Key points
- Cyclosporiasis is an intestinal infection that spreads when people ingest food or water contaminated with stool.
- Cyclosporiasis can be treated with an antibiotic regimen of trimethoprim-sulfamethoxazole (TMP-SMX).
- Because testing for Cyclospora is not routinely conducted in most US laboratories, healthcare providers may have to specifically request testing for it.
Overview
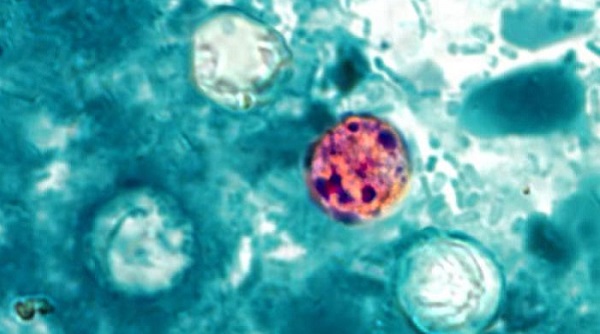
Cyclospora cayetanensis is a unicellular parasite that causes an intestinal infection called cyclosporiasis. Because Cyclospora is a coccidian parasite, infected people shed oocysts (rather than cysts or ova) in their feces.
Risk factors
Anyone can be at risk for infection, though people living or traveling in the tropics and subtropics may be at increased risk for infection because cyclosporiasis is endemic in some countries in these zones. In all regions where cyclosporiasis is endemic the infection appears to be seasonal, though seasonality varies in different settings and is not well understood.
Incubation
Some infected persons are asymptomatic, particularly in settings where cyclosporiasis is endemic. Among symptomatic persons, the incubation period averages one week (ranging as soon as 2 days – 2 weeks or more).
How it spreads
Cyclospora infection is transmitted by ingesting food or water that has been contaminated with Cyclospora oocysts. Foodborne outbreaks of cyclosporiasis in the United States have been linked to consumption of fresh produce.
Cyclospora cayetanensis completes its life cycle in humans. However, the oocysts shed in the feces of infected persons must mature (sporulate) outside the host, in the environment, to become infective for someone else. This process is thought to require at least 1 – 2 weeks in favorable environmental conditions. Therefore, direct person-to-person (fecal-oral) transmission of Cyclospora is unlikely.
Clinical features
Cyclospora infects the small intestine and typically causes watery diarrhea with frequent, sometimes explosive, bowel movements. Other common symptoms include
- Loss of appetite
- Weight loss
- Abdominal cramping/bloating
- Increased flatus
- Nausea
- Prolonged fatigue
Other symptoms can include
- Vomiting
- Body aches
- Low-grade fever
- Other flu-like symptoms
If untreated, the illness may last for a few days to a month or longer and may follow a remitting-relapsing course. Although cyclosporiasis usually is not life threatening, reported complications have included malabsorption, cholecystitis, and reactive arthritis.
Prevention
The best way for people to prevent infection is to avoid consuming food or water that may be contaminated with stool. Travelers to cyclosporiasis-endemic areas should be aware that although food and water precautions for Cyclospora are similar to precautions for other intestinal pathogens, Cyclospora is unlikely to be killed by routine chemical disinfection or sanitizing methods. Symptomatic reinfection can occur.
Testing and diagnosis
Healthcare providers should consider Cyclospora as a potential cause of prolonged diarrheal illness, particularly in patients with a history of recent travel to Cyclospora-endemic areas, such as tropical and subtropical regions.
Ova and parasite testing of stool for Cyclospora requires special stains or other laboratory procedures that are not routinely conducted in most U.S. laboratories.
Similarly, not all gastrointestinal polymerase chain reaction (PCR) panels include a target for Cyclospora. Therefore, when evaluating persons with symptoms consistent with cyclosporiasis, specifically request testing for this parasite. If indicated, stool specimens should also be checked for other microbes that can cause a similar illness.
Challenges in diagnosis
Diagnosis can be difficult in part because patients who are symptomatic might not shed enough oocysts in their stool to be readily detectable by laboratory examinations. Therefore, patients might need to submit several specimens collected on different days.
Laboratory testing
Laboratories should use sensitive recovery methods (concentration procedures) and detection methods that highlight Cyclospora oocysts. The oocysts can be stained with modified acid-fast or modified ("hot") safranin techniques. Cyclospora oocysts also are autofluorescent, meaning when stool containing the parasite is viewed under an ultraviolet (UV) fluorescence microscope the oocysts appear blue or green against a black background. Molecular diagnostic methods, such as polymerase chain reaction (PCR) analysis, are used to look for the parasite's DNA in the stool.
Another important point is that Cyclospora oocysts may be shed intermittently and at low levels, even by persons with profuse diarrhea. A single negative stool specimen does not exclude the diagnosis; several specimens collected on different days—that are processed and examined with sensitive methods—may be required.
Treatment and recovery
Trimethoprim-sulfamethoxazole (TMP-SMX), (sold as Bactrim,* Septra,* or Cotrim*) is the treatment of choice. The typical regimen for immunocompetent adults is:
- TMP 160 mg plus SMX 800 mg (one double-strength tablet), orally, twice a day, for 7 – 10 days. People living with HIV may need longer courses of therapy.
*Use of trade names is for identification only and does not imply endorsement by the Public Health Service or by the U.S. Department of Health and Human Services.
