At a glance

Summary
The Advisory Committee on Immunization Practices (ACIP) recommends that all health care personnel (HCP) receive an annual influenza vaccination to reduce influenza-related morbidity and mortality among HCP and their patients12. While not specific to HCP, ACIP also recommends that all persons aged ≥6 months be vaccinated with COVID-19 vaccines and remain up to date3. During March 26–April 16, 2024, CDC conducted an opt-in Internet panel survey of 2,750 U.S. HCP to estimate influenza vaccination coverage during the 2023–2024 influenza season as well as receipt of the updated 2023–24 COVID-19 vaccine. Overall, 75.4% of HCP reported receiving influenza vaccination during the 2023–2024 season and 31.3% reported having received the updated 2023–24 COVID-19 vaccine. Influenza and updated 2023–24 COVID-19 vaccination coverage were lowest among assistants and aides and those whose employer neither required nor recommended the vaccines. Influenza vaccination coverage was lowest among those working in long-term care facilities (LTC) and home health care settings, and updated 2023–24 COVID-19 vaccination coverage was lowest among those working in ambulatory settings. Influenza vaccination coverage was highest among pharmacists (93.9%) and physicians (93.0%) and HCP who worked in hospital settings (89.1%), similar to previous seasons. Updated 2023–24 COVID-19 vaccination coverage was highest among physicians (52.7%) and HCP who worked in LTC and home health care settings (34.8%). Maximizing HCP influenza and COVID-19 vaccination uptake among HCP and patients in the upcoming season is important to reduce influenza and COVID-19 related morbidity and mortality among HCP and their patients, and decrease absenteeism among HCP due to respiratory illness. Implementing workplace strategies shown to improve influenza and COVID-19 vaccination coverage among HCP, including vaccination requirements and providing vaccines onsite, could increase vaccination coverage4.
Methods
An Internet panel survey of HCP was conducted from March 26, 2024–April 16, 2024, to provide estimates of influenza and COVID-19 vaccination coverage among HCP during the 2023–24 influenza season. Respondents were recruited from two preexisting national opt-in Internet sources: MedscapeA , a medical website managed by WebMD Health Professional Network, and general population Internet panels operated by DynataB. Responses were weighted to the distribution of the U.S. population of HCPC by occupationD, age, sex, race and ethnicity, work setting, and U.S. Census Bureau region. A poststratification weight for each responding person in the survey was calculated by fitting a generalized exponential model and estimating the model parameters using calibration equations5. Among 2,892 eligible participants, a total of 2,786 completed the survey (completion rate=96.3%E). Thirty-six participants were excluded because they indicated working in a setting other than those listed, and the verbatim description did not qualify as a health care setting, leaving 2,750 respondents in the analytic sample.
Weighted proportions and corresponding 95% confidence intervals (CIs) for two vaccination measures (influenza vaccination coverage for the 2023–24 season and receipt of updated 2023–24 COVID-19 vaccination coverageF) were estimated for each work setting, occupation, and demographic characteristic. Long-term care (LTC) and home health care settings include nursing homes, assisted living facilities, other long-term care facilities, home health agencies, and home health care. Employer requirements for the two vaccination measures were assessed through two separate questionsG. Annual influenza vaccination coverage for all work settings and occupations from the past ten seasons from similar annual surveys conducted since the 2010–11 influenza season67 are shown to examine trends in HCP influenza coverage over time, by occupation and work setting. The Korn-Graubard method was used to calculate CIs for proportions, assuming that the weighted estimates were approximately unbiasedH. CDC's National Center for Health Statistics reliability criteria for proportions were applied to the estimates in the descriptive analyses of HCP characteristics and attitudes toward influenza and updated 2023–24 COVID-19 vaccines8. T-tests were used to assess differences in the estimated influenza and COVID-19 vaccination coverage between subgroups. Rao-Scott chi-squared testing was used to assess differences in the estimated influenza vaccination coverage between seasons; p<0.05 was considered statistically significant. SAS/STAT survey procedures (version 9.4; SAS Institute) were used to conduct all analyses.
Results
Overall, 75.4% of HCP reported having received an influenza vaccination during the 2023-2024 season, similar to the 75.9% reported in the 2022–2023 season (Table 1). Among all HCP, influenza vaccination coverage over the previous ten seasons ranged from 77.3%-81.1%, steadily increased from the 2014–2015 season through the 2018–2019 seasons, and then decreased between the 2019–2020 and 2020–2021 seasons and between the 2021–2022 and 2023–2024 seasons after an apparent increase in 2021–2022 (Figure 1). Similar patterns were seen for HCP working in ambulatory care and other clinical settings. While coverage among HCP working in hospitals declined from a high of 95.2% in 2018–2019 to 85.7% in 2022–23 and 89.1% in 2023-2024, coverage among HCP working in LTC settings has remained stable from 2015–2016 (69.2%) through 2023–2024 (65.2%) (Figure 1). As in previous seasons, influenza vaccination coverage in 2023–2024 was highest among HCP working in hospitals (89.1%) and lowest among HCP working in LTC and home health care settings (65.2%) (Table 1, Figure 1). Influenza vaccination coverage was highest among pharmacists (93.9%), physicians (93.0%), nurses (87.6%), and nurse practitioners and physician assistants (85.7%) and lower among other clinical personnel (81.8%), non-clinical personnel (69.5%), and assistants/aides (63.2%); similar patterns were seen in previous seasons (Table 1, Figure 2). Estimates and 95% CIs for influenza seasons 2014–2015 through 2023–2024 are reported in the supplemental Table S1.
During the 2023–2024 season, significantly higher influenza vaccination coverage was reported among Asian, non-Hispanic HCP (89.2%) than White, non-Hispanic HCP (75.9%); HCP with either a master's, professional, or doctoral degree (83.7%) than among those with some college education or less (59.5%). Influenza vaccination coverage was also highest among HCP who were aged ≥60 years (80.7%), HCP who reported working in a non-rural area (76.1%), and the Midwest region (80.4%). No statistically significant changes in influenza vaccination coverage compared with the 2022–2023 season were observed in any HCP group.
