Vaccination Coverage Among Adults in the United States, National Health Interview Survey, 2016
Key Findings
- Compared with 2015 NHIS estimates, modest increases in vaccination coverage occurred for some vaccines and age groups but coverage decreased for one vaccine overall and in two age groups in one racial/ethnic category. Apart from these changes, vaccination coverage among adults in 2016 was similar to estimates from 2015.
- Overall influenza vaccination decreased 3.1 percentage points to 70.4% among adults ≥65 years, and decreased among whites in all age groups except among adults 19-49 years (range: minus 2.2 – minus 3.5 percentage points).
- Pneumococcal vaccination increased 3.3 percentage points to 66.9% among adults ≥ 65 years.
- Vaccination of adults 19 years and older with tetanus toxoid, reduced diphtheria toxoid, and acellular pertussis vaccine (Tdap) increased by 3.4 percentage points to 26.6% overall.
- Hepatitis A vaccination increased by 14.8 percentage points to 23.7% among adults 19-49 years with chronic liver conditions.
- Herpes Zoster (Shingles) vaccination increased 2.8 percentage points to 33.4% among adults 60 years and older and increased 3.1 percentage points to 37.4% among adults 65 years and older.
- HPV vaccination (at least one dose) among females and males 19-26 years who had not received HPV vaccination prior to 19 years was 8.6% and 2.7%, respectively.
- Coverage did not change for other vaccinations in other age groups and many adults remained unvaccinated with recommended vaccines.
- Racial and ethnic vaccination differences persisted for all vaccinations in this report with generally lower coverage for most vaccinations among non-Hispanic black, Hispanic, and non-Hispanic Asian adults compared with white adults. Vaccination differences widened for Tdap (blacks, all age groups) and herpes zoster (Asians, ≥65 years) (due primarily to increases among whites).
Conclusions/Recommendations:
- Many adults in the United States have not received recommended vaccinations and racial/ethnic vaccination differences persist.
- Influenza vaccination decreased among whites and overall among adults ≥65 years.
- While modest gains occurred in vaccination coverage for pneumococcal, Tdap, hepatitis A (persons with chronic liver conditions), herpes zoster, and HPV vaccination, coverage did not improve for other vaccinations and many adults remained unvaccinated with recommended vaccines.
- Among adults 65 years and older:
- Over one-third did not report pneumococcal or Td vaccination.
- Approximately 4 out of 5 did not report Tdap vaccination.
- Nearly two-thirds did not report a herpes zoster vaccination.
- Among adults younger than 65 years with indications for pneumococcal vaccination, approximately 3 out of 4 did not report ever having been vaccinated.
- Among adults 19-26 years recommended for HPV catch-up vaccination:
- About 11 out of 12 females and 32 out of 33 males not vaccinated before 19 years did not report HPV vaccination (at least one dose).
- Among adults 65 years and older:
- The recommendation of a health care provider can ensure vaccination.
- Following the Standards for Adult Immunization Practice, all providers should routinely assess adults’ vaccination status at every clinical encounter, strongly recommend needed vaccines, and either offer needed vaccines or refer their patients to another provider who can administer the recommended vaccine, and document the vaccines administered in their state’s immunization information system (IIS).
- Vaccination providers should ensure reporting of vaccinations to their state’s IIS to support consolidation of adult patients’ vaccination records (1, 2). Using their state’s IIS can help providers access their patients’ immunization records and improve the ability to routinely and accurately assess their patients’ vaccination status.
Introduction
Adults are at risk of illness, hospitalization, disability, and, in some cases, death from vaccine-preventable diseases, particularly influenza (flu) and pneumococcal disease. CDC recommends vaccinations for adults based on age, health conditions, prior vaccinations, and other factors (3) to prevent vaccine-preventable diseases and related outcomes. Many adults are not fully vaccinated, leaving them vulnerable to preventable infectious diseases.
This report summarizes data on vaccination coverage for U.S. adults 19 years and older from the 2016 National Health Interview Survey (NHIS) (4). The NHIS is an in-person survey of eligible civilian non-institutionalized adults. Information on receipt of vaccinations, health and health care is self-reported and not verified through review of medical records or other means (5).
Who Was Vaccinated?
