 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Compendium of Measures To Prevent Disease Associated with Animals in Public Settings, 2005National Association of State Public Health Veterinarians, Inc. (NASPHV) Prepared by This report has been endorsed by CDC, the Council of State and Territorial Epidemiologists, and the American Veterinary Medical Association. The material in this report originated in the National Center for Infectious Diseases, Anne Schuchat, MD, Director; and the Division of Bacterial and Mycotic Diseases, Judith R. Aguilar, Acting Director. Corresponding preparer: J.B. Bender DVM, Co-chair, NASPHV Animal Contact Compendium Committee, University of Minnesota, Veterinary Public Health, 136F Andrew Boss, 1354 Eckles Avenue, St. Paul, MN 55108, Telephone: 612-625-6203; Fax: 612-624-4906; E-mail: bende002@umn.edu. Disclosure of Relationship: CDC, the National Association of State Public Health Veterinarians (NASPHV), our planners, and our content professionals have disclosed that they have no financial interests or other relationships with the manufactures of commercial products, suppliers of commercial services, or commercial supporters. This report does not include any discussion of the unlabeled use of a product or a product under investigational use.
SummaryMultiple venues encourage or permit the public to come in contact with animals, resulting in millions of human-animal contacts each year. These settings include county or state fairs, petting zoos, animal swap meets, pet stores, zoologic institutions, circuses, carnivals, farm tours, livestock-birthing exhibits, educational exhibits at schools, and wildlife photo opportunities. Although multiple benefits of human-animal contact exist, infectious diseases, rabies exposures, injuries, and other human health problems associated with these settings are of concern. Rabid or potentially rabid animals in public settings can result in extensive public health investigation and action. Infectious disease outbreaks reported during the previous decade have been attributed to multiple organisms, including Escherichia coli O157:H7, Salmonella, Coxiella burnetti, Mycobacterium tuberculosis, and ringworm. Such incidents have substantial medical, public health, legal, and economic effects. This report provides standardized recommendations for public health officials, veterinarians, animal venue operators, animal exhibitors, visitors to animal venues and exhibits, and others concerned with disease-control and with minimizing risks associated with animals in public settings. The recommendation to wash hands is the single most important prevention step for reducing the risk for disease transmission. Other critical recommendations are that venues include transition areas between animal areas and nonanimal areas (where food is sold) and that animals are properly cared for and managed in public settings. In addition, this report recommends educating venue operators, staff, exhibitors, and visitors regarding the risk for disease transmission where animal contact is possible. IntroductionContact with animals in public settings (e.g., fairs, farm tours, and petting zoos) provides opportunities for entertainment and education concerning animals and animal husbandry. However, inadequate understanding of disease transmission and animal behavior can lead to infectious diseases, rabies exposures, injuries, and other health problems among visitors, especially children, in these settings. Diseases called zoonoses or zoonotic diseases can be transmitted from animals to humans. Of particular concern are situations in which substantial numbers of persons are exposed to zoonotic disease or become ill, necessitating public health investigation and medical follow-up. A 2004 review identified >25 human infectious disease outbreaks during 1990--2000 associated with visitors to animal exhibits (1). The National Association of State Public Health Veterinarians (NASPHV) recognizes the positive benefits of human-animal contact. NASPHV considers that the risks of these contacts can be minimized in properly supervised and managed settings by using appropriately selected animals that receive regular health examinations and preventive care. Although eliminating all risk from animal contacts might not be achievable, this report provides standardized recommendations for minimizing disease and injury. NASPHV recommends that local and state public health, agricultural, environmental, and wildlife agencies, and other organizations use these recommendations to establish their own guidelines or regulations for reducing the risk for disease from human-animal contact in public settings. Multiple venues exist where public contact with animals is permitted (e.g., animal displays, petting zoos, animal swap meets, pet stores, zoologic institutions, nature parks, circuses, carnivals, farm tours, livestock-birthing exhibits, county or state fairs, schools, and wildlife photo opportunities). Persons responsible for managing these venues are encouraged to use the information in this report to reduce risk. Guidelines to reduce risks for disease from animals in health-care facilities and service animals (e.g., guide