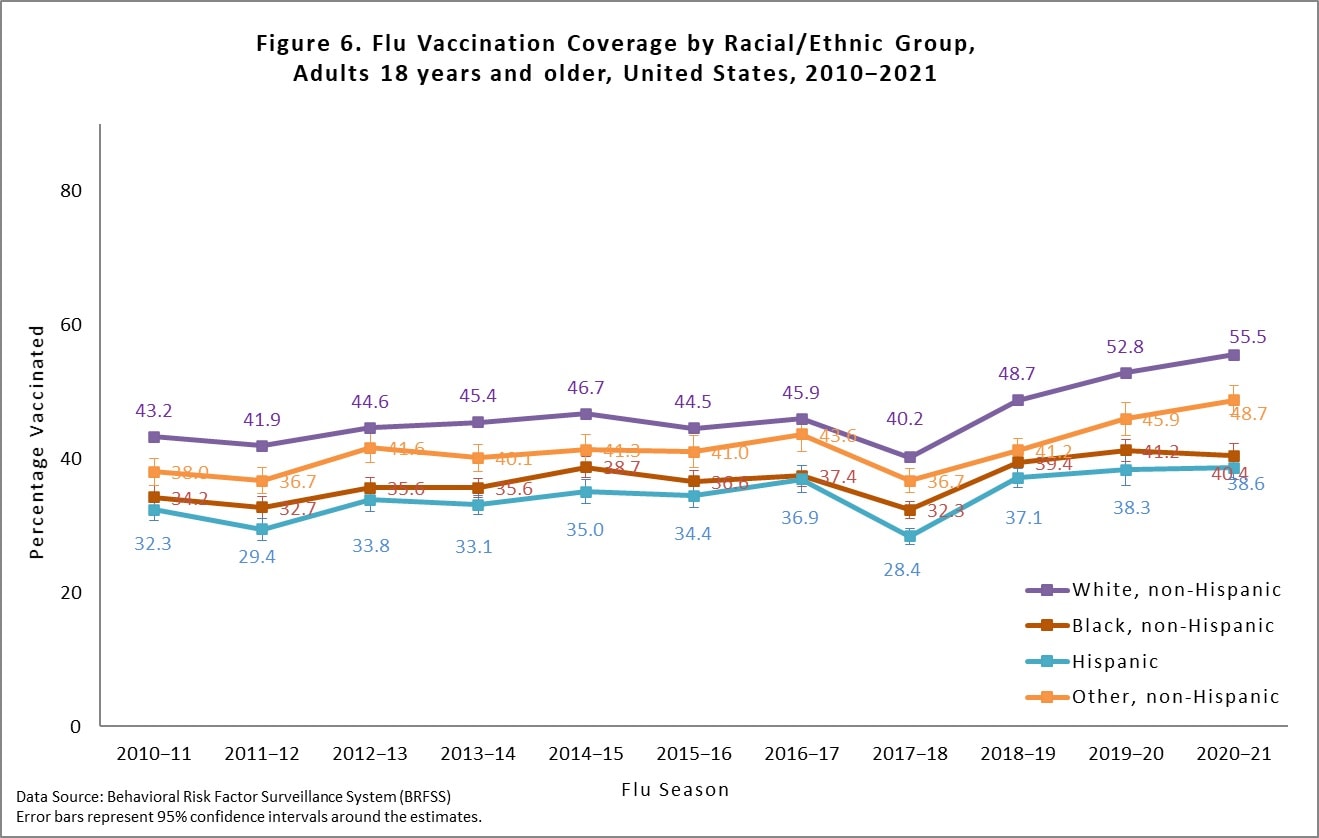
Flu vaccination coverage for Hispanic adults and non-Hispanic black adults during the 2019–20 season did not show statistically significant changes compared with the 2018–19 season, while non-Hispanic white adults and other race/ethnicity adults had increases in coverage (Figure 6). Similar to the 2018–19 season, differences in flu vaccination coverage were observed between racial/ethnic groups. Non-Hispanic white adults had higher flu coverage than non-Hispanic black, Hispanic, and adults of other racial/ethnic groups. Additionally, Hispanic and non-Hispanic black adults had lower flu vaccination coverage than adults of other racial/ethnic groups. Lastly, Hispanic adults also had lower coverage than non-Hispanic black adults. No other statistically significant pair-wise differences were observed. Flu vaccination coverage estimates for more detailed racial/ethnic groups (Asian, American Indian/Alaska Native, other or multiple races) is provided as a table weblink in the "Additional Flu Vaccination Coverage Estimates" section of this report.
