 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
| Recommendations and Reports |
| March 28, 2003 / 52(RR06);1-8 |
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Key Clinical Activities for Quality Asthma CareRecommendations of the National Asthma Education and Prevention ProgramPrepared by The material in this report originated in the National Center for Environmental Health, Richard J. Jackson, M.D., Director; Division of Environmental Hazards and Health Effects, Michael A. McGeehin, Ph.D., Director. Summary In 1997, the National Asthma Education and Prevention Program (NAEPP), coordinated by the National Heart, Lung, and Blood Institute, published the second Expert Panel Report (EPR-2): Guidelines for the Diagnosis and Management of Asthma (National Heart, Lung, and Blood Institute, National Asthma Education and Prevention Program. Expert Panel Report 2: Guidelines for the diagnosis and management of asthma. Bethesda MD: US Department of Health and Human Services, National Institutes of Health, 1997; publication no. 97-4051. Available at http://www.nhlbi.nih.gov/guidelines/asthma/asthgdln.pdf) . Subsequently, the NAEPP Expert Panel identified key questions regarding asthma management that were submitted to an evidence practice center of the Agency for Healthcare Research and Quality to conduct a systematic review of the evidence. The resulting evidence report was used by the Expert Panel to update recommendations for clinical practice on selected topics. These recommendations (EPR--Update 2002) were published in 2002. (National Heart, Lung, and Blood Institute, National Asthma Education and Prevention Program. Guidelines for the diagnosis and management of asthma---update on selected topics 2002. J Allergy Clin Immunol 2002;110[November 2002, part 2]. Available at http://www.nhlbi.nih.gov/guidelines/asthma/index.htm) . To improve the implementation of these guidelines, a working group of the Professional Education Subcommittee of the NAEPP extracted key clinical activities that should be considered as essential for quality asthma care in accordance with the EPR-2 guidelines and the EPR--Update 2002. The purpose was to develop a report that would help purchasers and planners of health care define the activities that are important to quality asthma care, particularly in reducing symptoms and preventing exacerbations, and subsequently reducing the overall national burden of illness and death from asthma. This report is intended to help employer health benefits managers and other health-care planners make decisions regarding delivery of health care for persons with asthma. Although this report is based on information directed to clinicians; it is not intended to substitute for recommended clinical practices for caring for persons with asthma, nor is it intended to replace the clinical decision-making required to meet individual patient needs. Readers are referred to the EPR-2 for the full asthma guidelines regarding diagnosis and management of asthma or to the abstracted Practical Guide (National Heart, Lung, and Blood Institute, National Asthma Education and Prevention Program. Practical guide for the diagnosis and management of asthma. Bethesda MD: US Department of Health and Human Services, National Institutes of Health, 1997; publication no. 97-4053. Available at http://www.nhlbi.nih.gov/health/prof/lung/asthma/practgde.htm) and to the EPR--Update 2002. The 1997 EPR-2 guidelines and EPR--Update 2002 were derived from a consensus of leading asthma researchers from academic, clinical, federal, and voluntary institutions and based on scientific evidence supported by the literature. The 10 key activities highlighted here correspond to the four recommended-as-essential components of asthma management: assessment and monitoring, control of factors contributing to asthma severity, pharmacotherapy, and education for a partnership in care. The key clinical activities are not intended for acute or hospital management of patients with asthma but rather for the preventive aspects of managing asthma long term. This report was developed as a collaborative activity between CDC and the NAEPP. BackgroundThe National Asthma Education and Prevention Program (NAEPP), administered and coordinated by the National Heart, Lung, and Blood Institute, began developing a consensus set of science-based guidelines for diagnosis and management of asthma shortly after its establishment in 1989. With wide participation of asthma specialists from academia, research, and clinical care, as well as representatives from voluntary health organizations and federal agencies, the first Expert Panel Report: Guidelines for the Diagnosis and Management of Asthma was produced in 1991 (1); a revision, the EPR-2, was published in 1997 (2), and an update to the EPR-2 was published in 2002 (3). The EPR-2 and EPR--Update 2002 comprise the prevailing science-based consensus concerning accurate information for health-care providers regarding asthma diagnosis and management. The EPR-2 has been disseminated nationwide and abstracted into a practical guide, a best practices pediatric guide, and a pocket guideline. However, although these asthma care principles have been widely endorsed, they have not been adequately applied (4--8). This report is a companion to the NAEPP Expert Panel Reports. It identifies a core set of 10 key clinical activities essential for ensuring that health care delivered to patients with asthma emphasizes the prevention aspect of care and addresses the components of care recommended in the Expert Panel Reports. The action steps listed for each key clinical activity suggest specific ways to accomplish the respective activity. The process of developing a core set of key clinical activities involved a detailed review of the EPR-2 guidelines and input from persons researching their implementation (1--3, 9--11). These activities were identified in the context of the currently proposed asthma-specific measures for managed care (12), as well as the national health goals of Healthy People 2010 (13) (Box 1) and the strategic plan of the U.S. Department of Health and Human Services (DHHS), Action Against Asthma (14). These reports complement each other to help health-care professionals, policymakers, patients, and the public work together to improve asthma care for the overall population and reduce asthma-related morbidity and mortality. Essential Components of Care and Associated Key Clinical ActivitiesThe four essential components of asthma management---assessment and monitoring, controlling factors contributing to asthma severity, pharmacotherapy, and education for partnership in care---are distilled from the NAEPP EPR-2 Guidelines for the Diagnosis and Management of Asthma (Table 1). In addition, 10 key clinical activities are described and listed, each according to the essential component it represents. Action steps are suggested to help accomplish each of the clinical activities. The intent of this report is to help employer health benefits managers and health-care planners make decisions regarding delivery of quality health care for persons with asthma. Assessment and Monitoring