Table 1. Receipt of influenza vaccination during 2022-2023 and 2023-2024 influenza seasons among health care personnel, by selected characteristics — Internet panel surveys*, United States, April 2024
| 2022–23 Influenza season | 2023–24 Influenza season | ||||
|---|---|---|---|---|---|
| Characteristic | No. (weighted %) | Weighted % vaccinated (95% CI)† | No. (weighted %) | Weighted % vaccinated (95% CI)† | Percentage point change in weighted % vaccinated, 2022-2023 to 2023-2024 (95% CI) |
| Total | 3,437 | 75.9 (73.1, 78.6) | 2,750 | 75.4 (72.4, 78.3) | -0.5 (-4.4, 3.5) |
| Age group, years | |||||
| 18-29 (Ref) | 422 (15.8) | 72.7 (65.5, 79.2) | 167 (12.7) | 72.5 (61.5, 81.8) | -0.2 (-12.0, 11.6) |
| 30-44 | 1,585 (43.2) | 72.6 (67.4, 77.4) | 1,071 (45.5) | 74.8 (69.9, 79.3) | 2.2 (-4.5, 8.9) |
| 45-59 | 979 (28.1) | 78.5 (73.9, 82.6) | 985 (27.9) | 74.9 (70.0, 79.5) | -3.6 (-9.8, 2.7) |
| 60+ | 449 (12.9) | 85.3 (79.3, 90.1)§ | 525 (13.8) | 80.7 (72.4, 87.4) | -4.6 (-13.4, 4.3) |
| Race and ethnicity¶ | |||||
| White, non-Hispanic (Ref) | 2,164 (60.1) | 76.2 (72.3, 79.9) | 1,701 (58.9) | 75.9 (72.6, 79.0) | -0.3 (-5.2, 4.6) |
| Asian, non-Hispanic | 245 (6.6) | 84.0 (72.0, 92.3) | 220 (6.7) | 89.2 (80.7, 94.8)§ | 5.2 (-6.3, 16.7) |
| Black, non-Hispanic | 405 (15.3) | 70.4 (62.6, 77.3) | 322 (16.9) | 70.5 (59.9, 79.7) | 0.1 (-11.7, 12.0) |
| Hispanic | 503 (15.1) | 78.8 (72.2, 84.4) | 420 (14.5) | 74.5 (64.4, 82.9) | -4.3 (-14.9, 6.4) |
| Other, non-Hispanic | 116 (2.8) | —** | 81 (3.0) | —** | -0.8 (-23.5, 21.9) |
| Education | |||||
| Some college education or less (Ref) | 1,035 (27.1) | 63.4 (56.7, 69.7) | 635 (28.9) | 59.5 (53.5, 65.3) | -3.9 (-12.5, 4.6) |
| Associate or bachelor’s degree | 1,113 (47.2) | 79.4 (75.4, 83.0)§ | 858 (43.9) | 80.8 (75.6, 85.3)§ | 1.4 (-4.6, 7.4) |
| Master’s, professional, or doctoral degree | 1,289 (25.8) | 82.8 (78.2, 86.7)§ | 1,254 (27.2) | 83.7 (79.1, 87.5)§ | 0.9 (-4.9, 6.7) |
| Occupation†† | |||||
| Physician (Ref) | 354 (3.5) | 94.5 (90.1, 97.3) | 355 (3.8) | 93.0 (88.5, 96.2) | -1.5 (-6.3, 3.4) |
| Nurse practitioner/Physician assistant | 219 (1.6) | 91.0 (86.2, 94.5) | 219 (1.7) | 85.7 (79.9, 90.3)§ | -5.3 (-11.6, 1.0) |
| Nurse | 217 (18.2) | 88.1 (81.7, 92.9)§ | 220 (17.8) | 87.6 (80.7, 92.7) | -0.5 (-8.3, 7.2) |
| Pharmacist | 322 (1.3) | 90.7 (86.8, 93.7) | 328 (1.4) | 93.9 (90.5, 96.3) | 3.2 (-1.1, 7.5) |
| Other clinical personnel§§ | 601 (21.0) | 82.5 (77.3, 86.9)§ | 592 (21.4) | 81.8 (76.9, 86.0)§ | -0.7 (-7.1, 5.7) |
| Assistant/Aide | 1,083 (23.7) | 62.8 (59.3, 66.1)§ | 698 (23.5) | 63.2 (58.5, 67.7)§ | 0.4 (-5.2, 6.0) |
| Non-clinical personnel¶¶ | 612 (30.5) | 70.6 (62.8, 77.6)§ | 307 (30.3) | 69.5 (61.5, 76.8)§ | -1.1 (-11.3, 9.2) |
| Work setting*** | |||||
| Hospital (Ref) | 1,125 (39.4) | 85.7 (81.3, 89.4)§ | 929 (38.8) | 89.1 (84.8, 92.5)§ | 3.4 (-2.0, 8.8) |
| Ambulatory care | 1,083 (32.4) | 75.3 (70.9, 79.4) | 991 (37.4) | 74.6 (69.8, 79.0) | -0.7 (-6.8, 5.4) |
| Long-term care facility/Home health care††† | 1,029 (28.1) | 68.3 (61.4, 74.5)§ | 660 (26.5) | 65.2 (58.0, 71.9)§ | -3.0 (-12.3, 6.2) |
| Other clinical setting§§§ | 674 (11.9) | 68.5 (61.3, 75.0)§ | 573 (9.7) | 68.0 (59.2, 76.0) | -0.5 (-11.0, 10.0) |
| Location of primary workplace | |||||
| Rural (Ref) | 555 (15.2) | 65.1 (53.9, 75.3) | 370 (13.8) | 70.9 (61.3, 79.2) | 5.7 (-7.7, 19.1) |
| Non-rural | 2,876 (84.8) | 77.7 (75.1, 80.2)§ | 2,376 (86.2) | 76.1 (72.9, 79.2) | -1.6 (-5.6, 2.4) |
| U.S. Census Bureau region | |||||
| Northeast (Ref) | 661 (17.8) | 79.3 (73.0, 84.7) | 620 (18.0) | 73.2 (64.9, 80.5) | -6.1 (-15.5, 3.3) |
| Midwest | 781 (22.0) | 75.0 (69.4, 80.1) | 588 (24.1) | 80.4 (73.0, 86.6) | 5.4 (-2.9, 13.7) |
| South | 1,299 (37.6) | 75.5 (69.9, 80.5) | 985 (35.6) | 74.7 (70.3, 78.8) | -0.8 (-7.4, 5.8) |
| West | 690 (22.6) | 74.4 (68.1, 80.0) | 552 (22.3) | 72.9 (65.9, 79.2) | -1.5 (-10.1, 7.1) |
| Employer influenza vaccination requirement | |||||
| Required (Ref) | 1,345 (41.6) | 95.9 (93.6, 97.5) | 980 (39.2) | 97.5 (95.9, 98.7) | 1.7 (-0.6, 3.9) |
| Recommended | 1,316 (38.8) | 70.2 (64.2, 75.8)§ | 1,092 (38.6) | 74.1 (69.1, 78.7)§ | 3.9 (-3.4, 11.2) |
| Not required or recommended | 776 (19.6) | 44.8 (38.9, 50.9)§ | 678 (22.3) | 38.8 (32.6, 45.2)§ | -6.0 (-14.5, 2.5) |
| Offered influenza vaccine onsite†††† | |||||
| Yes (Ref) | 1,146 (58.6) | 70.3 (63.8, 76.2) | 967 (54.6) | 74.2 (68.6, 79.3) | 3.9 (-4.0, 11.9) |
| No | 946 (41.4) | 49.5 (44.2, 54.9)§ | 803 (45.4) | 45.5 (39.7, 51.4)§ | -4.0 (-11.8, 3.8) |
Abbreviation: CI = confidence interval; Ref = referent group.
*Respondents were recruited from two preexisting national opt-in Internet sources: Medscape (https://www.medscape.com), a medical website managed by WebMD Health Professional Network, and general population Internet panels operated by Dynata (Dynata_Panel_Book.pdf).† Modified Clopper-Pearson 95% CI according to the approach of Korn and Graubard (https://www150.statcan.gc.ca/n1/en/pub/12-001-x/1998002/article/4356-eng.pdf?st = nQVSWv1i).
§Statistically significant (p<0.05) when compared with ref in the same season.
¶Race and ethnicity were self-reported. Respondents identified as Hispanic might be of any race. The "Other" race category included persons who identified as American Indian or Alaska Native, Native Hawaiian or other Pacific Islander, and persons who selected multiple races.
**Estimates do not meet the National Center for Health Statistics' standards of reliability. https://www.cdc.gov/nchs/data/series/sr_02/sr02_175.pdf.
