Colchicine: Biotoxin
CAS #:
64-86-8
RTECS #: GH0700000
UN #: 3249 (Guide 151)
Common Names:
- Colchineos
- Colcin
Agent Characteristics
Pale yellow to greenish-yellow crystals, scales, or powder; darkens when exposed to light.
Colchicine is a highly toxic plant hormone that is used medically in the treatment of gout and in scientific research. Colchicine stops the process of cell division (it is an antimitotic agent). Exposure to colchicine can be fatal in very small doses (e.g., 7 to 65 mg). Colchicine is derived from the meadow saffron or autumn crocus plant (Colchicum autumnale), which is locally abundant in meadows throughout most of Europe and has become naturalized in parts of North America. It can also be found in the tubers of the Glory Lily (Gloriosa superba) found primarily in Florida. It is odorless or nearly so and has a very bitter taste. It is produced in tablets, granules, and ampules of sterile solution. It has uses in the production of legitimate and illicit plant production.
- Indoor Air: Colchicine can be released into indoor air as fine particles or liquid spray (aerosol).
- Water: Colchicine can be used to contaminate water.
- Food: Colchicine can be used to contaminate food.
- Outdoor Air: Colchicine can be released into outdoor air as fine particles or liquid spray (aerosol).
- Agricultural: If colchicine is released into the air as fine particles or liquid spray (aerosol), it has the potential to contaminate agricultural products.
Colchicine can be absorbed into the body by ingestion, inhalation, or eye contact. Colchicine can also be injected through the skin or administered intravenously. It is unknown whether colchicine can be absorbed through intact skin.
Personal Protective Equipment
First Responders should use a NIOSH-certified Chemical, Biological, Radiological, Nuclear (CBRN) Self Contained Breathing Apparatus (SCBA) with a Level A protective suit when entering an area with an unknown contaminant or when entering an area where the concentration of the contaminant is unknown. Level A protection should be used until monitoring results confirm the contaminant and the concentration of the contaminant.
NOTE: Safe use of protective clothing and equipment requires specific skills developed through training and experience.
Select when the greatest level of skin, respiratory, and eye protection is required. This is the maximum protection for workers in danger of exposure to unknown chemical hazards or levels above the IDLH or greater than the AEGL-2.
- A NIOSH-certified CBRN full-face-piece SCBA operated in a pressure-demand mode or a pressure-demand supplied air hose respirator with an auxiliary escape bottle.
- A Totally-Encapsulating Chemical Protective (TECP) suit that provides protection against CBRN agents.
- Chemical-resistant gloves (outer).
- Chemical-resistant gloves (inner).
- Chemical-resistant boots with a steel toe and shank.
- Coveralls, long underwear, and a hard hat worn under the TECP suit are optional items.
Select when the highest level of respiratory protection is necessary but a lesser level of skin protection is required. This is the minimum protection for workers in danger of exposure to unknown chemical hazards or levels above the IDLH or greater than AEGL-2. It differs from Level A in that it incorporates a non-encapsulating, splash-protective, chemical-resistant splash suit that provides Level A protection against liquids but is not airtight.
- A NIOSH-certified CBRN full-face-piece SCBA operated in a pressure-demand mode or a pressure-demand supplied air hose respirator with an auxiliary escape bottle.
- A hooded chemical-resistant suit that provides protection against CBRN agents.
- Chemical-resistant gloves (outer).
- Chemical-resistant gloves (inner).
- Chemical-resistant boots with a steel toe and shank.
- Coveralls, long underwear, a hard hat worn under the chemical-resistant suit, and chemical-resistant disposable boot-covers worn over the chemical-resistant suit are optional items.
Select when the contaminant and concentration of the contaminant are known and the respiratory protection criteria factors for using Air Purifying Respirators (APR) or Powered Air Purifying Respirators (PAPR) are met. This level is appropriate when decontaminating patient/victims.
- A NIOSH-certified CBRN tight-fitting APR with a canister-type gas mask or CBRN PAPR for air levels greater than AEGL-2.
- A NIOSH-certified CBRN PAPR with a loose-fitting face-piece, hood, or helmet and a filter or a combination organic vapor, acid gas, and particulate cartridge/filter combination or a continuous flow respirator for air levels greater than AEGL-1.
- A hooded chemical-resistant suit that provides protection against CBRN agents.
- Chemical-resistant gloves (outer).
- Chemical-resistant gloves (inner).
- Chemical-resistant boots with a steel toe and shank.