Key Clinical Activity 1. After a person seeks medical care for symptoms that suggest asthma, the diagnosis of asthma should be clearly established and the baseline severity of the disease classified to help establish the recommended course of therapy. For symptomatic adults and children aged >5 years who can perform spirometry, asthma can be diagnosed after a medical history and physical examination documenting an episodic pattern of respiratory symptoms and from spirometry that indicates partially reversible airflow obstruction (>12% increase and 200 mL in forced expiratory volume in 1 second [FEV1] after inhaling a short-acting bronchodilator or receiving a short [2--3 week] course of oral corticosteroids). Alternative diagnoses of symptoms that suggest asthma, including conditions affecting the upper and lower airways (e.g., upper airway obstruction/foreign body, bronchitis, pneumonia/bronchiolitis, chronic obstructive pulmonary disease, tumor/neoplasm, pulmonary embolism, congestive heart failure, vocal cord dysfunction, or viral lower respiratory tract infection) should be ruled out and may require additional tests. For the patient with a probable diagnosis of asthma after initial evaluation (i.e., symptomatic with normal spirometry and no alternative diagnosis), presumptive treatment may be necessary to reach a final diagnosis. Referral to a specialist (see Key Clinical Activity 4) may be necessary if the diagnosis is in doubt, other conditions are aggravating the asthma, or the contribution of occupational or environmental exposures needs to be confirmed. For infants and children aged <5 years, the diagnostic steps are the same except that spirometry, the most objective measure of lung function, is not feasible for this age group. Therefore, young children with asthma symptoms should be treated as having suspected asthma once alternative diagnoses are ruled out. Their medical histories and physical examinations should be expanded to look for factors associated with the development of chronic persistent asthma: more than three episodes of wheezing in the past year that lasted more than 1 day and affected sleep, AND parental history of asthma or physician-diagnosed atopic dermatitis, or two of the following: physician-diagnosed allergic rhinitis, wheezing apart from colds, or peripheral blood eosinophilia (15). Over time, the diagnosis may become apparent or referral to a specialist may be necessary to perform additional testing to exclude other diagnoses. Many children aged <6 years who wheeze with respiratory tract infections respond well to asthma therapy (16) even though the diagnosis may be unconfirmed until persistence or recurrence of signs and symptoms is established. Approximately one third of children who wheeze with respiratory infections develop asthma that persists after age 6 (17).
Key Clinical Activity 2. Because asthma is characterized by varying signs and symptoms, for appropriate treatment and monitoring, the severity of such signs and symptoms must be classified at the initial and all subsequent visits. Initially and before treatment has been optimized, clinical signs, symptoms, and peak flow monitoring or spirometry are used to classify severity (Table 2) (Box 2). After the patient's asthma is stable, severity is subsequently classified according to the level of medication required to maintain treatment goals (Table 3). Health-care providers should have the knowledge, equipment, staff or access to needed resources to aid in classification and proper management of all patients with asthma.
Key Clinical Activity 3. Patients with asthma experience varying symptoms and severity because of the nature of asthma, their exposure to environmental allergens or irritants, or insufficient adherence to their medication regimen. For these reasons, they require adjustments in therapy and regular follow-up visits. The first follow-up visit should be scheduled within the month after initial diagnosis. Routine visits thereafter should be scheduled every 1--6 months, depending on the severity of asthma and the patient's ability to maintain control of symptoms. Routine care includes clinical assessment of airway function over time. Spirometry is recommended at the initial assessment and at least every 1--2 years after treatment is initiated and the symptoms and peak expiratory flow have stabilized. Spirometry as a monitoring measure may be performed more frequently, if indicated, on the basis of severity of symptoms and the disease's lack of response to treatment. At all follow-up visits, the physician reviews the patient's medication use and management plan, including self-monitoring records. Also at each visit, the physician should assess the patient's self-management skills, including correct technique for use of inhalers, spacers, and peak flow meters, as applicable. See Education for Partnership in Care (Key Clinical Activities 9 and 10) for more detailed discussion regarding the asthma management plan and patient self-management. All patients should have access to and be instructed in the use of devices needed to administer medication or monitor their asthma (e.g., inhalers, spacers, nebulizers, and peak flow meters [PFMs]). Several devices may be required to ensure optimal treatment. Patients who use inhaled corticosteroids delivered by metered-dose inhalers should use a spacer to increase consistency of the dose and to minimize the possibility of local side effects. Some patients cannot easily coordinate actuation and inhalation using a metered-dose inhaler; spacers enable easier and more effective administration of medication. Spacers with face masks and nebulizers are both available for young children. PFMs are recommended for patients with moderate or severe, persistent asthma and those with a history of severe exacerbations to help them monitor their symptoms during daily management as well as their response to home treatment during an exacerbation.