††Excludes students.
§§Includes dentists, allied health professionals, technicians and technologists, emergency technicians, emergency medical technicians, and paramedics.
¶¶Includes administrative support staff members and managers, and non-clinical support staff members.
***Respondents could select more than one work setting. Each work setting is represented by a separate variable with two values (yes and no, where reference value is no).
†††Nursing home, assisted living facility, other long-term care facility, home health agency, or home health care.
§§§Includes dentist office or dental clinic, pharmacy, emergency medical services, and other settings where clinical care or related services were provided to patients.
¶¶¶Rurality was defined using zip codes in which >50% of the population resides in a nonmetropolitan county, a rural U.S. Census Bureau tract, or both, according to the Health Resources and Services Administration's definition of rural population. https://www.hrsa.gov/rural-health/about-us/what-is-rural.
****https://www2.census.gov/geo/pdfs/maps-data/maps/reference/us_regdiv.pdf.
††††Excludes those with employer influenza vaccination requirement.
Figure 1. Percentage of health care personnel who received influenza vaccination, by work setting* — Internet panel surveys†, United States, 2014-2015 through 2023-2024 influenza seasons§
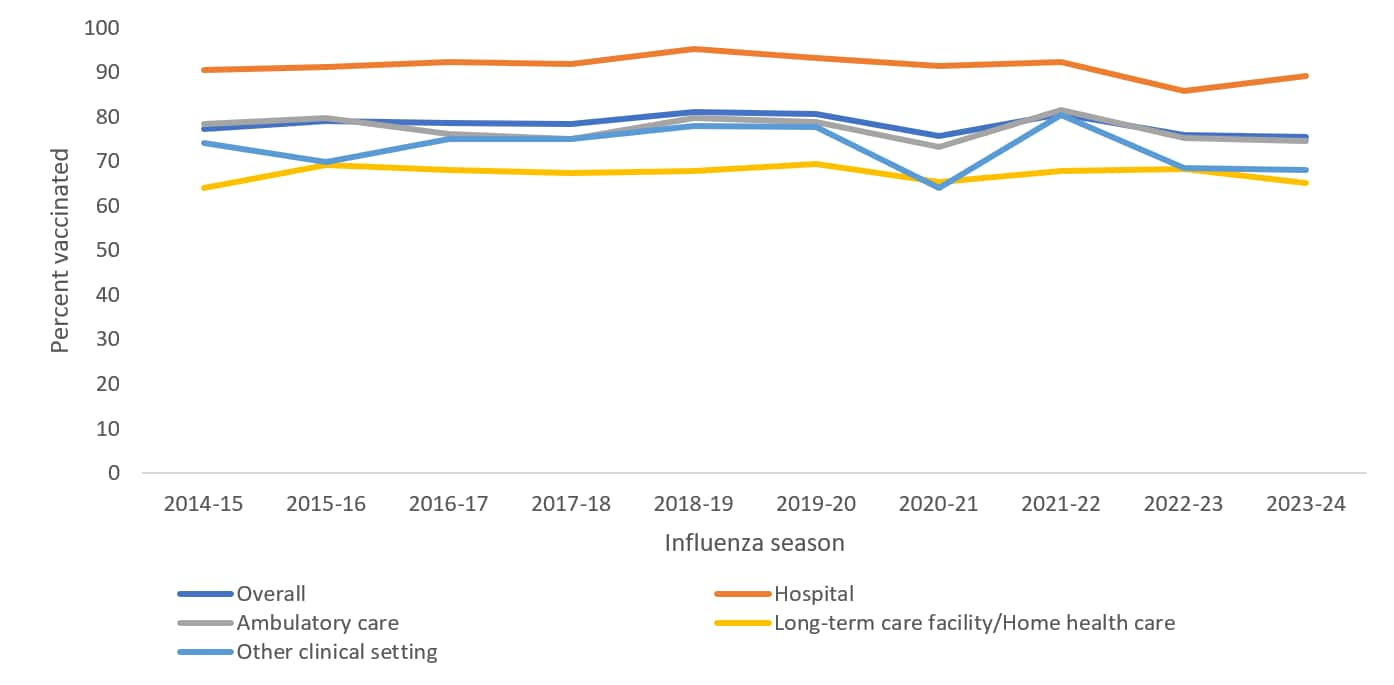
*Respondents could select more than one work setting. The other clinical setting category includes dentist office or dental clinic, pharmacy, emergency medical services, and other settings where clinical care or related services were provided to patients.
†Respondents were recruited from two preexisting national opt-in Internet sources: Medscape (https://www.medscape.com), a medical website managed by WebMD Health Professional Network, and general population Internet panels operated by Dynata (Dynata_Panel_Book.pdf).
§During the 2020-2021 influenza season, a weighting methodological change was implemented. Prior to the 2020-2021 influenza season, weights were calculated to population control totals controlling for the main effects (occupation, age group, race and ethnicity, sex, work setting, and Census region); From the 2020-2021 influenza season and onward, interaction terms between occupation and the other main effects were added in the weighting model. Influenza Vaccination Coverage Among Health Care Personnel — United States, 2020–21 Influenza Season | FluVaxView | Seasonal Influenza (Flu) | CDC
Figure 2. Percentage of health care personnel who received influenza vaccination, by occupation* — Internet panel surveys†, United States, 2014-2015 through 2023-2024 influenza seasons§
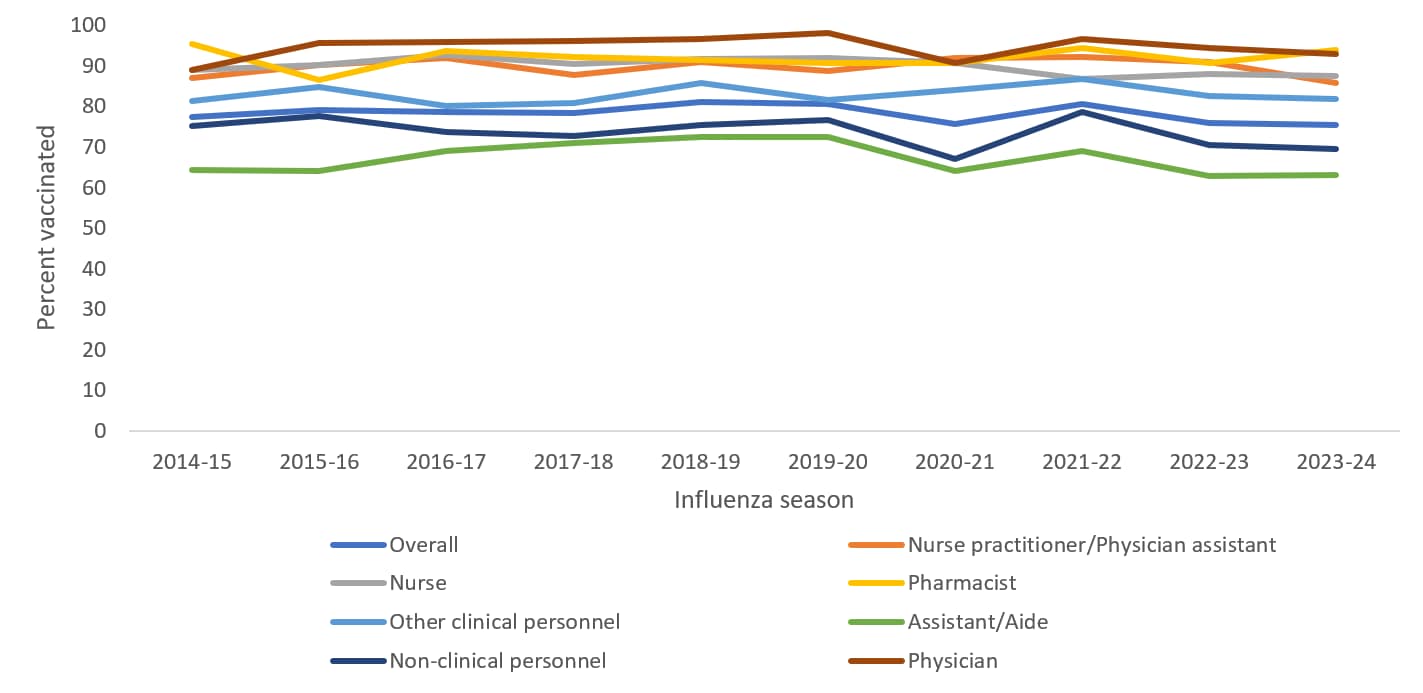
*Other clinical personnel include dentists, allied health professionals, technicians and technologists, emergency medical technicians, and paramedics. Non-clinical personnel includes administrative support staff members and managers, and non-clinical support staff members.