dogs) have been developed (2--4). These settings are not specifically addressed in this report, although the general principles and recommendations might be applicable. Enteric (Intestinal) DiseasesInfections with enteric bacteria and parasites pose the highest risk for human disease from animals in public settings (5). Healthy animals harbor multiple human enteric pathogens. Certain organisms have a low infectious dose (6--8). Because of the popularity of animal venues, a substantial number of persons might be exposed to these organisms. Reports of illness and outbreaks among visitors to fairs, farms, and petting zoos have been documented. Pathogens linked to outbreaks include Escherichia coli O157:H7, Campylobacter, Salmonella, and Cryptosporidium (9--17). Although these reports usually document cattle, sheep, and goats as sources for infection, poultry (18--21) and other domestic and wild animals also are potential sources. The primary mode of transmission for enteric pathogens is the fecal-oral route. Because animal fur, hair, skin, and saliva (22) can become contaminated with fecal organisms, transmission might occur when persons pet, touch, or are licked by animals. Transmission has also occurred from fecal contamination of food, including raw milk (23--25), sticky foods (e.g., cotton candy [26]), water (27--29), and environmental surfaces (12,18,30,31). Animals infected with enteric pathogens (e.g., E. coli O157:H7, Salmonella, and Campylobacter) frequently exhibit no signs of illness and might shed pathogens intermittently. Therefore, although removing ill animals (especially those with diarrhea) is necessary to protect animal and human health, it is not sufficient: animals that appear to be healthy might still be infectious and contaminate the environment. Certain organisms live months or years in the environment (32--36). Because of intermittent shedding and limitations of laboratory tests, culturing fecal specimens or other attempts to identify, screen, and remove infected animals might not be effective in eliminating the risk for transmission. Antimicrobial treatment of animals cannot be depended upon to eliminate infection and shedding of enteric pathogens or to prevent reinfection. Multiple factors increase the probability of transmission at animal exhibits. Animals are more likely to shed pathogens because of stress induced by prolonged transportation, confinement, crowding, and increased contact with persons (37--43). Commingled animals increase the probability that animals shedding organisms will infect other animals. The prevalence of certain enteric pathogens might be higher in young animals (44--46), which are frequently exhibited by petting zoos. Shedding of E. coli O157:H7 and Salmonella is highest in the summer and fall when substantial numbers of traveling animal exhibits, agricultural fairs, and petting zoos are scheduled (43,47,48). The risk for infections or outbreaks is increased by certain human factors and behaviors. These factors include inadequate hand washing, venues that attract substantial numbers of children, a lack of close supervision of children, hand-to-mouth activities (e.g., use of pacifiers, thumb-sucking, smoking, and eating) in proximity to animals, and a lack of awareness of the risk. The layout and maintenance of facilities and animal exhibits can also contribute to the risk for infection. Risk factors include inadequate hand-washing facilities (1), structural deficiencies associated with temporary food-service facilities, inadequate separation between animal exhibits and food-consumption areas (49), and contaminated or inadequately maintained drinking water and sewage/manure disposal systems (27-- 29,31). Lessons from OutbreaksTwo E. coli O157:H7 outbreaks in Pennsylvania and Washington State led to CDC establishing recommendations for enteric disease prevention in animal contact settings (http://www.cdc.gov/foodborneoutbreaks/pulication/recomm_farm_animal.htm). Findings in both outbreaks were animal contact at farms open to the public and inadequate hand washing (14,16). In the Pennsylvania outbreak, 51 persons (median age: 4 years) became ill within 10 days of visiting a dairy farm, and eight (16%) developed hemolytic uremic syndrome (HUS), a potentially fatal consequence of E. coli O157:H7 infection. The same strain of E. coli O157:H7 was isolated from cattle, case-patients, and the farm environment. In addition to the reported cases, an increased number of diarrhea cases in the community were attributed to visiting the farm. An assessment of the farm environment determined that 1) no areas existed for eating and drinking that were separate from the animal contact areas, and 2) the limited hand-washing facilities were not configured for children (14). Failure to properly wash hands was also a contributing factor in other outbreaks caused by Cryptosporidium (11) and Salmonella (12). The protective effect of hand washing and the persistence of organisms in the environment were demonstrated in an outbreak of Salmonella infections at a Colorado zoo. Sixty-five cases (the majority of them children) were associated with touching a wooden barrier around the Komodo dragon