Influenza Vaccination
- Influenza vaccination coverage for the 2015-16 season overall among adults ≥19 years was 43.5%, similar to the estimate for the 2014-15 season.
- Compared with the 2014-15 season, influenza vaccination coverage decreased among whites ≥19 years (2.2 percentage points to 46.3%), 50-64 years (3.5 percentage points to 46.7%), and ≥65 years (3.1 percentage points to 72.0%).
- Influenza vaccination coverage among adults ≥65 years overall decreased by 3.1 percentage points to 70.4% for the 2015–16 season compared with the 2014–15 season estimate.
- In the 2015-16 season, coverage among whites ≥19 years (46.3%) was higher than that for blacks (39.5%) and Hispanics (33.1%).
Pneumococcal Vaccination
- Pneumococcal vaccination coverage among adults 19-64 years at increased risk for pneumococcal disease was 24.0% in 2016, similar to the estimate for 2015.
- Coverage among whites 19-64 years at increased risk was higher (24.5%) compared with Asians (16.2%), but did not differ for other racial/ethnic groups.
- Pneumococcal vaccination coverage among adults ≥65 years was 66.9% in 2016, a 3.3 percentage point increase compared with 2015.
- Coverage among whites ≥65 years (71.0%) was higher compared with blacks (55.5%), Hispanics (48.6%), and Asians (52.6%).
Tetanus Vaccination
- In 2016, the proportion of adults reporting having received any tetanus toxoid-containing vaccination during the past 10 years was 62.2% for adults ≥19 years, 62.8% for adults 19-49 years, 64.2% for adults 50-64 years, and 58.0% for adults ≥65 years, all similar to estimates for 2015.
- Whites had higher coverage across all age groups compared with blacks, Hispanics, and Asians.
- Among adults for whom Tdap vaccination could be assessed, coverage in the past ten years was 26.6% among adults ≥19 years (a 3.4 percentage point increase compared with 2015), 28.0% among adults 19-64 years (a 3.3 percentage point increase compared with 2015), and 20.4% among adults ≥65 years (a 3.9 percentage point increase compared with 2015).
- Whites had higher Tdap coverage across all age groups compared with blacks, Hispanics, and Asians and these vaccination differences increased for blacks only compared with differences measured in 2015.
Hepatitis A Vaccination
- In 2016, reported hepatitis A vaccination coverage (≥2 doses) was 9.5 % for adults ≥19 years, 13.4% for adults 19-49 years, and 5.4% for adults ≥50 years, similar to the estimates for 2015.
- Among adults 19-49 years, coverage for blacks (10.2%) was lower than that for whites (14.0%).
- Vaccination coverage was higher among adults who had traveled outside the United States to a country in which hepatitis A is of high or intermediate endemicity than among respondents who did not travel outside the United States or had traveled only to countries in which the disease is of low endemicity.
- Hepatitis A vaccination coverage among adults 19-49 years with chronic liver conditions was 23.7%, a 14.8 percentage point increase compared with the 2015 estimate.
Hepatitis B Vaccination
- In 2016, reported hepatitis B vaccination coverage (≥3 doses) was 24.8 % for adults ≥19 years, 32.9% for adults 19-49 years, and 15.9% for adults ≥50 years, similar to the estimates for 2015.
- Among adults 19-49 years, coverage for blacks (27.0%) and Hispanics (25.8%) was lower than that for whites (36.2%).
- Vaccination coverage was higher among adults who had traveled outside the United States to a country in which hepatitis B is of high or intermediate endemicity than among respondents who did not travel outside the United States or had traveled only to countries in which the disease is of low endemicity.
Herpes Zoster Vaccination
- Among adults ≥60 years, 33.4% reported receiving herpes zoster vaccination, a 2.8 percentage point increase from 2015. Whites ≥60 years had higher herpes zoster vaccination coverage (37.7%) compared with blacks (15.7%), Hispanics (21.4%), and Asians (21.9%) and these vaccination differences increased compared with 2015 estimates.
- Among adults 60-64 years, 23.9% reported herpes zoster vaccination, similar to the estimate for 2015. Whites 60-64 years had higher herpes vaccination coverage (27.2%) compared with blacks (8.9%).