Among all people ≥6 months, the percentage vaccinated during the 2019–20 season was 51.8%, 2.6 percentage points higher than coverage in the 2018–19 season (49.2%; Table 1). Coverage during the 2019–20 season increased for white people and people of other non-Hispanic race but did not increase for black or Hispanic people (Table 1). White people had higher flu coverage than black, Hispanic, and other people. Additionally, people of non-Hispanic other races had higher coverage than black and Hispanic people. No other statistically significant pair-wise differences were observed.
Table 1. Flu Vaccination Coverage* among All People 6 months and older, by Race/Ethnicity, United States,† 2019–20 Season
| Race/Ethnicity‡ | %§ ± 95% CI|| | Difference from the 2018–19 Season ± 95% CI |
|---|---|---|
| Overall | 51.8 ± 0.5 | 2.6 ± 0.6¶ |
| White only, non-Hispanic | 54.8 ± 0.5 | 3.8 ± 0.6¶ |
| Black only, non-Hispanic | 45.6 ± 1.2 | 0.9 ± 1.8 |
| Hispanic | 46.6 ± 1.7 | 0.1 ± 2.0 |
| Other, non-Hispanic** | 51.8 ± 2.0 | 4.2 ± 2.4¶ |
* Estimates of the percentage vaccinated are based on interviews conducted September (BRFSS) or October (NIS-Flu) 2019 through June 2020 and reported vaccinations from July 2019 through May 2020.
† Excludes U.S. territories.
‡ Race is self-reported; people of Hispanic ethnicity may be of any race.
§ Percentage vaccinated. Percentages are weighted to the U.S. population. Month of vaccination was imputed for respondents with missing month of vaccination data.
|| Confidence interval (CI) half-widths.
¶ Statistically significant difference between the 2019–20 season and the 2018–19 season by t-test (p<0.05).
** Includes Asian, American Indian/Alaska Native, Native Hawaiian or other Pacific Islander, multiracial, and other races.
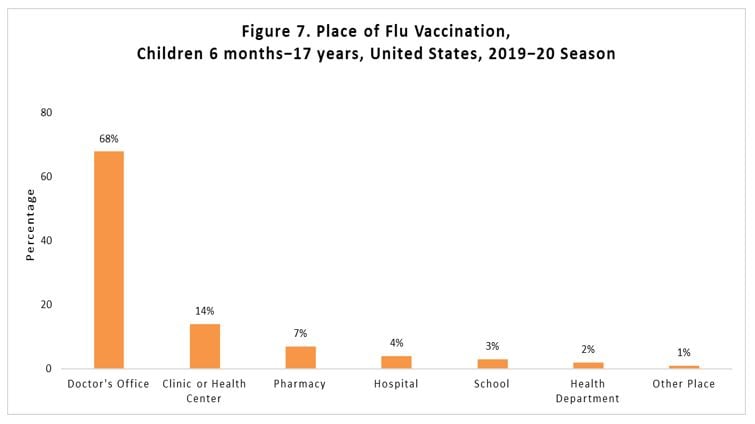
Place of flu vaccination among vaccinated children 6 months through 17 years was most often a doctor's office (69%), followed by clinic/health center (14%), and pharmacy (7%; Figure 7). A weblink to place of flu vaccination by child age groups is included in the additional tables in the next section of this report. Place of flu vaccination for adults from BRFSS is not available for the 2019–20 season; it is collected every 3rd year. The most recent adult place of flu vaccination report is available in Figure 5 at the following link: FluVaxView.