exhibit. Noninfected children were substantially more likely to have washed their hands after visiting the exhibit. Salmonella was isolated from 39 case-patients, a Komodo dragon, and the wooden barrier (12). During 2000--2001 at a Minnesota children's farm day camp, washing hands with soap after touching a calf and washing hands before going home were protective factors in two outbreaks involving multiple enteric organisms (50). A total of 84 illnesses were documented among attendees. Implicated organisms for the human infections were E. coli O157:H7, Cryptosporidium parvum, non-O157 Shiga toxin-producing E. coli (STEC), Salmonella enterica serotype Typhimurium, and Campylobacter jejuni. These organisms, as well as Giardia, were also isolated from the calves. Risk factors for children included caring for an ill calf and getting visible manure on their hands. Enteric pathogens can contaminate and persist in animal housing areas. For example, E. coli O157:H7 can survive in soil for months (31,32,34,51). Prolonged environmental persistence of pathogens was documented in an Ohio outbreak of E. coli O157 infections in which 23 persons became ill at a fair after handling sawdust, attending a dance, or eating and drinking in a building where animals were exhibited during the previous week (31). Fourteen weeks after the fair ended, E. coli O157 was isolated from multiple environmental sources within the building, including sawdust on the floor and dust on the rafters. Forty-two weeks after the fair ended, E. coli O157 was recovered from sawdust on the floor. Transmission of E. coli O157:H7 from airborne dust was implicated in an Oregon county fair outbreak with 60 cases, the majority of them children (18). Illness was associated with visiting an exhibition hall that housed goats, sheep, pigs, rabbits, and poultry but was not associated with touching animals or their pens, eating, or inadequate hand washing. The same organism was recovered from ill persons and the building. In 2004, an outbreak of E. coli O157:H7 infection was associated with attendance at a goat and sheep petting zoo at the North Carolina State Fair (51). Health officials investigated 112 case-patients, including 15 who had HUS. The same strain of E. coli O157:H7 infecting case-patients was isolated from the animal bedding 10 days after the fair was over. The strain was also isolated from the soil after the animal bedding was removed. The effect of improper facility design was illustrated by one of the most substantial waterborne outbreaks in the United States (28,29). Approximately 800 suspected cases of E. coli O157:H7 and Campylobacter were identified among attendees at a New York county fair where the water and sewage systems had deficiencies. Sporadic InfectionsMultiple sporadic infections, not identified as part of recognized outbreaks, have been associated with animal environments. A study of sporadic E. coli O157:H7 infections among selected U.S. states and counties determined that case-patients, especially children, were more likely to have visited a farm with cows than healthy persons (52). Additional studies also documented an association between E. coli O157:H7 infection and visiting a farm (53) or living in a rural area (54). Studies of human cryptosporidiosis have documented contact with cattle or visiting farms as risk factors for infection (55--57). A case-control study identified multiple factors associated with Campylobacter infection, including raw milk consumption and contact with farm animals (58). In other studies, farm residents were at a lower risk for infection with Cryptosporidium (55) and E. coli O157:H7 (59) than farm visitors, probably because the residents had acquired immunity to the infection as a result of their early and frequent exposure to these organisms. Additional Health ConcernsAlthough enteric diseases are the most commonly reported health risks associated with animals in public settings, multiple other health risks are of concern. For example, allergies can be associated with animal dander, scales, fur, feathers, body wastes (urine), and saliva (60--62). Additional health concerns addressed in this report include injuries, rabies exposures, and other infections. InjuriesInjuries associated with animals in public settings include bites, kicks, falls, scratches, stings, crushing of the hands or feet, and being pinned between the animal and a fixed object. These injuries have been associated with multiple species, including big cats (e.g., tigers), monkeys, domestic animals, and zoo animals. The settings have included public stables, petting zoos, traveling photo opportunities, schools, children's parties, and animal rides.