†Respondents were recruited from two preexisting national opt-in Internet sources: Medscape (https://www.medscape.com), a medical website managed by WebMD Health Professional Network, and general population Internet panels operated by Dynata (Dynata_Panel_Book.pdf).
§During the 2020-2021 influenza season, a major weighting methodological change was implemented. Prior to the 2020-2021 influenza season, weights were calculated to population control totals controlling for the main effects (occupation, age group, race and ethnicity, sex, work setting, and Census region); From the 2020-2021 influenza season and onward, interaction terms between occupation and the other main effects were added in the weighting model. Influenza Vaccination Coverage Among Health Care Personnel — United States, 2020–21 Influenza Season | FluVaxView | Seasonal Influenza (Flu) | CDC.
Overall, 31.3% of HCP reported having received the updated 2023–24 COVID-19 vaccine (Table 2), compared with 38.6% who reported having received a COVID-19 bivalent vaccine during the 2022–2023 survey7. Receipt of the 2023–24 updated COVID-19 vaccine was highest among Asian, non-Hispanic HCP (53.4%), physicians (52.7%), HCP aged ≥60 years (45.0%), and those who reported receiving an influenza vaccine in 2023-2024 (39.2%). Receipt of the updated 2023–24 COVID-19 vaccine was lowest among HCP who were aged 30-44 years (28.5%), Hispanic (28.7%), had some college education or less (25.4%), were assistants/aides (27.7%), and working in ambulatory care (26.1%) (Table 2).
Table 2. Receipt of updated 2023-24 COVID-19 vaccine* among health care personnel, by selected characteristics — Internet panel surveys†, United States, April 2024
| Characteristic | Total no. (weighted %) | Receipt of updated 2023-24 COVID-19 vaccination (95% CI)§ |
|---|---|---|
| Total | 2,749 | 31.3 (28.3, 34.5) |
| Age group, years | ||
| 18-29 (Ref) | 167 (12.7) | 30.1 (19.6, 42.3) |
| 30-44 | 1,071 (45.6) | 28.5 (23.9, 33.4) |
| 45-59 | 985 (27.9) | 29.8 (24.6, 35.4) |
| 60+ | 524 (13.8) | 45.0 (37.0, 53.2)¶ |
| Race and ethnicity ** | ||
| White, non-Hispanic (Ref) | 1,700 (58.9) | 29.6 (25.8, 33.6) |
| Asian, non-Hispanic | 220 (6.7) | 53.4 (39.3, 67.0)¶ |
| Black, non-Hispanic | 322 (17.0) | 29.7 (21.9, 38.4) |
| Hispanic | 420 (14.5) | 28.7 (20.8, 37.7) |
| Other, non-Hispanic | 81 (3.0) | —†† |
| Education | ||
| Some college education or less (Ref) | 635 (28.9) | 25.4 (20.1, 31.2) |
| Associate or bachelor’s degree | 858 (43.9) | 30.4 (25.2, 35.9) |
| Master’s, professional, or doctoral degree | 1,253 (27.2) | 39.1 (33.7, 44.7)¶ |
| Occupation§§ | ||
| Physician (Ref) | 354 (3.8) | 52.7 (45.5, 59.8) |
| Nurse practitioner/Physician assistant | 219 (1.7) | 29.4 (23.1, 36.3)¶ |
| Nurse | 220 (17.8) | 29.8 (21.6, 39.0)¶ |
| Pharmacist | 328 (1.4) | 39.8 (33.5, 46.5)¶ |
| Other clinical personnel ¶¶ | 592 (21.4) | 34.1 (28.0, 40.6)¶ |
| Assistant/Aide | 698 (23.5) | 27.7 (23.5, 32.3)¶ |
| Non-clinical personnel *** | 307 (30.3) | 30.1 (23.2, 37.7)¶ |
| Work setting††† | ||
| Hospital | 929 (38.8) | 33.9 (28.6, 39.6) |
| Ambulatory care | 990 (37.4) | 26.1 (21.7, 30.8)¶ |
| Long-term care facility/Home health care§§§ | 660 (26.5) | 34.8 (28.4, 41.6) |
| Other clinical setting ¶¶¶ | 573 (9.7) | 28.1 (20.1, 37.3) |
| Location of primary workplace **** | ||
| Rural (Ref) | 370 (13.8) | 25.7 (17.2, 35.8) |
| Non-rural | 2,375 (86.2) | 32.2 (28.9, 35.6) |
| U.S. Census Bureau region†††† | ||
| Northeast (Ref) | 620 (18.0) | 32.8 (26.1, 40.1) |
| Midwest | 588 (24.1) | 33.3 (26.0, 41.1) |
| South | 984 (35.6) | 27.7 (23.1, 32.7) |
| West | 552 (22.3) | 33.7 (26.9, 41.0) |
| Employer COVID-19 vaccination recommendation | ||
| Required (Ref) | 265 (12.5) | 55.6 (45.0, 65.7) |
| Recommended | 1,294 (47.7) | 38.1 (33.0, 43.3)¶ |
| Not required or recommended | 1,190 (39.8) | 15.7 (12.6, 19.2)¶ |
| Offered updated COVID-19 vaccine onsite§§§§ | ||
| Yes (Ref) | 712 (26.0) | 40.8 (33.8, 48.2) |
| No | 1,772 (74.0) | 23.3 (20.0, 26.9)¶ |
| Receipt of influenza vaccine during 2023–24 | ||
| No (Ref) | 591 (24.6) | 7.2 (4.7, 10.5) |
| Yes | 2,158 (75.4) | 39.2 (35.4, 43.1)¶ |
Abbreviations: CI = confidence interval; Ref = referent group.
*Respondents were considered to have received an updated 2023-24 COVID-19 vaccine if they responded "Yes" to the question, "An updated COVID-19 vaccine (2023-2024 formula) became available in September 2023. Have you received an updated 2023-24 COVID-19 vaccine?"
†Respondents were recruited from two preexisting national opt-in Internet sources: Medscape (https://www.medscape.com), a medical website managed by WebMD Health Professional Network, and general population Internet panels operated by Dynata (Dynata_Panel_Book.pdf).