- Among adults ≥65 years, 37.4% reported herpes zoster vaccination, a 3.1 percentage point increase from 2015. Whites ≥65 years had higher herpes zoster vaccination coverage (41.7%) compared with blacks (19.6%), Hispanics (22.1%), and Asians (23.3%) and these vaccination differences increased for Asians only compared with differences measured in 2015.
Human Papillomavirus Vaccination
- In 2016, among females 19-26 years, 48.5% reported receipt of at least one dose of HPV vaccine, a 6.9 percentage point increase compared with the estimate reported for 2015. Blacks (41.5%) had lower coverage compared with whites (52.2%) and this vaccination difference increased compared with the difference measured in 2015.
- Among females 19-21 years, HPV vaccination coverage was 51.6%, a 9.6 percentage point increase compared with the estimate for 2015.
- Among females 22-26 years, HPV vaccination coverage was 46.6%, similar to the 2015 estimate.
- Among males 19-26 years and 19-21 years, HPV vaccination coverage (at least one doses) was 13.5% and 21.2%, increases of 3.4 and 5.5 percentage points, respectively.
- HPV vaccination (at least one dose) among females and males 19-26 years who had not received HPV vaccination prior to 19 years was 8.6% and 2.7%, similar to estimates for 2015.
Trends in Adult Vaccination Coverage, 2010-2016
- Overall during 2010 through 2016, although point estimates for each year generally varied by only a few percentage points, linear trend tests indicated that vaccination coverage generally increased for all vaccines in this report, except for tetanus vaccination (Td or Tdap) among adults ≥19 years.
- Influenza vaccination, >19 years—range: 37.2%–44.8%.
- Pneumococcal vaccination, 19-64 years at increased risk—range: 18.5%–24.0%.
- Pneumococcal vaccination, >65 years—range: 59.7%–66.9%.
- Tdap vaccination, 19-64 years—range: 8.2%–28.0%.
- Tdap vaccination, >65 years (2012-2016)—range: 8.0%–20.4%.
- Hepatitis A vaccination, >19 years—range: 8.1%–9.5%.
- Hepatitis B vaccination, >19 years—range: 24.5%–27.1%.
- Herpes zoster vaccination, >60 years—range: 14.4%–33.4%.
- HPV vaccination, females 19-26 years—range: 20.7%–48.5%.
- HPV vaccination, males 19-26 years (2011-2016)—range: 2.1%–13.5%.
- During the 2009-10 through the 2015-16 influenza seasons, fewer than half of adults ≥19 years were vaccinated (range: 37.2%–44.8%).
FIGURE. Estimated proportion of adults ≥19 years who received selected vaccines, by age group and increased risk status— National Health Interview Survey, United States, 2010–2016. See data file [1 sheet].
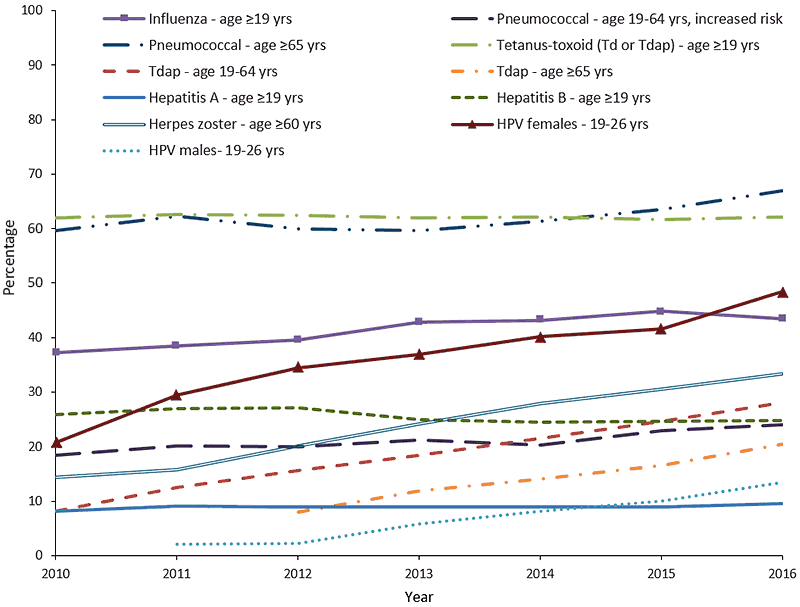
Abbreviations: HPV = human papillomavirus; Td = tetanus and diphtheria toxoids; Tdap = tetanus toxoid, reduced diphtheria toxoid, and acellular pertussis vaccine. See additional trend figures for select vaccines [4 sheets].