* Rabies ExposuresContact with mammals might expose persons to rabies through contamination of mucous membranes, bites, scratches, or other wounds with infected saliva or nervous tissue. Although no human rabies deaths caused by animal contact in public exhibits have been recorded, multiple rabies exposures have occurred, requiring extensive public health investigation and medical follow-up. For example, in the previous decade, thousands of persons have received rabies postexposure prophylaxis (PEP) after being exposed to rabid or potentially rabid animal species (including cats, goats, bears, sheep, ponies, and dogs) at 1) a pet store in New Hampshire (63), 2) a county fair in New York State (64), 3) petting zoos in Iowa (65,66) and Texas (J.H. Wright, DVM, Texas Department of Health, personal communication, 2004), and 4) school and rodeo events in Wyoming (1). Substantial public health and medical care challenges associated with potential mass rabies exposures include difficulty in identifying and contacting persons, correctly assessing exposure risks, and providing timely medical treatment. Prompt assessment and treatment are critical for this disease, which is usually fatal. Other InfectionsMultiple bacterial, viral, fungal, and parasitic agents have been associated with animal contact. These organisms are transmitted through various modes. Infections from animal bites are common and frequently require extensive treatment or hospitalization. Bacterial pathogens that are frequently associated with animal bites include Pasteurella, Staphylococcus, Streptococcus, Capnocytophaga canimorsus, Bartonella henselae (cat-scratch disease), and Streptobacillus moniliformis (rat-bite fever). Certain monkey species (especially macaques) that are kept as pets or used in public exhibitions can be infected with herpes B virus, either asymptomatically or with mild oral lesions. Human exposure through bites or fluids can result in a fatal meningoencephalitis (67,68). Because of difficulties with laboratory testing to confirm monkey infection and high herpes B prevalence, monkey bites can require intensive public health and medical follow-up. Skin contact with animals in public settings might also result in human infection. Fifteen cases of ringworm infection (club lamb fungus) caused by Trichophyton species and Microsporum gypseum were documented among owners and family members who exhibited lambs in Georgia during a show season (69). Ringworm infection in 23 persons and multiple animal species were traced to a Microsporum canis infection in a hand-reared zoo tiger cub (70). Orf virus infections (contagious ecthyma or sore mouth) have occurred in goats and sheep at a children's petting zoo (71) and in a lamb used for an Easter photo opportunity (M. Eidson, DVM, New York State Department of Health, personal communication, 2003). After handling various species of infected exotic animals, a zoo attendant experienced an extensive papular skin rash from a cowpox-like virus (72). In 2003, multiple cases of monkeypox occurred among persons who had had contact with infected prairie dogs either at a child care center (73,74) or a pet store (J.J. Kazmierczak, DVM, Wisconsin Department of Health and Family Services, personal communication, 2004). Ecto- and endoparasites pose concerns when humans and exhibit animals interact. Sarcoptes scabiei is a skin mite that infests humans and animals, including swine, dogs, cats, foxes, cattle, and coyotes (75,76). Although human infestation from animal sources is usually self-limiting, skin irritation and itching might occur for multiple days and be difficult to diagnose (75--77). Animal fleas bite humans, which increases the risk for infection or allergic reaction. In addition, fleas are the intermediate host for a tapeworm species that can infect children. Multiple other animal helminths might infect humans through fecal-oral contact or through contact with animals or contaminated earth (78,79). Parasite-control through veterinary care and proper husbandry coupled with hand washing reduce the risks associated with ecto- and endoparasites (80). Tuberculosis (TB) is another disease of concern in certain animal settings. Twelve circus elephant handlers at an exotic animal farm in Illinois were infected with Mycobacterium tuberculosis, and one handler had signs consistent with active disease after three elephants died of TB. Medical history and testing of the handlers indicated that the elephants had been a probable source of exposure for the majority of the human infections (81). At a zoo in Louisiana, seven animal handlers who were previously negative for TB tested positive after a Mycobacterium bovis outbreak in rhinoceroses and monkeys (82). The U.S. Department of Agriculture (USDA) developed guidelines regarding removal of infected animals from public contact as a result of concerns regarding the risk for exposure to the public (83). Zoonotic pathogens might also be transmitted by direct or indirect contact with reproductive fluids, aborted fetuses, or newborns from infected dams. Live-birthing exhibits, usually involving livestock (e.g., cattle, pigs, goats, or sheep), are popular at agricultural fairs. Although the public usually does not have direct contact with animals during birthing, newborns and their dams are frequently available for petting and observation afterward. Q fever (Coxiella burnetii), leptospirosis, listeriosis, brucellosis, and chlamydiosis are serious zoonoses that can be associated with contact with reproductive materials (84). C. burnetii is a rickettsial organism that most frequently infects cattle, sheep, and goats. The disease can cause abortion in animals, but more frequently the infection is