Additional Flu Vaccination Coverage Estimates
Children:
- Flu Vaccination Coverage, by Age Group, Children, United States, 2019–20 Season
- Flu Vaccination Coverage by Sex, Children, United States, 2010–20 Season
- Flu Vaccination Coverage by Race/Ethnicity and Age Group, Children, United States, 2019–20 Season
- Flu Vaccination Coverage for Local Areas and Territories, Children, 2019–20 Season
- Place of Flu Vaccination, Children, United States, 2019–20 Season
Adults:
- Flu Vaccination Coverage, by Age Group and High Risk Status, Adults, United States, 2019–20 Season
- Flu Vaccination Coverage by Sex, Adults, United States, 2019–20 Season
- Flu Vaccination Coverage by Race/Ethnicity and Age Group, Adults, United States, 2019–20 Season
- Flu Vaccination Coverage for Local Areas and Territories, Adults, 2019–20 Season
Limitations
Interpretation of the results in this report should take into account several limitations of the estimates produced from the NIS-Flu and BRFSS surveys. First, survey weighting adjustments may not eliminate all the possible bias from incomplete sample frames; both surveys exclude households with no telephones, and NIS-Flu also excludes households with only landline telephones. Second, response rates for both surveys were low, and flu vaccination coverage may differ between survey respondents and non-respondents; survey weighting adjustments may not adequately control for these differences. Third, there may be errors in flu vaccination status due to recall error of parents for NIS-Flu and of respondents for BRFSS.45 Fourth, errors from incomplete sample frame, nonresponse, and accuracy of reported flu vaccination status might change over time, which could lead to inaccurate assessment of trends in flu vaccination coverage. Fifth, due to BRFSS interviews not being completed in all months, adult estimates for New Jersey may be subject to differential bias compared with estimates based on the full set of interviews from September 2019-June 2020, and adult estimates for the District of Columbia represent vaccination coverage through November rather than through May. The projected DC vaccination coverage estimate for adults would be 55.3% through May 2020, applying the relative increase in DC estimates from November 2017 to May 2018 to the 49.3% estimate for the 2019-20 season. Sixth, estimates differed from National Health Interview Survey (NHIS) estimates, the data source for evaluating progress toward the Healthy People 2020 and 2030 flu vaccination coverage objectives; NHIS uses a different sampling method and in-person interviews but does also rely on self or parental report.67 A recent study found that NIS-Flu estimates were generally higher than NHIS estimates over several flu seasons for children.8 CDC continues to assess consistency between flu vaccination coverage estimates from different surveys and other data sources and evaluate accuracy of estimates from these data sources. For example, given the total number of doses of flu vaccine distributed in the United States in 2019–20 and population estimates, the maximum percentage of all people 6 months and older that could have been vaccinated was 55%. Although 52% were vaccinated according to the results in this report, this estimate may not be the actual proportion vaccinated given the limitations stated above.
CDC is exploring non-survey data sources to track flu vaccination coverage such as claims and other administrative data. While the NIS-Flu estimates for children are available weekly to CDC during the flu season, BRFSS data are not available to produce weekly estimates for adults for flu vaccination. To provide within-season weekly estimates of flu vaccination for adults, CDC acquired projected estimates based on claims data of the number of flu vaccines given at pharmacies in the United States from IQVIA. IQVIA claims-derived flu vaccination coverage was calculated using these projected estimates along with estimates of the percentage of vaccinated adults who received their flu vaccination at a pharmacy in each state (based on BRFSS surveys). The IQVIA claims-derived estimates for the end of flu season coverage from past seasons can be compared with existing estimates based on BRFSS. For national-level estimates, IQVIA claims-derived estimates were within five percentage points of the BRFSS estimates for the 2019-20 and two previous flu seasons. However, state-level estimates show more variability; for the 2018–19 season IQVIA claims-derived and BRFSS estimates differed between 0.5 and 35.5 percentage points across states for 18–64 year-old adults and 0.6 and 34.6 percentage points for adults 65 years and older. CDC continues to evaluate ways to improve the accuracy of IQVIA claims-derived flu vaccination coverage estimates, and plans to launch a Weekly Flu Vaccination Dashboard online via FluVaxView during the fall of 2020, including the IQVIA claims-derived estimates for adults and the weekly NIS-Flu estimates for children.
Discussion
Flu vaccination coverage during the 2019–20 season was higher than coverage during the 2018–19 season for both children and adults. For several seasons prior to the 2018–19 season, flu vaccination coverage had remained the same for children.8 For adults, there was a sizable increase in coverage for the last two consecutive seasons after many flu seasons of small increases, and one recent season with a decrease (though this decrease in 2017-18 was not confirmed by other data sources).9 Yet, despite these increases, the Healthy People 2020 national target of 70% of children and adults vaccinated against flu was not achieved, with coverage lagging by 6 percentage points for children and almost 20 percentage points for adults.10 Reflecting this lack of substantial progress for adults, the newly launched Healthy People 2030 target for flu vaccination of persons ≥6 months has also been set at 70%.7 Furthermore, flu vaccination coverage in some states and among some racial/ethnic groups is still far from optimal.