Additional Vaccination Coverage Information
- Vaccination coverage for selected vaccinations was estimated for adults ≥19 years who were healthcare personnel and proportions were estimated of adults ≥19 years by type of tetanus vaccine received, age at first dose of HPV vaccine, and racial/ethnic vaccination differences (See: Box 1).
- Estimates of proportions vaccinated were stratified by age group, health insurance status, having a usual place for health care, number of physician contacts, nativity, number of years living in the United States, and citizenship (See: Box 2).
What Can Be Done? (Recommendations)
In 2016, adult vaccination coverage in the United States remained similar to 2015, except for modest increases in pneumococcal (adults ≥65 years), Tdap (adults ≥19 years), hepatitis A (adults 19-49 years with chronic liver conditions), herpes zoster (adults ≥60 years and adults ≥65 years), and HPV (females 19-21 and 19-26 years; males 19-21 years and 19-26 years) vaccination. Influenza vaccination decreased among adults ≥65 years overall and among whites in all age groups except adults 19-49 years. Many adults in the United States have not received recommended vaccinations and racial and ethnic vaccination differences persisted for all seven vaccines in this report, widening for pneumococcal (≥65 years, blacks, Hispanics, and Asians compared with whites), Tdap (all age groups, blacks, Hispanics, and Asians compared with whites), herpes zoster (≥60 years and ≥65 years, blacks, Hispanics, and Asians compared with whites), and HPV (females 19-26 years, blacks compared with whites). Incorporating routine assessment of adult vaccination needs, recommendation, and offer of needed vaccinations into routine clinical care of adults can help improve vaccination rates and narrow racial and ethnic differences in vaccination coverage (1, 2, 5, 6).
To improve vaccination coverage, providers and provider organizations are encouraged to increase awareness and use of tools for implementing the Standards for Adult Immunization Practice. In addition, CDC encourages healthcare providers to consider immunization quality improvement projects that may result in measurable increases in adult immunization rates. Nationwide adoption of electronic health records, electronic patient portals, and patient-directed clinical decision support offer opportunities for improving adult vaccination rates (5). Some states are implementing innovative strategies to enhance vaccine access. For example, the Oregon Immunization Program has established a “mini-grant project” where annual funding announcements are issued and any group interested in providing or promoting immunizations can apply. This may include local health departments, clinics, or coalitions who are working with underserved populations within their own communities. The Massachusetts Department of Public Health has partnered with Center for Health Care Financing (CHCF) to implement a vaccination billing service for local health departments to ensure that the local health agencies are able to receive reimbursement for vaccines administered to patients with various health insurance plans, including Medicaid, Medicare part B and private health insurance plans. The Massachusetts Department of Public Health has also developed a strategy to help local health departments and other community health centers reach and vaccinate uninsured and disparate populations, which is highlighted in their guide to reaching and engaging diverse communities [61 pages].
Data Source and Methods
NHIS collects information about the health and health care of the noninstitutionalized U.S. civilian population using nationally representative samples. Face-to-face interviews are conducted by the U.S. Census Bureau for CDC’s National Center for Health Statistics. Non-institutionalized adults 19 years and older with interviews conducted during August 2015-June 2016 (for influenza vaccination) and January–December 2016 (for pneumococcal, Td, Tdap, hepatitis A, hepatitis B, herpes zoster, and HPV vaccination) were included in this analysis. The total adult sample was 32,626 persons ≥19 years. The final sample adult component response rate for the 2016 NHIS was 54.3%. The final sample adult response rates for estimating influenza vaccination coverage for the 2015-16 influenza season were 55.2% for 2015 and 54.3% for 2016. NHIS methods have been previously published. Questions about receipt of vaccinations recommended for adults are asked of one randomly selected adult within each family in the household and have been described previously (5). Weighted data were used to produce national vaccination coverage estimates. For non-influenza adult vaccination coverage estimates, the weighted proportion of respondents who reported receiving selected vaccinations was calculated. To better assess influenza vaccination coverage for the 2015-16 season, the Kaplan-Meier survival analysis procedure was used. Point estimates and 95% confidence intervals (CIs) were calculated by using statistical software to account for the complex sample design. T tests were used for comparisons between 2016 and 2015 and, for comparisons of each level of each characteristic (e.g., race/ethnicity), to a chosen referent level (e.g., for race/ethnicity, non-Hispanic white was the reference group). Statistical significance was defined as p<0.05. Coverage estimates are not reported for small sample size (n<30) or relative standard error (standard error/estimates) >0.3. Influenza vaccination coverage estimates from NHIS (≥19 years) reported here differ by 1.8% from previously reported estimates from BRFSS (Behavioral Risk Factor Surveillance System) (≥18 years); however, vaccination trends were similar during the 2009-2010 through the 2015-2016 seasons; racial/ethnic vaccination differences were similar.