asymptomatic. During parturition, infected animals shed substantial numbers of organisms that might become aerosolized. The majority of persons exposed to C. burnetii develop an asymptomatic infection, but clinical illness can range from an acute influenza-like illness to life-threatening endocarditis. A Q fever outbreak involving 95 confirmed case-patients and 41 hospitalizations was linked to goats and sheep giving birth at petting zoos. These petting zoos were in indoor shopping malls, indicating that indoor-birthing exhibits might pose an increased risk for Q fever transmission (85). Chlamydophila psittaci infections cause respiratory disease (commonly called psittacosis) and are usually acquired from psittacine birds (86). For example, an outbreak of C. psittaci pneumonia occurred among the staff at the Copenhagen Denmark Zoo (87). On limited occasions, chlamydial infections acquired from sheep, goats, and birds result in reproductive problems in humans (86,88,89). RecommendationsGuidelines and recommendations from multiple organizations contributed to the recommendations in this report. A limited number of states have specific guidelines or legislation for petting zoo exhibitors and other animal exhibition venues (1,16,90--92). However, in the United Kingdom, recommendations to prevent enteric infections at animal exhibitions and agricultural fairs were developed in 1989 (93), 1995 (94), and 2000 (95). In the United States, the American Zoo and Aquarium Association has accreditation standards for reducing risks of animal contact with the public in zoologic parks (96). In accordance with the Animal Welfare Act, the USDA Animal Care licenses and inspects certain animal exhibits for humane treatment of animals, but this act is not intended for human health protection. No federal laws address the risk for transmission of pathogens at venues where the public has contact with animals. However, in 2001, CDC issued guidelines to reduce the risk for enteric pathogens (16). CDC has also issued recommendations for preventing transmission of Salmonella from reptiles to humans (97). The Association for Professionals in Infection Control and Epidemiology (APIC) developed guidelines to address risks associated with the use of service animals in health-care settings (2). Opportunities for animal contact with the public occur in various settings. Recommendations provided in this report should be tailored to specific settings, and the report should be incorporated into guidelines and regulations developed at the state or local level. This report should be disseminated to persons who own or manage animals in public settings. State and local human and animal health agencies should make educational materials available to venue operators and other interested persons (90,91,98). Incidents of disease transmission or injury should be promptly reported to public health authorities and investigated. Educational Responsibilities of Venue OperatorsEducation is essential to reduce risks associated with animal contact in public settings. Animal owners, exhibit operators, and their staff should be educated to make appropriate management decisions. In addition, the public should be educated so that they can weigh the benefits and risks of animal contact and take appropriate measures to reduce risks. Recommendations include the following:
General Recommendations for Managing Public and Animal ContactThe public's contact with animals should occur in settings where controls are in place to reduce the potential for injuries or disease and increase the probability that exposures will be reported, documented, and handled appropriately. The design of facilities or contact settings should minimize the risk for exposure and facilitate hand washing (Box 1). Certain jurisdictions might choose to establish more restrictive recommendations in areas where animal contact is specifically encouraged (e.g., petting zoos). Requirements for the design of facilities or contact settings might include double barriers to prevent contact with animals or contaminated surfaces except for specified interaction areas. Manure disposal and wastewater runoff should occur in areas where the risk for exposure to pedestrians is eliminated or reduced. Control methods should focus on facility design and management. Recommendations regarding the management of animals in public settings should address animal areas (where animal contact is possible or encouraged), transition areas, and nonanimal areas (areas in which animals are not permitted, with the exception of service animals) (Figure). Specific guidelines might be necessary for certain settings (e.g., schools [Box 2]). Recommendations for cleaning procedures should be tailored to the specific situation (Appendix). Animal Areas Recommendations should be applied both to settings in which animal contact is possible (e.g., county fairs) and settings in which direct animal contact is encouraged (e.g., petting zoos). However, in settings where direct animal contact is encouraged, additional precautions should be taken to reduce the risk for injuries and disease transmission. For areas where animal contact is possible, design of the entry and exit