§Modified Clopper-Pearson 95% CI according to the approach of Korn and Graubard (https://www150.statcan.gc.ca/n1/en/pub/12-001-x/1998002/article/4356-eng.pdf?st = nQVSWv1i).
¶Statistically significant (p<0.05) when compared with Ref.
**Race and ethnicity were self-reported. Respondents who identified as Hispanic might be of any race. The "Other" race category included persons who identified as American Indian or Alaska Native, Native Hawaiian or other Pacific Islander, and persons who selected multiple races.
††Estimate does not meet CDC's National Center for Health Statistics' standards of reliability (https://www.cdc.gov/nchs/data/series/sr_02/sr02_175.pdf).
§§Excludes students (N=31).
¶¶Includes dentists, allied health professionals, technicians and technologists, emergency technicians, emergency medical technicians, and paramedics.
***Includes administrative support staff members and managers, and nonclinical support staff members.
†††Respondents could select more than one work setting. Each work setting is represented by a separate variable with two values (yes and no, where reference value is no).
§§§Nursing home, assisted living facility, other long-term care facility, home health agency, or home health care.
¶¶¶Includes dentist office or dental clinic, pharmacy, emergency medical services, and other settings where clinical care or related services were provided to patients.
****Rurality was defined using zip codes in which >50% of the population resides in a nonmetropolitan county, a rural U.S. Census Bureau tract, or both, according to the Health Resources and Services Administration's definition of rural population. https://www.hrsa.gov/rural-health/about-us/what-is-rural.
††††https://www2.census.gov/geo/pdfs/maps-data/maps/reference/us_regdiv.pdf.
§§§§Excludes those with employer updated COVID-19 vaccination requirement.
Employer requirements for receipt of influenza and updated 2023–24 COVID-19 vaccination were reported by 39.2% and 12.5% of HCP overall, respectively (Figure 3A). HCP working in LTC settings were less likely to report requirements for influenza vaccine (25.6%) compared with HCP working in ambulatory care settings (33.4%) and hospitals (62.1%). For the updated 2023–24 COVID-19 vaccine, HCP working in ambulatory care settings were less likely to report requirements for receipt of vaccine (10.2%) compared with HCP working in hospital (14.8%) or LTC (13.5%) settings.
Influenza vaccination coverage was highest among HCP who reported an employer requirement for influenza vaccination (97.5%) compared with those who reported an employer recommendation for vaccination without a requirement (74.1%) or no recommendation or requirement for vaccination (38.8%). Updated 2023–24 COVID-19 vaccination coverage was also higher among HCP who reported an employer requirement for updated COVID-19 vaccination (55.6%) than among those who reported an employer recommendation without a requirement (38.1%), or no recommendation or requirement (15.7%) (Figure 3B). Additionally, among HCP who were not required by their employer to be vaccinated, 74.2% were vaccinated for influenza and 40.8% were vaccinated with the updated 2023–24 COVID-19 vaccine when their employers offered these vaccines onsite at the workplace, compared with 45.5% and 23.3%, respectively, among those whose employers did not offer these vaccines onsite (Table 1 and 2).
Figure 3. Prevalence of employer requirement or recommendation for influenza and updated 2023-24 COVID-19 vaccination† (A) and vaccination coverage, by employer requirement status (B) among health care personnel, by work setting – Internet panel surveys§, United States, April 2024
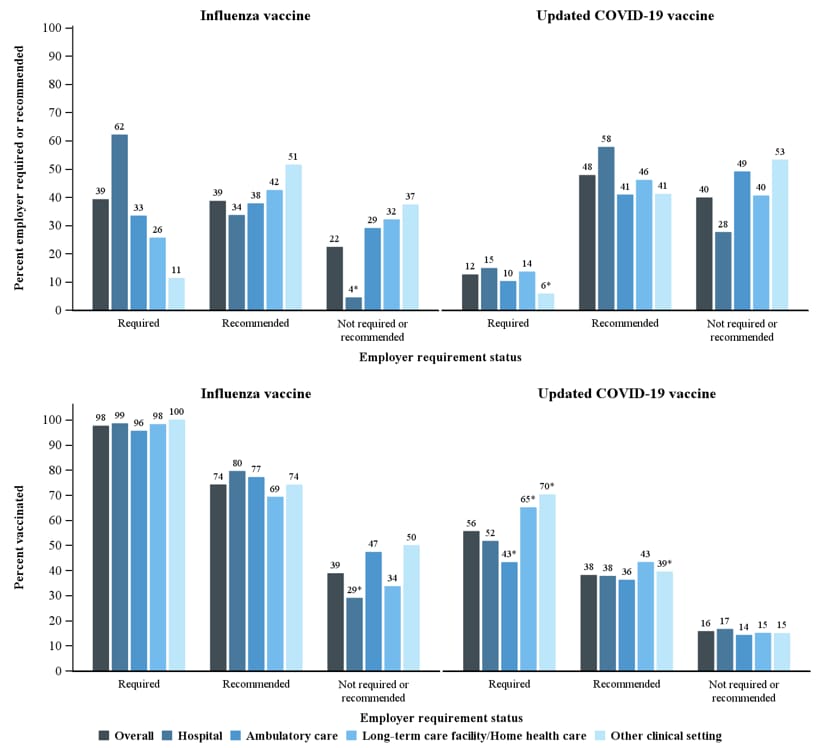
*Estimates do not meet the National Center for Health Statistics' standards of reliability and should be interpreted with caution.
†Respondents were considered to have received an updated 2023-24 COVID-19 vaccine if they responded "Yes" to the question, "An updated COVID-19 vaccine (2023-2024 formula) became available in September 2023. Have you received an updated 2023-24 COVID-19 vaccine?"
§Respondents were recruited from two preexisting national opt-in Internet sources: Medscape (https://www.medscape.com), a medical website managed by WebMD Health Professional Network, and general population Internet panels operated by Dynata (Dynata_Panel_Book.pdf).
When asked about their attitudes towards influenza and COVID-19 and influenza and COVID-19 vaccinations, most HCP agreed that they are at risk for getting influenza (71.3%) and COVID-19 (71.0%). The majority of the HCP surveyed also agreed that people around them were at risk of getting influenza (79.9%) and COVID-19 (79.3%). When asked if the influenza vaccination or COVID-19 vaccination can protect them from getting influenza or COVID-19, 78.4% agreed that influenza vaccination can protect them, whereas only 59.6% agreed that COVID-19 vaccinations can protect them from getting COVID-19. Furthermore, 84.6% of HCP agreed that the influenza vaccination was safe, compared with 63.3% of HCP who agreed that the COVID-19 vaccination was safe. When asked about requirements for vaccination, 58.8% agreed that HCP should be required to be vaccinated against influenza, but only 43.7% agreed that HCP should be required to be vaccinated against COVID-19 (Figure 4).