Limitations
- All data rely on self-report and were not validated with medical records. However, adult self-reported vaccination status has been shown to be ≥70% sensitive in one or more studies for pneumococcal, tetanus toxoid-containing, herpes zoster, and hepatitis B vaccines and ≥70% specific in one or more studies for all except tetanus and hepatitis B vaccination (7, 8, 9, 10).
- Adults particularly might not be able to recall accurately vaccines received as infants or adolescents and hepatitis B vaccination coverage levels might be greatly underestimated. Additional study is needed for accuracy of recall by young adults of vaccinations they may have been received as children or adolescents. The findings for hepatitis B vaccination among younger adults 19-29 years should be viewed with caution, based on comparison with estimates based on provider-reported vaccinations from the NIS (National Immunization Survey)-Teen (11).
- The response rate was 54.3%. Nonresponse bias can result if respondents and nonrespondents differ in their vaccination rates, and if survey weighting does not fully correct for this.
- The NHIS excluded persons in the military and those residing in institutions, which might result in underestimation or overestimation of vaccination coverage levels.
- The Tdap vaccination estimate is subject to considerable uncertainty. Respondents who reported a tetanus vaccination but were unable to say whether Td or Tdap was used during 2005–2016 were excluded (38.7%) from estimations of Tdap coverage, creating a potential for bias.
- Due to small sample size, the increase in hepatitis A vaccination coverage among persons 19-49 years with chronic liver disease could be spurious.
- NHIS survey data methods and limitations.
Authors: Mei-Chuan Hung, MPH, PhD 1,2, Walter W. Williams, MD, MPH1, Peng-Jun Lu, MD, PhD 1, David K. Kim, MD 1, Lisa A. Grohskopf, MD 3, Tamara Pilishvili, MPH 4, Tami H. Skoff 4, MS, Noele P. Nelson, MD, PhD 5, Rafael Harpaz, MD 6, Lauri E. Markowitz, MD 6, Alfonso Rodriguez-Lainz, PhD, DVM 7, and Amy Parker Fiebelkorn, MSN, MPH 1
1Immunization Services Division, National Center for Immunization and Respiratory Diseases, CDC
2Leidos, Inc, Atlanta, GA
3Influenza Division, National Center for Immunization and Respiratory Diseases, CDC
4Division of Bacterial Diseases, National Center for Immunization and Respiratory Diseases, CDC
5Division of Viral Hepatitis, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, CDC
6Division of Viral Diseases, National Center for Immunization and Respiratory Diseases, CDC
7Division of Global Migration and Quarantine, National Center for Emerging and Zoonotic Infectious Diseases, CDC
References:
- National Vaccine Advisory Committee. Recommendations from the National Vaccine Advisory Committee: standards for adult immunization practice. Public Health Rep 2014;129:115–23.
- CDC. Standards for Adult Immunization Practice.
- CDC. Vaccine information for adults.
- National Health Interview Survey public use data file.
- Williams WW, Lu P-J, O’Halloran AO, et al. Surveillance of vaccination coverage among adult populations – United States, 2015. MMWR Surveill Summ 2017;66(No. SS-11):1-28.
- Community Preventive Services Task Force. The guide to community preventive services. Increasing appropriate vaccination: universally recommended vaccinations. Atlanta, GA: US Department of Health and Human Services, CDC; 2011.
- Rolnick SJ, Parker ED, Nordin JD, Hedblom BD, Wei F, Kerby T, et al. Self-report compared to electronic medical record across eight adult vaccines: do results vary by demographic factors? Vaccine 2013;31(37):3928-3935.