points for animal contact areas should be planned to facilitate proper visitor flow through transition areas (Figure). These transition areas should include educational information and hand-washing facilities. Fences, gates, or other types of barriers can restrict uncontrolled access to animals and animal contact areas and ensure that visitors enter and exit through transition areas. Animal feed and water should not be accessible to the public. In addition, in buildings where animals live, adequate ventilation is essential for both animals (99) and humans. Food and beverages. No food or beverages should be allowed in animal areas. In addition, smoking, carrying toys, and use of pacifiers, spill-proof cups ("sippy cups"), and baby bottles should not be permitted in animal areas. Cleaning procedures. Manure and soiled animal bedding should be removed promptly. Animal waste and specific tools for waste removal (e.g., shovels and pitchforks) should be confined to designated areas restricted from public access. Manure and soiled bedding should not be transported or removed through nonanimal areas or transition areas used by visitors. If this is unavoidable, precautions should be taken to avoid spillage and aerosolization. During events where animal contact is encouraged, periodic disinfection of the venue might reduce the risk for disease transmission during the event. Supervision of children. Children should be closely supervised during contact with animals to discourage contact with manure and soiled bedding. Hand-to-mouth contact (e.g., thumb-sucking) should also be discouraged. Appropriate hand washing should be required. Additional recommendations for groups at high risk, including children aged <5 years, are outlined in this report (see Additional Recommendations). Staff. Trained staff should be present in areas where animal contact is permitted to encourage appropriate human-animal interactions, reduce risk for exposure (e.g., by promptly cleaning up wastes), and process reports of injuries and exposures. Feeding animals. If feeding animals is permitted, only food sold by the venue for that purpose should be allowed. Food sold for animal consumption should not be eaten by humans and should not be provided in containers that can be eaten by persons (e.g., ice cream cones). This policy will reduce the risk for animal bites and the probability of children eating food that has come into contact with animals. Use of animal areas for public (nonanimal) activities. Zoonotic pathogens can contaminate the environment for substantial periods (31). If animal areas need to be used for public events (e.g., weddings and dances), these areas should be cleaned and disinfected, particularly if food and beverages are served. Materials with smooth, impervious surfaces (e.g., steel, plastic, and sealed concrete) are easier to clean than other materials (e.g., wood or dirt floors). Removing organic material (bedding, feed, and manure) before using disinfectants is important. A list of disinfectants is included in this report (Appendix). Transition Areas Between Animal and Nonanimal Areas Providing transition areas for visitors to pass through when entering and exiting animal areas is critical. The transition areas between animal and nonanimal areas should be designated as clearly as possible, even if they need to be conceptual rather than physical (Figure). In these areas, information should be provided regarding the 1) prevention of infection and injury and 2) location of hand-washing facilities and instructions for visitors to wash their hands upon exiting.
Nonanimal Areas Nonanimal areas are areas in which animals are not permitted, with the exception of service animals.
Animal Care and ManagementThe risk for disease or injuries from animal contacts can be reduced by carefully managing the specific animals used for such contacts. These recommendations should be considered for management of animals in contact with the public.
NASPHV recognizes the benefits of human-animal contact. However, infectious diseases, rabies exposures, injuries, and other human health problems have occurred in animal contact settings secondary to human-animal contact. These incidents have substantial medical, public health, legal, and economic effects. The recommendation to wash hands is the single most important prevention step for reducing the risk for disease transmission. The standardized recommendations in this report should be used by public health officials, veterinarians, venue operators, animal exhibitors, and other persons concerned with disease control to minimize risks associated with animals in public settings. References
* M. Eidson, DVM, New York State Department of Health, personal communication, 2003. J.B. Bender, DVM, University of Minnesota, personal communication, 2003. M.T. Jay-Russell, DVM, California Department of Health, personal communication, 2003. G.L. Swinger, DVM, Tennessee Department of Health, personal communication, 2003. National Association of State Public Health Veterinarians, Inc., Committee Millicent Eidson, DVM, Cochair; Jeffrey B. Bender, DVM,
CoChair; Carina Blackmore, DVM, PhD; James J. Kazmierczak, DVM, James H.
Wright, DVM.