Figure 4. Attitudes toward influenza and COVID-19 and influenza and COVID-19 vaccinations* among health care personnel – Internet panel surveys†, United States 2024
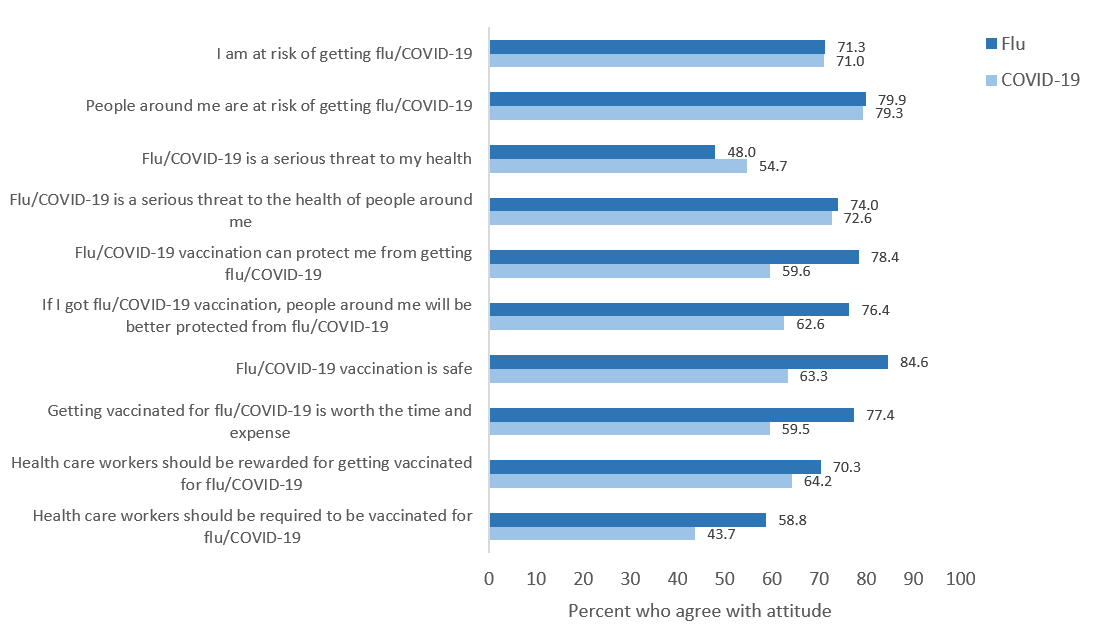
*Percent of health care personnel who agreed with each attitude statement among respondents. Weighted percentages are shown.
†Respondents were recruited from two preexisting national opt-in Internet sources: Medscape (https://www.medscape.com), a medical website managed by WebMD Health Professional Network, and general population Internet panels operated by Dynata (Dynata_Panel_Book.pdf).
Discussion
As observed during previous influenza seasons, nonclinical personnel, assistants and aides, HCP working in LTC and home health care settings, HCP with less than a college degree, and HCP who reported their employer neither required nor recommended the influenza vaccine had the lowest coverage with influenza and COVID-19 vaccines679. Similar patterns were observed for COVID-19 vaccination coverage, with the exception that HCP working in ambulatory care settings had the lowest coverage by work setting with updated 2023–2024 COVID-19 vaccine. Overall, more than two-thirds of HCP did not receive an updated 2023-24 COVID-19 vaccine and coverage remained suboptimal. Influenza vaccination coverage among HCP decreased in the 2020-2021 season following the COVID-19 pandemic, particularly in ambulatory and other clinical settings. Some HCP in these settings may have been working remotely or primarily conducting telehealth visits and not subject to onsite vaccination policies. After apparent recovery and return to pre-pandemic coverage rates during the 2021–2022 season, coverage decreased again during the 2022–2023 and 2023–2024 seasons for unknown reasons and was similar to the 2020–2021 season69. Continued monitoring will be necessary to understand if coverage will remain lower or will return to 80% or greater coverage as occurred in 2018-2020, and 2021-22. (Supplementary Table S1)
Employer vaccination requirements were strongly associated with influenza and COVID-19 vaccination uptake among HCP. Influenza vaccination coverage was approximately 60 percentage points higher among HCP with employer vaccination requirements, compared with HCP without employer vaccination requirements or recommendations. Comparatively, requirements for updated 2023–24 COVID-19 vaccine were infrequently reported in all work settings by HCP, even among hospitals, a large percentage of which had influenza vaccination requirements. Requirements for the updated 2023-24 COVID-19 vaccinations were also substantially lower than requirements for the primary COVID-19 vaccination series6. Approximately 60% of HCP reported requirements for COVID-19 vaccination in 2021–2022, but the prevalence of vaccination recommendations, requirements, and the offering COVID-19 vaccine onsite have declined. While the ACIP recommends that emphasis be placed on HCP for flu vaccination2, and the Community Guide recommends that employers offer free onsite flu vaccines for HCP4, no such specific recommendations are in place for COVID-19 vaccination aside from vaccination requirements, workplace vaccination policies and promotional events, such as offering vaccination onsite, requirements to sign a waiver or declination form if not vaccinated, and public identification of vaccinated individuals, may be effective in increasing vaccination coverage in many work settings1011. Useful resources that can help with increasing vaccination coverage among HCP include CDC's long-term care web-based toolkit which provides access to resources, strategies, and educational materials, and interventions recommended by the Community Preventive Services Task Force412.
HCP working in LTC and home health care settings and assistants and aides have historically had lower influenza vaccination coverage. This finding was consistent through the prior nine influenza seasons and during the 2023–2024 season. Prior studies have also found that HCP working in LTC settings report fewer influenza vaccination requirements and promotional activities47. This is especially concerning since patient populations in LTC and home health care settings tend to be more vulnerable and at high risk for severe influenza related illnesses13.
Measured attitudes towards influenza and COVID-19 and influenza and COVID-19 vaccinations showed that most HCP agree that they and those around them are at increased risk for getting influenza and COVID-19. Attitudes towards safety of an influenza vaccination and COVID-19 vaccination differed among HCP, with few HCP agreeing that the COVID-19 vaccination was safe. Even fewer HCP agreed that the COVID-19 vaccination could protect them from COVID-19 or that HCP should be required to be vaccinated against COVID-19. The safety and efficacy of COVID-19 vaccines are supported by clinical trials and other studies, which have shown that COVID-19 vaccines are effective against severe illness, hospitalization, and death; severe adverse reactions after COVID-19 vaccines are rare31415. Providing vaccination at the worksite during work hours, coupled with employer communication about the favorable benefit-risk balance of COVID-19 vaccination could increase COVID-19 vaccine coverage, as seen in prior studies on influenza vaccination coverage416. As waning immunity from prior COVID-19 vaccines have been observed17, it remains important that HCP stay up to date on all recommended COVID-19 vaccinations, including getting updated vaccines when indicated. Remaining up to date with all COVID-19 and influenza recommended vaccinations is important for all HCP to prevent severe illness in themselves and to reduce the risk of exposing their patients to vaccine-preventable diseases.