- Escape mask, face shield, coveralls, long underwear, a hard hat worn under the chemical-resistant suit, and chemical-resistant disposable boot-covers worn over the chemical-resistant suit are optional items.
Select when the contaminant and concentration of the contaminant are known and the concentration is below the appropriate occupational exposure limit or less than AEGL-1 for the stated duration times.
- Limited to coveralls or other work clothes, boots, and gloves.
Emergency Response
- When heated to decomposition, colchicine emits toxic fumes of carbon monoxide, carbon dioxide, and nitrogen oxides.
- Colchicine is incompatible with strong oxidants and mineral acids.
- Upper and lower explosive (flammable) limits in air are not available for colchicine.
- Colchicine is non-combustible.
- The agent itself does not burn, but it may decompose upon heating to produce corrosive and/or toxic fumes.
- Fire may produce irritating, corrosive, and/or toxic gases.
- For small fires, use dry chemical, carbon dioxide, or water spray.
- For large fires, use water spray, fog, or regular foam. Move containers from the fire area if it is possible to do so without risk to personnel. Dike fire control water for later disposal; do not scatter the material. Use water spray or fog; do not use straight streams.
- For fire involving tanks or car/trailer loads, fight the fire from maximum distance or use unmanned hose holders or monitor nozzles. Do not get water inside containers. Cool containers with flooding quantities of water until well after the fire is out. Withdraw immediately in case of rising sound from venting safety devices or discoloration of tanks. Always stay away from tanks engulfed in fire.
- For massive fire, use unmanned hose holders or monitor nozzles; if this is impossible, withdraw from the area and let the fire burn.
- Run-off from fire control or dilution water may be corrosive and/or toxic, and it may cause pollution.
- If the situation allows, control and properly dispose of run-off (effluent).
- If a tank, rail car, or tank truck is involved in a fire, isolate it for 0.5 mi (800 m) in all directions; also consider initial evacuation for 0.5 mi (800 m) in all directions.
- This agent is not included in the DOT ERG 2004 Table of Initial Isolation and Protective Action Distances.
- In the DOT ERG 2004 orange-bordered section of the guidebook, there are public safety recommendations to isolate a colchicine (Guide 151) spill or leak area immediately for at least 150 ft (50 m) for liquids and 75 ft (25 m) for solids in all directions.
- Colchicine withstands drying, storage, or boiling.
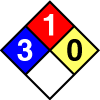
- Health: 3
- Flammability: 1
- Reactivity: 0
- Special:
- OSHA: Not established/determined
- NIOSH: Not established/determined
- AIR MATRIX
No references were identified for this sampling matrix for this agent. - OTHER
Hoja H, Marquet P, Verneuil B, Lotfi H, Dupuy JL, Dreyfuss MF, Lachatre G [1996]. Determination of colchicine in biological fluids by liquid chromatography mass spectrometry with pneumatically assisted electrospray ionization. Analusis 24(9-10):391-394.Ko RJ, Li WY, Koda RT [1990]. Determination of the antimitotic agents N-Desacetylcolchicine, demecolcine and colchicine in serum and urine. J Chromatogr B: Biomed Sci Appl 525:411-418.
Li W, Fitzloff JF, Farnsworth NR, Fong HHS [2002]. Evaluation of commercial Ginkgo biloba dietary supplements for the presence of colchicine by high-performance liquid chromatography. Phytomedicine 9(5):442-446.
Tracqui A, Kintz P, Ludes B, Rougé C, Douibi H, Mangin P [1996]. High-performance liquid chromatography coupled to ion spray mass spectrometry for the determination of colchicine at ppb levels in human biofluids. J Chromatogr B: Biomed Sci Appl 675(2):235-242.
- SOIL MATRIX
No references were identified for this sampling matrix for this agent. - SURFACES
No references were identified for this sampling matrix for this agent. - WATER
Kasim EA [2002]. Voltammetric behavior of the anti-inflammatory alkaloid colchicine at a glassy carbon electrode and a hanging mercury electrode and its determination at PPB levels. Anal Lett 35(12):1987-2004.Wang J, Ozsoz M [1990]. Trace measurements of colchicine by adsorptive stripping voltammetry. Talanta 37(8):783-787.
Wang Y, Wang KM, Liu WH, Shen GL, Yu RQ [1997]. A new fluorescence optical-fiber sensor for colchicines. Anal Sci 13(3):447-451.
Signs/Symptoms
Colchicine toxicity may be fatal. Patient/victims may be asymptomatic up to 24 hours post exposure. Onset of gastrointestinal signs and symptoms may occur as early as 2 hours and as late as 24 hours post exposure. Onset of multiple system organ failure may occur within 24 to 72 hours. Recovery may begin within 6 to 8 days post exposure.