Box 1 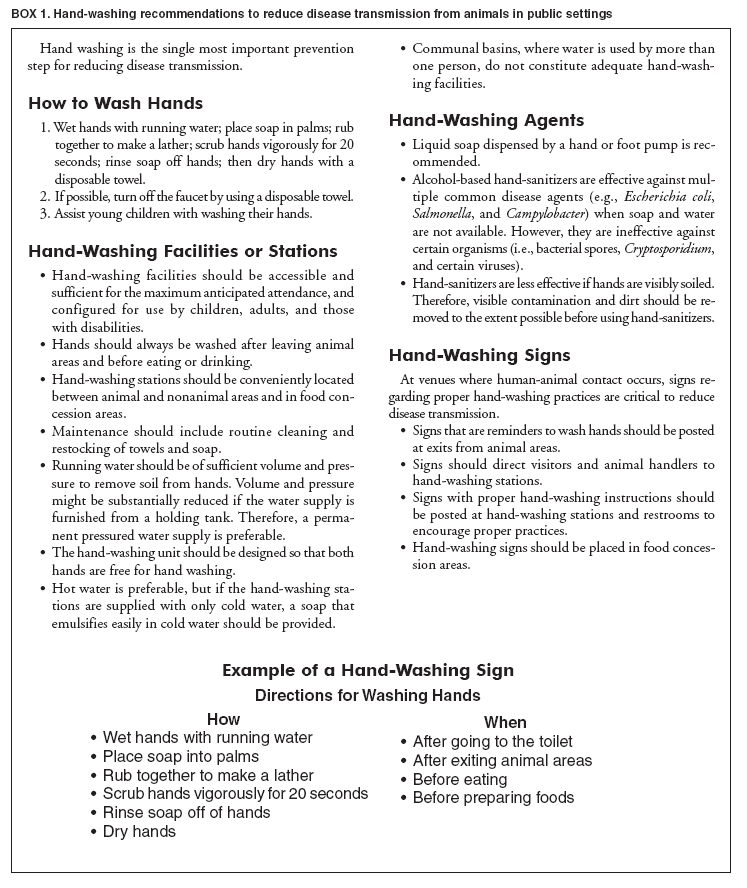 Return to top. Box 2 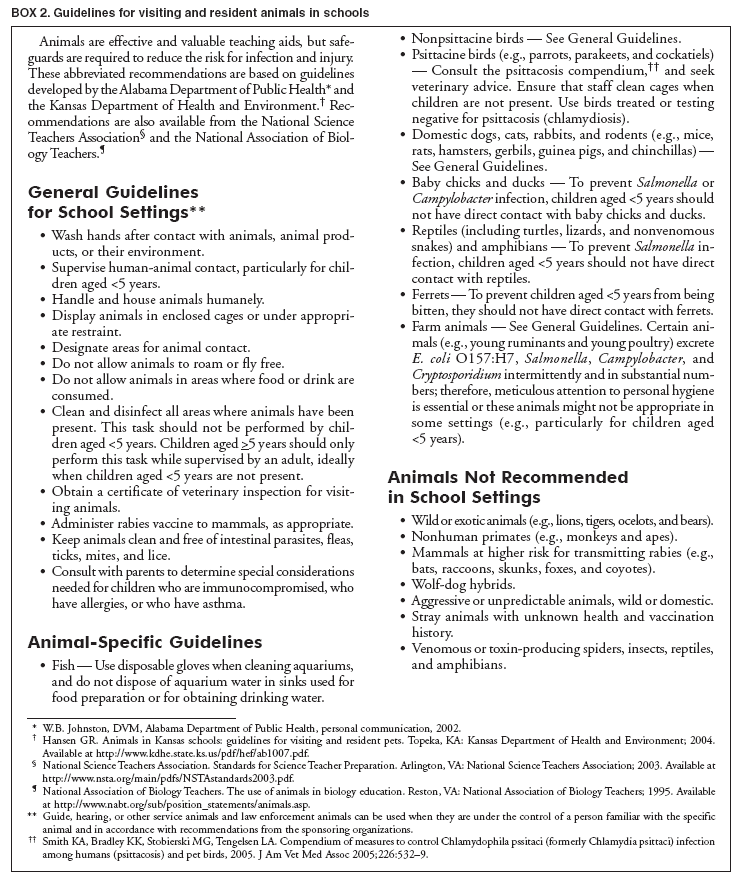 Return to top. Figure 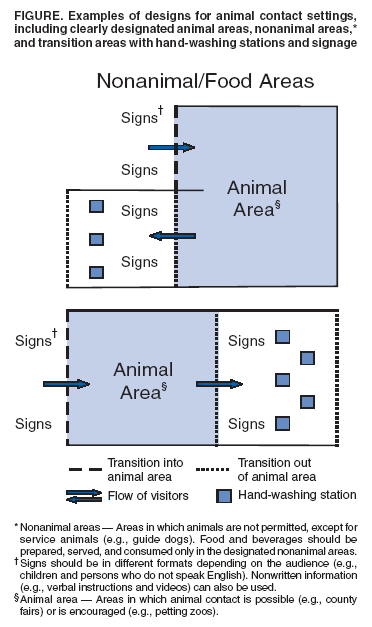 Return to top.
All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Page converted: 3/18/2005 |
|||||||||
This page last reviewed 3/18/2005
|