What to know
Though malaria was successfully eliminated in the United States, the parasitic disease still kills more than 400,000 people each year globally. In addition, parasitic and tropical diseases continue to cause illness within the United States. To protect people at home, CDC uses AMD technologies to help to identify and track antibiotic-resistant malaria internationally.

Addressing malaria in three sectors
Malaria is caused by Plasmodium, a parasite hitching a ride in the gut of a mosquito. When the mosquito feeds, Plasmodium enters the person's bloodstream through the mosquito's bite.
About 3.3 billion people—nearly half the world's population—live in areas where they are at risk of malaria. The United States is not immune. Each year about 1,700 travelers return to the U.S. from foreign travel with what is referred to as imported malaria.
While effective, current methods for fighting malaria, including insecticides, drugs, and improved diagnostic tests, have not fully succeeded in eliminating the disease. CDC is using AMD technologies to address malaria in three main sectors: insecticide resistance in mosquitoes, drug resistance in parasites, and testing.
Insecticide-resistant mosquitoes
In 1940, United States began to use powerful chemical pesticides to get rid of mosquitos. This intense mosquito-control initiative successfully eradicated malaria from the United States by the early 1950s. Ridding the world of mosquitoes is critical to malaria prevention.
However, decades of unmanaged insecticide use and routine exposure to chemicals have left many populations of mosquitoes resistant to multiple insecticides. The resistance includes pyrethroids, which are the most cost-effective public health insecticides currently available.
CDC is using AMD methods to identify DNA markers of pyrethroid resistance in the Anopheles albimanus mosquito. That particular mosquito is a prolific malaria vector in the Americas.
Using this information in that mosquito, for example, we can address it appropriately in several ways. That can include selecting the appropriate insecticides, ensuring maximum mosquito control, and implementing strategies to decrease insecticide resistance.

Drug-resistant parasites
About 1,700 people return to the United States infected with malaria contracted during foreign travel, so we continue to detect U.S. cases. In some cases, the Plasmodium parasites causing the disease are resistant to typical treatments.
Since the 1960s, Plasmodium parasites have continually evolved to resist antimalarial drugs, which makes malaria difficult to control. AMD methods can quickly help identify and track genetic markers of resistance.
CDC uses this technology to build an integrated surveillance system to identify and track drug-resistant Plasmodium. Early identification of resistant parasites will help guide accurate treatment and prophylaxis of malaria, limiting the spread of resistant parasites.