| Weighted % vaccinated (95% CI) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Characteristic | 2014-15 | 2015-16 | 2016-17 | 2017-18 | 2018-19 | 2019-20 | 2020-21 | 2021-22 | 2022-23 | 2023-24 |
| Total | 77.3 (74.6, 79.8) | 79.0 (76.6, 81.3) | 78.6 (76.0, 81.0) | 78.4 (76.0, 80.8) | 81.1 (78.6, 83.4) | 80.6 (78.2, 82.8) | 75.7 (70.7, 80.3) | 80.6 (77.4, 83.5) | 75.9 (73.1, 78.6) | 75.4 (72.4, 78.3) |
| Occupation¶ | ||||||||||
| Physician | 88.9 (84.5, 92.4) | 95.6 (92.0, 97.9) | 95.8 (92.5, 97.9) | 96.1 (92.2, 98.4) | 96.7 (93.5, 98.6) | 98.0 (95.3, 99.4) | 90.8 (83.7, 95.6) | 96.6 (94.4, 98.2) | 94.5 (90.1, 97.3) | 93.0 (88.5, 96.2) |
| Nurse practitioner/Physician assistant | 87.0 (80.9, 91.8) | 90.3 (84.0, 94.7) | 92.0 (86.0, 96.0) | 87.8 (79.7, 93.5) | 91.0 (82.0, 96.4) | 88.8 (80.9, 94.2) | 91.9 (83.5, 96.8) | 92.2 (88.6, 95.0) | 91.0 (86.2, 94.5) | 85.7 (79.9, 90.3) |
| Nurse | 89.0 (83.1, 93.4) | 90.1 (84.4, 94.3) | 92.6 (87.3, 96.2) | 90.5 (85.1, 94.5) | 91.8 (86.1, 95.7) | 92.0 (86.9, 95.5) | 90.8 (82.5, 96.0) | 86.8 (81.6, 90.9) | 88.1 (81.7, 92.9) | 87.6 (80.7, 92.7) |
| Pharmacist | 95.3 (88.1, 98.8) | 86.5 (74.8, 94.1) | 93.7 (90.2, 96.2) | 92.2 (87.9, 95.4) | 91.5 (86.9, 94.8) | 90.6 (86.4, 93.8) | 90.7 (86.9, 93.7) | 94.4 (92.0, 96.2) | 90.7 (86.8, 93.7) | 93.9 (90.5, 96.3) |
| Other clinical personnel** | 81.3 (76.7, 85.4) | 84.7 (80.7, 88.2) | 80.0 (75.6, 84.0) | 80.9 (75.3, 85.6) | 85.8 (81.0, 89.8) | 81.7 (76.6, 86.1) | 84.0 (77.4, 89.4) | 86.8 (83.0, 89.9) | 82.5 (77.3, 86.9) | 81.8 (76.9, 86.0) |
| Assistant/Aide | 64.4 (58.5, 69.9) | 64.1 (60.1, 67.9) | 69.1 (65.2, 72.9) | 71.1 (66.7, 75.2) | 72.5 (68.2, 76.5) | 72.4 (68.3, 76.1) | 64.0 (59.5, 68.4) | 69.1 (64.6, 73.3) | 62.8 (59.3, 66.1) | 63.2 (58.5, 67.7) |
| Non-clinical personnel†† | 75.2 (69.2, 80.5) | 77.7 (71.9, 82.8) | 73.7 (67.3, 79.5) | 72.8 (67.1, 77.9) | 75.5 (69.5, 80.8) | 76.7 (71.0, 81.8) | 67.0 (52.8, 79.3) | 78.6 (68.8, 86.6) | 70.6 (62.8, 77.6) | 69.5 (61.5, 76.8) |
| Work setting§§ | ||||||||||
| Hospital | 90.4 (86.6, 93.3) | 91.2 (88.1, 93.8) | 92.3 (89.0, 94.8) | 91.9 (88.4, 94.6) | 95.2 (92.7, 97.0) | 93.2 (89.9, 95.6) | 91.3 (87.7, 94.2) | 92.2 (89.4, 94.4) | 85.7 (81.3, 89.4) | 89.1 (84.8, 92.5) |
| Ambulatory care | 78.4 (74.2, 82.2) | 79.8 (74.9, 84.2) | 76.1 (71.2, 80.5) | 75.1 (69.8, 79.9) | 79.8 (74.8, 84.1) | 78.8 (74.1, 82.9) | 73.3 (59.1, 84.6) | 81.4 (76.9, 85.3) | 75.3 (70.9, 79.4) | 74.6 (69.8, 79.0) |
| Long-term care facility/Home health care¶¶ | 63.9 (58.0, 69.6) | 69.2 (64.6, 73.6) | 68.0 (62.2, 73.4) | 67.4 (62.5, 71.9) | 67.9 (62.5, 73.0) | 69.3 (64.1, 74.2) | 65.4 (58.9, 71.6) | 67.9 (59.6, 75.4) | 68.3 (61.4, 74.5) | 65.2 (58.0, 71.9) |
| Other clinical setting*** | 74.0 (65.2, 81.5) | 69.8 (61.3, 77.4) | 75.0 (68.3, 80.9) | 74.9 (67.8, 81.1) | 77.9 (70.2, 84.5) | 77.7 (71.1, 83.5) | 64.1 (54.0, 73.3) | 80.4 (73.0, 86.4) | 68.5 (61.3, 75.0) | 68.0 (59.2, 76.0) |
*Respondents were recruited from two preexisting national opt-in Internet sources: Medscape (https://www.medscape.com), a medical website managed by WebMD Health Professional Network, and general population Internet panels operated by Dynata (Dynata_Panel_Book.pdf)
†During 2020-21 influenza season, a weighting methodological change was implemented. Prior to 2020-21 influenza season, weights were calculated to population control totals controlling for the main effects (occupation, age group, race and ethnicity, sex, work setting, and Census region); 2020-21 influenza season and onward, interaction terms between occupation and the other main effects were added in the weighting model. Influenza Vaccination Coverage Among Health Care Personnel — United States, 2020–21 Influenza Season | FluVaxView | Seasonal Influenza (Flu) | CDC.
§Modified Clopper-Pearson 95% CI according to the approach of Korn and Graubard (https://www150.statcan.gc.ca/n1/en/pub/12-001-x/1998002/article/4356-eng.pdf?st = nQVSWv1i).
¶Excludes students.
**Includes dentists, allied health professionals, technicians and technologists, emergency technicians, emergency medical technicians, and paramedics.
††Includes administrative support staff members and managers, and non-clinical support staff members.
§§Respondents could select more than one work setting. Each work setting is represented by a separate variable with two values (yes and no, where reference value is no).
¶¶Nursing home, assisted living facility, other long-term care facility, home health agency, or home health care.
***Includes dentist office or dental clinic, pharmacy, emergency medical services, and other settings where clinical care or related services were provided to patients.
Limitations
The findings in this report are subject to at least five limitations. First, the study used a nonprobability sample of volunteer members of Medscape and Dynata Internet panels. Responses were weighted to be representative of the U.S. population of HCP; however, some bias might remain in the coverage estimates. Second, the self-selection of respondents to the panels and to the survey might introduce selection bias if the participation in the panel or survey is related to likelihood of being vaccinated. Third, vaccination status was self-reported and might be subject to recall or social desirability bias. Fourth, formal statistics that rely on the assumption of random sampling were used to determine differences in vaccination coverage between groups in this non-random sample and results should be interpreted with caution.I Finally, insufficient sample size resulted in the coverage estimates in some subgroups not meeting the National Center for Health Statistics reliability criteria for reporting proportions.
Authors
Mehreen Meghani, MPH1, Zhuping Garacci, MS2, Hilda Razzaghi, PhD1, Marie A. de Perio, MD3, Jeneita Bell, A. Scott Laney, PhD4, Carla L. Black, PhD1
Acknowledgments: Jeneita Bell, MD, MPH5
1Immunization Services Division, National Center for Immunization and Respiratory Diseases, CDC; 2Cherokee Nation Operational Solutions; 3Office of the Director, National Institute for Occupational Safety and Health, CDC; 4Division of Respiratory Health, National Institute for Occupational Safety and Health, CDC; Division of Healthcare Quality Promotion, National Center for Emerging and Zoonotic Infectious Diseases
- Physicians, nurse practitioners, physician assistants, nurses, dentists, pharmacists, allied health professionals, technicians, technologists, emergency medical technicians, paramedics, and students in a medical-related field were recruited from the current membership roster of Medscape. Additional information on Medscape is available at https://www.medscape.com.