- Mangtani P, Shah A, Roberts JA. Validation of influenza and pneumococcal vaccine status in adults based on self-report. Epidemiol Infect 2007;135(1):139-143.
- Donald RM, Baken L, Nelson A, Nichol KL. Validation of self-report of influenza and pneumococcal vaccination status in elderly outpatients. Am J Prev Med 1999;16:173-7.
- Zimmerman RK, Raymund M, Janosky JE, et al. Sensitivity and specificity of patient self-report of influenza and pneumococcal polysaccharide vaccinations among elderly outpatients in diverse patient care strata. Vaccine 2003;21:1486-91.
- Walker TY, Elam-Evans LD, Singleton JA, et al. National, Regional, State, and Selected Local Area Vaccination Coverage Among Adolescents Aged 13–17 Years — United States, 2016. MMWR Morb Mortal Wkly Rep 2017;66:874–882. DOI
| Table | URL (hyperlinked) | Result summary |
|---|---|---|
| Proportion of Health Care Personnel Who Received Selected Vaccinations | Box 1/ Table 1 [1 sheet] Table 1 HCP |
Overall, influenza, tetanus toxoid, reduced diphtheria toxoid and acellular pertussis vaccine (Tdap), and hepatitis B vaccination coverage for 2016 was similar to 2015 estimates among HCP ≥19 years. White HCP had higher vaccination coverage compared with black HCP or Hispanic HCP. |
| Proportion of Health Care Personnel with Direct Patient Care Who Received Selected Vaccinations | Box 1/ Table 2 [1 sheet] Table 2 HCP Direct Contact |
Overall, influenza and Tdap vaccination coverage for 2016 was similar to 2015 estimates among HCP ≥19 years with and without direct patient care. In 2016, among HCP ≥19 years with direct patient care, hepatitis B vaccination coverage decreased 4.6 percentage points to 69.5% compared with the estimate for 2015. Tdap and hepatitis B vaccination coverage was higher among HCP with direct patient care compared with those without direct patient care. |
| Proportion of Adults Who Received Tdap Among Those Reporting Tetanus Vaccination | Box 1/ Table 3 [1 sheet] Table 3 Tdap type |
Among adults ≥19 years, 41.5% reported they knew what type of tetanus vaccine they received, 44.6% reported they were not informed of the vaccination type, and 13.9% could not recall the type of tetanus vaccination received. Among those who reported they knew what type tetanus vaccine they received, 73.2% reported receiving Tdap. HCP reported receipt of Tdap more often than did non-HCP. |
| Age at First Dose of HPV Vaccination | Box 1/ Table 4 [1 sheet] Table 4 HPV Age at 1st dose |
Among women 19-26 years, 10.6% reported receiving the first dose of HPV vaccine at 11-12 years, 67.0% at 13-17 years, and 10.9% at 19-26 years. Among males 19-26 years, 9.8% reported receiving the first dose of HPV vaccine at 11-12 years, 53.0% at 13-17 years, and 21.6% at 19-26 years. Among respondents 19–26 years, the difference between the age reported at the time of the interview and the age at which respondents indicated that the first dose of HPV vaccine was received was ≥12 years for 4.8% of women and for 6.2% of males. This would imply receipt of vaccination in 2004 or earlier, before HPV vaccine was licensed for use in 2006. |
| Racial/Ethnic Differences in Vaccination Coverage Among Adults | Box 1/ Table 5 [1 sheet] Table 5 Summary RE diff |
Compared with 2015, racial/ethnic differences in vaccination coverage persisted for all seven vaccines in this report [7 sheets]. With whites as the reference group, there were differences in vaccination coverage for 48 of the 66 comparisons by vaccine and age/target groups (not including comparisons of the “other” race/ethnic group). |
| Average Change in Racial/Ethnic Vaccination Coverage Differences Among Adults, 2010–2016 | Box 1/ Table 6 [1 sheet] Table 6 Avg change RE diff |
During 2010–2016, vaccination differences between whites and blacks increased for tetanus and diphtheria toxoids (Td) (adults ≥19 years and 19-49 years), Tdap (all age groups), hepatitis A (adults 19-49 years), hepatitis B (adults 19-49 years and HCP ≥19 years), and herpes zoster vaccination (adults ≥60 years and ≥65 years). Among Hispanics, vaccination differences increased over this time period compared with whites for Tdap (all age groups), hepatitis A (adults 19-49 years), and herpes zoster vaccination (adults ≥60 years and ≥65 years). For Asians, vaccination differences increased over this time period compared with whites for Tdap (adults 19-64 years) and herpes zoster vaccination (adults ≥60 years and ≥65 years). |