Testing challenges
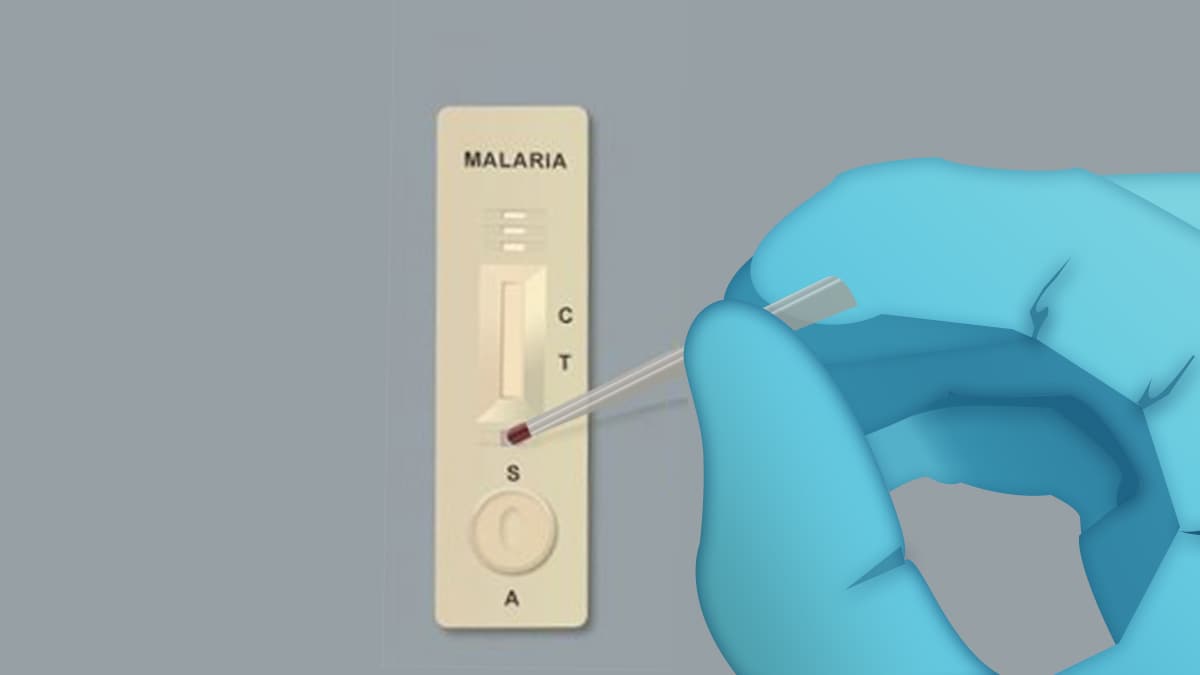
Rapid diagnostic tests are a critical tool for controlling malaria. The tests diagnose malaria in 15–20 minutes and do not require special training. Those factors make the tests perfect for malaria testing in remote communities with few medical workers.
According to the World Health Organization, the African region has increased its testing rates by 71% thanks to the availability of rapid tests. However, global public health partners have found the malaria parasites are mutating in a way that makes the tests less reliable.
To find out how the parasites are changing, CDC scientists are using AMD technologies to investigate the mutations. Then they use that information to work to develop tests to keep pace with changing malaria parasites.
Patenting a comprehensive parasitic diagnostic test
Diseases caused by parasites are notoriously difficult to identify. Even when scientists can acquire data, parasitic genomes are so large that they require specialized computer programs to decipher. However, using AMD technologies, CDC scientists developed and patented a laboratory method with the potential to revolutionize parasitic diagnostics.
The Universal Parasite Diagnostic assay, or UPDx, selectively detects all parasite DNA in a clinical blood sample without interference from human DNA. The test makes it easier to identify not just which parasite caused the illness but also genetic information about the parasite. CDC patented the process so it can be shared openly with other researchers at no charge to help advance research into other pathogens and diseases.
Accurately identifying neglected tropical diseases
The parasitic disease leishmaniasis is endemic in more than 90 countries in the tropics, subtropics, and southern Europe. People are infected with Leishmania parasites through sand fly bites. More than 20 different species of these parasites exist globally, and each species can cause different clinical forms of leishmaniasis.
There are two common forms of leishmaniasis. The first is cutaneous leishmaniasis, which causes skin sores. The second is visceral leishmaniasis, which affects several internal organs (usually spleen, liver, and bone marrow) and can be life-threatening.
Treatment of leishmaniasis depends in part on accurate identification of the Leishmania species causing a person's illness. However, current laboratory methods can be time-consuming, which can delay treatment decisions. Also, the current methods are not always successful in identifying some of the Leishmania species.
CDC scientists are using AMD techniques to develop molecular-based laboratory methods to improve Leishmania species identification and diagnosis. With rapid, accurate lab results, it's easier to provide timely clinical management of leishmaniasis and improve the patient outcomes.
Detecting and controlling polio outbreaks
One of CDC's earliest missions was to control and eliminate polio in the United States. Through concerted surveillance and vaccination efforts, polio in the United States was eradicated by 1979. Now we are on the verge of eradicating the disease worldwide.
But the poliovirus evolves 10 million times faster than bacteria. It is reemerging in many parts of the world, confounding efforts to stop its spread. CDC's labs provide critical diagnostic services and genomic sequencing of polioviruses to help guide disease control efforts in many countries. The older, slower sequencing technologies take more than a week to confirm an isolate as poliovirus.
In 2014, CDC began applying AMD methods to increase the ability to detect and confirm new polio infections. These technologies reduced the time for poliovirus strain identification from a week to just a few hours. CDC is sharing these laboratory procedures with the hope of helping other countries.
With these technologies, it's possible to rapidly detect wild poliovirus and understand its pathway, thus speeding up the response to importations or spread of virus. The understanding of the viral pathway also helps public health officials focus their efforts to prevent further spread.