The first phase of colchicine toxicity consists of gastrointestinal symptoms: burning sensation in the throat, nausea, vomiting, diarrhea, and abdominal pain. Excessive fluid loss from vomiting and diarrhea may result in hypovolemic shock. Patient/victims suffering from mild exposure may have no further adverse effects.
- Eye contact with liquid colchicine may produce clouding of the cornea that clears in a few weeks.
- See Ingestion Exposure.
- Gastrointestinal phase: Nausea; loss of appetite (anorexia); abdominal pain; vomiting (emesis); profuse, watery, and bloody diarrhea; joint pain; generalized weakness; fever; rashes; and hypovolemic shock.
- Multiple system organ failure phase: Hypovolemic shock due to extreme vascular damage and fluid loss through the GI tract may result in death; kidney damage resulting in low urine output and bloody urine; swollen, tender liver with elevated liver enzymes; low white blood cell counts (persisting for several days); other blood (hematologic) manifestations including bone marrow depression, low platelets, and anemia; muscular weakness; ascending paralysis that may result in respiratory failure; and loss of deep tendon reflexes. The patient/victim usually remains conscious but exhibits mental confusion or delirium and seizures. Pediatric patient/victims may experience hallucinations.
- See Signs/Symptoms Ingestion Exposure.
- Not established/determined.
Decontamination
The purpose of decontamination is to make an individual and/or their equipment safe by physically removing toxic substances quickly and effectively. Care should be taken during decontamination, because absorbed agent can be released from clothing and skin as a gas. Your Incident Commander will provide you with decontaminants specific for the agent released or the agent believed to have been released.
The following are recommendations to protect the first responders from the release area:
- Position the decontamination corridor upwind and uphill of the hot zone.
- The warm zone should include two decontamination corridors. One decontamination corridor is used to enter the warm zone and the other for exiting the warm zone into the cold zone. The decontamination zone for exiting should be upwind and uphill from the zone used to enter.
- Decontamination area workers should wear appropriate PPE. See the PPE section of this card for detailed information.
- A solution of detergent and water (which should have a pH value of at least 8 but should not exceed a pH value of 10.5) should be available for use in decontamination procedures. Soft brushes should be available to remove contamination from the PPE.
- Labeled, durable 6-mil polyethylene bags should be available for disposal of contaminated PPE.
The following methods can be used to decontaminate an individual:
- Decontamination of First Responder:
- Begin washing PPE of the first responder using soap and water solution and a soft brush. Always move in a downward motion (from head to toe). Make sure to get into all areas, especially folds in the clothing. Wash and rinse (using cold or warm water) until the contaminant is thoroughly removed.
- Remove PPE by rolling downward (from head to toe) and avoid pulling PPE off over the head. Remove the SCBA after other PPE has been removed.
- Place all PPE in labeled durable 6-mil polyethylene bags.
- Decontamination of Patient/Victim:
- Remove the patient/victim from the contaminated area and into the decontamination corridor.
- Remove all clothing (at least down to their undergarments) and place the clothing in a labeled durable 6-mil polyethylene bag.
- Thoroughly wash and rinse (using cold or warm water) the contaminated skin of the patient/victim using a soap and water solution. Be careful not to break the patient/victim’s skin during the decontamination process, and cover all open wounds.
- Cover the patient/victim to prevent shock and loss of body heat.
- Move the patient/victim to an area where emergency medical treatment can be provided.
First Aid
Initial treatment is primarily supportive. It includes relief of abdominal pain, measures to combat shock, and establishment of adequate respiratory exchange by maintenance of an adequate airway, control of respiration, and oxygen administration.
There is no antidote for colchicine toxicity.
- Immediately remove the patient/victim from the source of exposure.
- Immediately wash eyes with large amounts of tepid water for at least 15 minutes.
- Seek medical attention immediately.
- Immediately remove the patient/victim from the source of exposure.
- Ensure that the patient/victim has an unobstructed airway.
- Do not induce vomiting (emesis).
- Administer charcoal as a slurry (240 mL water/30 g charcoal). Usual dose: 25 to 100 g in adults/adolescents, 25 to 50 g in children (1 to 12 years), and 1 g/kg in infants less than 1 year old.