| Supplementary Table | URL (hyperlinked) | Result summary |
|---|---|---|
| Association of Health Insurance Status with Vaccination Coverage Among Adult Populations | Box 2/ Table 1 [1 sheet] SuppTable 1 Insurance – overall |
Overall, vaccination coverage was generally lower among adults without health insurance compared with those with health insurance. Adult vaccination coverage differed by the type of health insurance. Generally, vaccination coverage was higher among adults with private health insurance compared with those reporting public health insurance. |
| Association of Health Insurance Status and Having a Usual Place for Health Care with Vaccination Coverage | Box 2/ Table 2 [1 sheet] Supp Table 2 Ins – physician |
Generally, adults with a usual place for health care were more likely to report having received recommended vaccinations than those who did not have a usual place for health care, regardless of whether they had health insurance. Among adults with health insurance, coverage was higher among those who reported having a usual place for health care compared with those who did not have a usual place for health care. |
| Adult Vaccination Coverage by Health Insurance Status and Physician Contacts | Box 2/ Table 3 [1 sheet] Supp Table 3 Ins – contacts |
Generally, vaccination coverage was higher among those reporting having had one or more physician contacts in the past year compared with those who had not visited a physician in the past year, regardless of whether they had health insurance. In addition, vaccination coverage generally increased as the number of physician contacts increased. Among adults who had health insurance and ≥10 physician contacts within the past year, 23.7%–83.3% reported not having received a vaccine or vaccine series that were recommended either for all persons or for those with some specific indication. |
| Association of Respondent Age with Adult Vaccination Coverage | Box 2/ Table 1, 2, 3 [1 sheet] SuppTable 1 Insurance – overall Supp Table 2 Ins – physician Supp Table 3 Ins – contacts |
Influenza and pneumococcal vaccination coverage among adults ≥65 years was higher compared with coverage among adults 19–64 years; however, Td and Tdap coverage among adults ≥65 years was lower compared with coverage among adults <65 years. Hepatitis B vaccination coverage among adults with diabetes ≥60 years was lower compared with coverage among adults 19–59 years with diabetes. †Herpes zoster coverage among adults ≥65 years was higher compared with coverage among adults 60–64 years). |
| Adult Vaccination Coverage Adjusted for Selected Demographic and Access to Care Characteristics | Box 2/ Table 4 [1 sheet] Supp Table 4 Ins – adjusted |
Adults without health insurance were less likely than those with health insurance to be vaccinated after adjusting for confounders for influenza (≥19 years); pneumococcal (19-64 years, increased risk);Td (≥19 years); Tdap (≥19 years); hepatitis B (≥19 years and 19-49 years); and herpes zoster (≥60 years). |
| Adult Vaccination Coverage by Nativity, Years Living in the United States, and Citizenship | Box 2/ Table 5 [1 sheet] Supp Table 5 Nativity |
Overall, vaccination coverage among U.S.-born respondents was higher than that of foreign-born respondents with few exceptions (influenza vaccination [adults 19–49 years], hepatitis A vaccination [adults ≥19 years], and hepatitis B vaccination [adults ≥19 years with diabetes; 19-59 years with diabetes; ≥60 years with diabetes]). Compared with U.S.-born adults, there were large gaps in vaccination coverage among foreign-born adults for pneumococcal vaccination (>65 years), herpes zoster (>65 years), HPV vaccination (females 19-26 years), tetanus (≥19 years) and Tdap vaccination (adults ≥19 years). Vaccination status varied by time living in the United States. Coverage among foreign-born adults who were U.S. citizens was generally higher than that for foreign-born respondents who were not U.S. citizens. |
† In 2011, the Advisory Committee on Immunization Practices (ACIP) recommended hepatitis B vaccination for persons with diabetes 19–59 years and stated that persons with diabetes aged 60 years and older should be considered for vaccination.