- Assistants, aides, and non-clinical personnel (such as administrators, clerical support workers, janitors, food service workers, and housekeepers) were recruited from general population Internet panels operated by Dynata. Additional information on Dynata and its incentives for online survey participants is available at Dynata_Panel_Book.pdf .
- Population control totals of U.S. HCP by occupation and work setting were obtained from the U.S. Department of Commerce Bureau of Labor Statistics' occupational employment and wage statistics (https://www.bls.gov/oes/current/oessrci.htm). Population control totals by other demographic characteristics were obtained from the Bureau of Labor Statistics' labor force statistics from the current population survey. https://www.bls.gov/cps/data.htm
- Major occupational categories included physicians and dentists, nurse practitioners and physician assistants, nurses, pharmacists, other clinical personnel (including allied health professionals, technicians and technologists, and emergency medical technicians and paramedics), assistants and aides, and nonclinical personnel (including administrative support staff members and managers, and nonclinical support staff members).
- A survey response rate requires specification of the denominator at each stage of sampling. During recruitment of an online opt-in survey sample, such as the Internet panels described in this report, these numbers are not available; therefore, a response rate cannot be calculated. Instead, the survey completion rate is provided.
- Respondents were considered to have received an updated 2023-24 COVID-19 vaccine if they responded "Yes" to the question, "An updated COVID-19 vaccine (2023-2024 formula) became available in September 2023. Have you received an updated 2023-24 COVID-19 vaccine?"
- Questions included, "Since July 1, 2023, has your employer recommended or required that you be vaccinated for flu?" and "Has your employer recommended or required that you be vaccinated with the updated 2023-24 COVID-19 vaccine?" Responses for both questions included: recommend, require, neither, or unsure. Respondents could only select one option for each setting where they work.
- 4356-eng.pdf (statcan.gc.ca)
- NPS_TF_Report_Final_7_revised_FNL_6_22_13-2.pdf (aapor.org)
- Advisory Committee on Immunization Practices; CDC. Immunization of health-care personnel: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep 2011;60(No. RR-7):1–45. PMID:22108587
- Grohskopf LA, Ferdinands JM, Blanton LH, Broder KR, Loehr J. Prevention and Control of Seasonal Influenza with Vaccines: Recommendations of the Advisory Committee on Immunization Practices — United States, 2024–25 Influenza Season. MMWR Recomm Rep 2024;73(No. RR-5):1–25. DOI: http://dx.doi.org/10.15585/mmwr.rr7304a1
- CDC. Vaccines & immunizations: Interim Clinical Considerations for Use of COVID-19 Vaccines in the United States. Atlanta, GA: US Department of Health and Human Services, CDC; 2024. Accessed September 06,, 2024. www.cdc.gov/covid/hcp/vaccine-considerations/index.html
- Community Preventive Services Task Force. Worksite: seasonal influenza vaccinations using interventions with on-site, free, actively promoted vaccinations—healthcare workers. Atlanta, GA: US Department of Health and Human Services, CDC, Community Preventive Services Task Force; 2021. https://www.thecommunityguide.org/findings/worksite-seasonal-influenza-vaccinations-healthcare-on-site
- Folsom, Jr. RE, Singh AC. The generalized exponential model for sampling weight calibration for extreme values, nonresponse, and poststratification. Alexandria, VA: American Statistical Association; 2000. http://www.asasrms.org/Proceedings/papers/2000_099.pdf
- Razzaghi, H, Srivastav A, de Perio MA, Laney AS, Black CL. Influenza and COVID-19 Vaccination Coverage Among Health Care Personnel — United States, 2021-22. MMWR Morb Mortal Wkly Rep 2022; 71:1319-1326. DOI: http://dx.doi.org/10.15585/mmwr.mm7142a2
- Masalovich S, Razzaghi H, Duque J, et al. Influenza (flu): influenza vaccination coverage among health care personnel—United States, 2020–21 influenza season. Atlanta, GA: US Department of Health and Human Services, CDC; 2021. www.cdc.gov/fluvaxview/coverage-by-season/health-care-personnel-2020-2021.html
- Parker JD, Talih M, Malec DJ, et al. National Center for Health Statistics data presentation standards for proportions. Vital Health Stat 2 2017; 175:1–22. PMID:30248016
- Meghani M, Zhuping G, Razzaghi, H, et al. Influenza Vaccination Coverage Among Health Care Personnel — United States, 2022-2023 Influenza Season. Atlanta, GA: US Department of Health and Human Services, CDC; Influenza Vaccination Coverage Among Health Care Personnel — United States, 2022–23 Influenza Season | FluVaxView | Seasonal Influenza (Flu) | CDC
- Dey P, Halder S, Collins S, Benons L, Woodman C. Promoting uptake of influenza vaccination among healthcare workers: A randomized controlled trial. J Pub Health Med 2001;23: 346-348.
- Yue X, Black CL, Ball S, et al. Workplace interventions associated with influenza vaccination coverage among health care personnel in ambulatory care settings during the 2013-2014 and 2014-2015 influenza seasons. Am J Infection Control 2017;45:1243-1248.
- CDC. Post-acute and Long-term Care Facility Toolkit: Influenza Vaccination among Healthcare Personnel Atlanta, GA: US Department of Health and Human Services, CDC; 2020. Accessed September 6, 2022. Long-term-care-toolkit.pdf (cdc.gov)
- McMichael TM, Clark S, Pogosjans S, et al. COVID-19 in a long-term care facility — King County, Washington, February 27–March 9, 2020. MMWR Morb Mortal Wkly Rep 2020;69:339-342
- CDC. COVID-19 Vaccine Basics. Atlanta, GA: US Department of Health and Human Services, CDC; 2022. Accessed August 19, 2024. COVID-19 Vaccine Basics | COVID-19 | CDC
- Panagiotakopouos L, Moulia DL, Godfrey M, et al. Use of COVID-19 Vaccines for Persons Aged >=6 Months: Recommendations of the Advisory Committee on Immunization Practices— United States, 2024–2025. MMWR Morb Mortal Wkly Rep 2024;73:819-824. DOI: http://dx.doi.org/10.15585/mmwr.mm7337e2
- Black CL, Yue X, Ball SW, et al. Influenza Vaccination Coverage Among Health Care Personnel — United States, 2017—2018 Influenza Season. MMWR Morb Mortal Wkly Rep 2018;27:1050—1054. DOI: http://dx.doi.org/10.15585/mmwr.mm6738a2.
- Ferdinands JM, Rao S, Dixon BE, et al. Waning 2-Dose and 3-Dose Effectiveness of mRNA Vaccines Against COVID-19—Associated Emergency Department and Urgent Care Encounters and Hospitalizations Among Adults During Periods of Delta and Omicron Variant Predominance — VISION Network, 10 States, August 2021—January 2022. MMWR Morb Mortal Wkly Rep 2022;71:255-263. DOI: http://dx.doi.org/10.15585/mmwr.mm7107e2.