- If the patient/victim can be rapidly transported to an emergency department for decontamination, stomach pumping (gastric lavage) may be considered after the airway has been secured. Gastric lavage is recommended only after ingestion of a life-threatening amount of the agent and only if it can be done shortly after ingestion (generally within 1 hour). The risk of worsening injury to the lining of the gastrointestinal (GI) tract must be considered.
- If evidence of shock or low blood pressure (hypotension) is observed, begin intravenous (IV) fluid administration.
- Also see First Aid for Inhalation Exposure.
- Seek medical attention immediately.
- Immediately remove the patient/victim from the source of exposure.
- Evaluate respiratory function and pulse.
- Ensure that the patient/victim has an unobstructed airway.
- If shortness of breath occurs or breathing is difficult (dyspnea), administer oxygen.
- Assist ventilation as required. Always use a barrier or bag-valve-mask device.
- If breathing has ceased (apnea), provide artificial respiration.
- If evidence of shock or low blood pressure (hypotension) is observed, begin intravenous (IV) fluid administration.
- Also see First Aid for Ingestion Exposure.
- Seek medical attention immediately.
- Immediately remove the patient/victim from the source of exposure.
- See the Decontamination section for patient/victim decontamination procedures.
- Seek medical attention immediately.
Long-Term Implications
Patient/victims exposed to colchicine by ingestion should be observed for gastrointestinal symptoms for 12 hours following acute exposure. Heart function should be monitored, and the patient/victim should be evaluated for low blood pressure (hypotension), abnormal heart rhythms (dysrhythmias), and reduced respiratory function (respiratory depression). Monitor other organ systems as appropriate.
Gastrointestinal signs and symptoms are followed by multiple system organ failure. This is marked by bone marrow suppression, whole body vascular system clotting (disseminated intravascular coagulopathy), adult respiratory distress, cardiac dysfunction (dysrhythmia, failure, and arrest), intestinal obstruction (ileus), neuromuscular abnormalities (ascending paralysis, rhabdomyolysis, neuritis, and peripheral neuropathies), kidney failure, sepsis, fever, metabolic disturbances, and mental status changes are all key features of this stage. Death during this stage can result from hypovolemic, cardiac, or septic shock. These effects are due to a combination of colchicine’s direct action on organs as well as massive infection from sepsis.
Patient/victims surviving multiple system organ failure will begin to experience recovery after 6 to 8 days. Recovery is marked by an increase in white blood cell count (rebound leukocytosis), reversible hair loss (alopecia), and return of normal organ system functions.
Information is inconclusive about the carcinogenicity, developmental toxicity, or reproductive toxicity from chronic or repeated exposure to colchicine. Effects of chronic exposure to colchicine are mainly known from its use as a drug in human medicine. In these circumstances gastrointestinal symptoms are likely to cause discontinuation of the use of the drug, long before any other symptoms develop. Bone marrow depression with a condition marked by fever and other symptoms (agranulocytosis), persistent decrease in the number of blood platelets (thrombocytopenia), reduced white blood cell count (leukopenia), and anemia characterized by defective function of the blood-forming organs (aplastic anemia) may occur with prolonged colchicine administration. Loss of body and scalp hair (alopecia), rashes, blister-like inflammation of the skin (vesicular dermatitis), degeneration of certain nerves (peripheral neuritis or neuropathy), a break down of muscle tissue at the cellular level (myopathy), the absences of urine excretion (anuria), kidney (renal) damage, blood in the urine (hematuria), and one case of patches of purplish discoloration of the skin and mucous membranes (purpura) have also been reported with prolonged administration of colchicine.
On-Site Fatalities
- Consult with the Incident Commander regarding the agent dispersed, dissemination method, level of PPE required, location, geographic complications (if any), and the approximate number of remains.
- Coordinate responsibilities and prepare to enter the scene as part of the evaluation team along with the FBI HazMat Technician, local law enforcement evidence technician, and other relevant personnel.
- Begin tracking remains using waterproof tags.
- Wear PPE until all remains are deemed free of contamination.
- Establish a preliminary (holding) morgue.
- Gather evidence, and place it in a clearly labeled impervious container. Hand any evidence over to the FBI.
- Remove and tag personal effects.
- Perform a thorough external evaluation and a preliminary identification check.
- See the Decontamination section for decontamination procedures.
- Decontaminate remains before they are removed from the incident site.
