At a glance
People throughout the United States face climate change-related health risks, but some of us will feel the effects earlier and more severely.
Overview
CDC has partnered with the American Public Health Association (APHA) to create a playbook. This comprehensive, step-by-step resource is designed to supplement the BRACE framework and support public health departments and adaptation planners as incorporate fairness into their climate and health efforts.
Fairness principles are crucial to climate change adaptation planning.
People throughout the United States face climate change-related health risks, but some of us will feel the effects earlier and more severely. This is because of differences in our exposures to climate hazards, our sensitivity to these hazards, and our ability to adapt.1
Groups at increased risk include but are not limited to:
- Pregnant women.
- People with preexisting or chronic medical conditions.
- Those with low income.
- Some rural communities.
- Some communities of color.
- Immigrant groups.
- Indigenous peoples.
- Children.
- Older adults.
- Outdoor workers.
- Persons with disabilities.
Characterizations of vulnerability should consider how these populations experience disproportionate, multiple, and complex risks to their health and well-being in response to climate change.
The three primary factors that influence climate vulnerability
Exposure
Contact between a person and one or more climate change-related hazards, such as heat waves, wildfires, or floods. For example, outdoor workers might face more frequent and longer exposure to extreme heat. Persons who live or work along the coast could be at risk from sea level rise, flooding, and storm surge.
Sensitivity
The degree to which people are negatively affected by climate hazards if exposed. For example, people with pre-existing medical conditions such as asthma are more likely to have poor outcomes when exposed to poor air quality associated with climate change. Because of their developing airways, children who breath in wildfire smoke are more likely to be affected than are adults.
Ability to adapt
A person's ability to adapt includes their ability to adjust to potential hazards, take advantage of opportunities, or respond to the consequences of climate hazards. This is often directly related to the material or social resources a person or community might draw upon to avoid or lessen risk. For example, older adults might have difficulty walking or lack transportation. This could make it hard for them to get to cooling centers.
Relationship between the factors that affect climate vulnerability and health outcomes
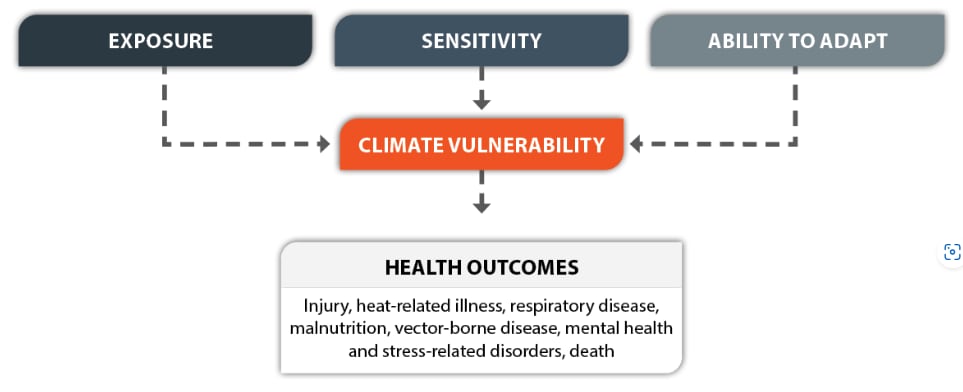
At the individual, community, and national levels, these aspects of vulnerability affect all people to some degree. However, past and present economic, social, and environmental factors in our society affect all three of these drivers and lead to some groups having more vulnerability than others.
Drivers of climate vulnerability rarely occur alone. For example, extremely hot days can lead to heat-related illnesses such as heat exhaustion or heat stroke. Heat can also increase air pollution levels and health problems related to poor air quality, such as respiratory issues, heart disease, and lung disease. People living in some neighborhoods are more likely to experience adverse effects of extreme heat and air pollution than those living in other parts of the same city.
Climate justice recognizes:
Climate-related risks are not distributed equally.
Obstacles may affect those living in rural communities,2 women, and older adults, for example.
Climate change will worsen existing disparities in social conditions and health.
Climate change will worsen existing disparities in social conditions and health. Social determinants of health are conditions in the places where people live, learn, work, and play that affect a wide range of health risks and outcomes. Climate change is expected to greatly affect those conditions and to intensify inequities. For example, people with limited income are more likely to live in subsidized housing, which is more likely to be in an area that floods.3 Their housing options also might have mold problems and inadequate insulation and air conditioning to effectively cope with severe heat or strong storms. People with lower incomes also might be unable to afford flood or fire insurance, rebuild damaged homes, or pay high medical bills after catastrophe strikes, fueling a continuous cycle of increasing vulnerability for those who are already disadvantaged.
Harms associated with climate change are burdening groups that have contributed the least to cause it.
Just 20 countries produce more than 80% of greenhouse gas emissions. Most of that (about 25%) has been from the United States.4 People living in countries that emit less greenhouse gasses are facing serious harm to their health and well-being from gases released by those 20 countries. This disparity in responsibility and harm is also seen between different communities within the United States.5 This is expected to increase in the future with additional climate change, further impacting those who are disproportionately affected.6
Fairness and building resilience against climate effects
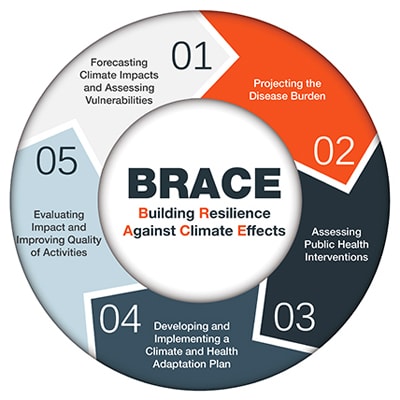
The Building Resilience Against Climate Effects (BRACE) framework is a five-step process that allows health officials to develop strategies and programs to help communities prepare for the health effects of climate change.
CDC partnered with the American Public Health Association (APHA) to create a playbook - a comprehensive, yet practical, step-by-step supplement to BRACE. This is a critical step to identifying and engaging populations most affected by climate change.
Working with health departments
Health departments are uniquely positioned to identify populations and communities that are experiencing greater climate vulnerability. Health departments have access to health and environmental data, partnerships with other governmental and nongovernmental organizations, and legal powers to protect and promote public health. CDC's Climate Ready Communities Initiative funds 13 jurisdictions to use the five-step Building Resilience Against Climate Effects (BRACE) framework to identify likely climate effects in their communities, potential health effects associated with these effects, and their most disproportionately affected populations and locations.
- https://health2016.globalchange.gov/climate-change-and-human-health
- https://www.cdc.gov/healthequity/core/index.html
- https://furmancenter.org/research/publication/housing-in-the-us-floodplains
- https://www.ucsusa.org/resources/each-countrys-share-co2-emissions
- https://www.sciencedirect.com/science/article/pii/S2214629621004552?via%3Dihub
- https://www.sciencedirect.com/science/article/abs/pii/S0140673619325966?via%3Dihub