Getting a flu vaccine is more important than ever this fall and winter because flu and COVID-19 may both be spreading in the United States at the same time. CDC recommends that all people 6 months and older get a yearly flu vaccine, with rare exceptions. Vaccinating people at high risk is especially important to decrease their risk of severe flu illness. Many people at higher risk from flu complications also are at higher risk from COVID-19. Getting a flu vaccine will not protect against COVID-19; however, flu vaccination has many other important benefits. Flu vaccines have been shown to reduce the risk of flu illness, hospitalization and death.
A flu vaccination not only reduces a person's risk from flu but may also help conserve potentially scarce healthcare resources. During the COVID-19 pandemic, reducing the overall burden of respiratory illnesses is important to protect vulnerable populations at risk for severe illness, the healthcare system, and other critical infrastructure. Thus, healthcare providers should use every opportunity during the flu vaccination season to administer flu vaccines to all eligible persons.
September and October are good times to get vaccinated; however, as long as flu viruses are circulating vaccination should continue. For the 2020–21 season, vaccine manufacturers have projected they will provide as many as 194–198 million doses of flu vaccine, which is more than the 175 million dose record set during the 2019–20 flu season.
How and where people get a flu vaccine may change due to the COVID-19 pandemic. Healthcare providers can find a collection of federal resources designed to guide vaccine planning during the COVID-19 pandemic at https://www.cdc.gov/vaccines/pandemic-guidance/index.html. CDC is working with healthcare providers and state and local health departments to develop contingency plans on how to vaccinate people against flu without increasing their risk of exposure to the virus that causes COVID-19. Some settings that usually provide flu vaccination, like workplaces and schools, may not offer vaccination this upcoming season because of challenges with maintaining social distancing. When going to get a flu vaccination, people should practice everyday preventive actions and follow CDC recommendations for lowering the risk of catching flu or COVID-19. People can ask their doctor, pharmacist, or health department if they are following CDC's vaccination pandemic guidance. Any vaccination location following CDC's guidance should be a safe place to get a flu vaccine. For more information please visit https://www.cdc.gov/flu/season/faq-flu-season-2020-2021.htm.
- Grohskopf, L.A., et al., Prevention and Control of Seasonal Influenza with Vaccines: Recommendations of the Advisory Committee on Immunization Practices – United States, 2020-21 Influenza Season. MMWR Recomm Rep, 2020. 69(8): p. 1-24.
- Wolter, K.K., et al., Statistical Methodology of the National Immunization Survey, 2005-2014. Vital Health Stat 1, 2017(61): p. 1-107.
- Furlow-Parmley, C., et al., Combining estimates from two surveys: an example from monitoring 2009 influenza A (H1N1) pandemic vaccination. Stat Med, 2012. 31(27): p. 3285-94.
- Brown, C., et al., Validity of parental report of influenza vaccination in young children seeking medical care. Vaccine, 2011. 29(51): p. 9488-92.
- Irving, S.A., et al., Evaluation of self-reported and registry-based influenza vaccination status in a Wisconsin cohort. Vaccine, 2009. 27(47): p. 6546-9.
- CDC. FluVaxView, Influenza vaccination coverage. 2019 [cited 2019; Available from: https://www.cdc.gov/fluvaxview/.
- Healthy People 2030: Increase the proportion of people who get the flu vaccine every year — IID-09. 2020 8/31/2020]; Available from: https://odphp.health.gov/healthypeople/objectives-and-data/browse-objectives/vaccination/increase-proportion-people-who-get-flu-vaccine-every-year-iid-09.
- Santibanez, T.A., et al., Trends in Childhood Influenza Vaccination Coverage, United States, 2012-2019. Public Health Rep, 2020. 135(5): p. 640-649.
- CDC. Estimates of influenza vaccination coverage among adults–United States, 2017-18 flu season. 2018
- 2020, H.P. 2020 Topics & objectives–immunization and infectious diseases. 2019 [cited 2019; Available from: https://odphp.health.gov/healthypeople/objectives-and-data/browse-objectives/infectious-disease.