Occupational Exposure Limits
- NIOSH REL:
- Not established/determined
- OSHA PEL:
- Not established/determined
- ACGIH TLV:
- Not established/determined
- NIOSH IDLH: Not established/determined
- DOE TEEL:
- TEEL-0: 0.04 mg/m3
- TEEL-1: 0.125 mg/m3
- TEEL-2: 0.9 mg/m3
- TEEL-3: 0.9 mg/m3
- AIHA ERPG:
- ERPG-1: Not established/determined
- ERPG-2: Not established/determined
- ERPG-3: Not established/determined
Acute Exposure Guidelines
| 5 min | 10 min | 30 min | 1 hr | 4 hr | 8 hr | |
|---|---|---|---|---|---|---|
| AEGL 1 (discomfort, non-disabling) – mg/m3 |
Not established/ determined | Not established/ determined | Not established/ determined | Not established/ determined | Not established/ determined | Not established/ determined |
| AEGL 2 (irreversible or other serious, long-lasting effects or impaired ability to escape) – mg/m3 |
Not established/ determined | Not established/ determined | Not established/ determined | Not established/ determined | Not established/ determined | Not established/ determined |
| AEGL 3 (life-threatening effects or death) – mg/m3 |
Not established/ determined | Not established/ determined | Not established/ determined | Not established/ determined | Not established/ determined | Not established/ determined |
Decontamination (Environment and Equipment)
The following methods can be used to decontaminate the environment/spillage disposal:
- Do not touch or walk through the spilled agent if at all possible. However, if you must, personnel should wear the appropriate PPE during environmental decontamination. See the PPE section of this card for detailed information.
- Keep combustibles (e.g., wood, paper, and oil) away from the spilled agent.
- Use water spray to reduce vapors or divert vapor cloud drift. Avoid allowing water runoff to contact the spilled agent.
- Do not direct water at the spill or the source of the leak.
- Stop the leak if it is possible to do so without risk to personnel, and turn leaking containers so that gas rather than liquid escapes.
- Prevent entry into waterways, sewers, basements, or confined areas.
- Isolate the area until gas has dispersed.
- Ventilate the area.
Agents can seep into the crevices of equipment making it dangerous to handle. The following methods can be used to decontaminate equipment:
- Not established/determined
Agent Properties
- Chemical Formula:
C22H25NO6 - Aqueous solubility:
Slightly soluble - Boiling Point:
Not established/determined - Density:
Not established/determined - Flammability:
Not combustible - Flashpoint:
Not established/determined
- Ionization potential:Not established/determined
- Log Kbenzene-water:
Not established/determined - Log Kow (estimated):
1.86 - Melting Point:
287.6°F to 302°F (142°C to 150°C) - Molecular Mass:
399.44
- Soluble In:1 g/220 mL ether; 1 g/100 mL benzene; freely soluble in alcohol or chloroform; soluble in methanol
- Specific Gravity:
Not established/determined - Vapor Pressure:
Not established/determined - Volatility:
Not established/determined
Hazardous Materials Warning Labels/Placards
- Shipping Name:
Medicine, solid, toxic, n.o.s. - Identification Number:
3249 (Guide 151) - Hazardous Class or Division:
6.1 - Subsidiary Hazardous Class or Division:
- Label:
Poison (Toxic),PG III - Placard Image:
Trade Names and Other Synonyms
- Acetamide, N-(5,6,7,9-tetrahydro-1,2,3,10-tetramethoxy-9-oxobenzo(a)heptalen-7-yl)-, (S)-
- 7-Acetamido-6,7-dihydro-1,2,3,10-tetramethoxybenzo[a]heptalen-9(5H)-one
- N-Acetyltrimethylcolchicinic acid methyl ether
- Benzo(a)heptalen-9(5H)-one
- Colchiceine methyl ether
- Colchicin (German)
- Colchicina (Italian)
- 7alpha-H-Colchicine
- Colchicine crystalline
- Colcin
- Colgout
- Colsaloid
- Condylon
- N-(5,6,7,9-Tetrahydro-1,2,3,10-tetramethoxy-9-oxobenzo[a]heptalen-7-yl)acetamide
- (S)-N-(5,6,7,9-Tetrahydro-1,2,3,10-tetramethoxy-9-oxobenzo[a]heptalen-7-yl)acetamide
In the event of a poison emergency, call the poison center immediately at 1-800-222-1222. If the person who is poisoned cannot wake up, has a hard time breathing, or has convulsions, call 911 emergency services.
For information on who to contact in an emergency, see the CDC website at emergency.cdc.gov or call the CDC public response hotline at (888) 246-2675 (English), (888) 246-2857 (Español), or (866) 874-2646 (TTY).
The user should verify compliance of the cards with the relevant STATE or TERRITORY legislation before use. NIOSH, CDC 2003.