Key Clinical Activity 4. Referral to an asthma specialist for consultation or comanagement is recommended in the following circumstances:
Specialty care for asthma may be provided by an allergist, pulmonologist, or other physician with expertise in asthma management. Patients undergoing specialty care may be comanaged by the referring physician or monitored by the referring physician in accordance with the specialty care physician's treatment regimen. Identifying and Controlling Factors Contributing to Asthma Severity
Key Clinical Activity 5. Environmental tobacco smoke (ETS) and house dust mite, cockroach, and cat and dog allergens can worsen asthma (or trigger asthma exacerbations) in sensitized and exposed persons (18). Irritant or allergen sensitivity can be determined by the patient's exposure and symptom history and confirmed with skin or blood testing. Allergy testing for perennial indoor allergens is recommended for persons with persistent asthma who are taking daily medications. After sensitivity is determined, avoidance of the trigger is recommended, and allergen abatement might be indicated. Ways to reduce allergen and irritant exposure should be reviewed and agreement sought with the patient to initiate measures. Examples of trigger avoidance include using dust mite impermeable pillow and mattress covers, removing furry pets, and taking measures to eliminate cockroaches (Box 3). No patient with asthma should smoke or be exposed to ETS. Physicians should review smoking status at the initial visit and all subsequent visits and, if patients smoke or are regularly exposed to ETS, should encourage and refer them to stop smoking. Exercise-induced bronchoconstriction describes the transient narrowing of airways associated with physical exertion in persons with asthma (17). Exercise-induced bronchoconstriction may be prevented with optimal long-term control of asthma. If the patient remains symptomatic during exercise, specific medications can be taken before exercise to prevent exercise-induced bronchoconstriction.
Key Clinical Activity 6. Allergic rhinitis, sinusitis, gastroesophageal reflux, and sensitivity to certain medicines, including aspirin, nonsteroidal antiinflammatory drugs (NSAIDs), and beta blockers, can exacerbate asthma symptoms. Health-care providers should evaluate their asthma patients for these conditions and inquire about their medications, especially when asthma symptoms persist or worsen despite medication adjustments. Health-care providers should provide annual influenza vaccinations to patients with persistent asthma to prevent a respiratory infection that can exacerbate asthma. However, patients who are clinically allergic to egg should not get the vaccine. Pharmacotherapy
Key Clinical Activity 7. Current evidence indicates that daily long-term control medications are necessary to prevent exacerbations and chronic symptoms for all patients with persistent asthma, whether the persistent asthma is mild, moderate, or severe. Inhaled corticosteroids are preferred because they are the most effective antiinflammatory medication available for treating the underlying inflammation characteristic of persistent asthma. For patients with mild persistent asthma, other long-term medications---cromolyn, leukotriene modifiers, nedocromil, and theophylline---are available but have not been demonstrated to be as effective as inhaled corticosteroids. Patients with moderate or severe disease usually require additional medication combined with inhaled corticosteroids for daily long-term control. All patients with asthma require a short-acting bronchodilator medication for managing acute symptoms or exacerbations when they occur; severe exacerbations require the addition of systemic (oral) corticosteroids to treat the increased inflammation present (see EPR-2 for additional information about managing exacerbations of asthma). The dosage and type of medications are crucial because asthma treatment is adjusted according to the level of asthma severity. Once therapy goals are achieved, a gradual reduction in treatment should be carefully undertaken to identify the minimum dose required to maintain control (Table 3). On the basis of the severity of asthma in an individual patient, various medication delivery and monitoring devices may be necessary (see Key Clinical Activity 3 for discussion of spacers/holding chambers, nebulizers, and peak flow and symptom monitoring).
Key Clinical Activity 8. Patients whose need increases for short-acting inhaled ß2-agonist to control serious day and night symptoms probably have inadequately controlled asthma. Although patients may need short-acting inhaled ß2-agonist during upper respiratory viral infections and exercise-induced bronchoconstriction, using more than one canister of short-acting ß2-agonist drugs per month is usually considered above expected use. At every patient visit, the health-care provider should review ß2-agonist medication use, including the patient's understanding of the dosage instructions, inhaler technique, and reasons for increased use. For patients using more ß2-agonist drugs than expected, daily long-term control therapy should be increased as needed, either by initiating or increasing daily long-term control therapy (Table 3). Education for Partnership in Care
Key Clinical Activity 9. As part of the overall management of patients with asthma, the health-care provider, in consultation with the patient or the parent or guardian of a child with asthma, should develop a written plan as part of educating patients regarding self management, especially for patients with moderate or severe persistent asthma and those with a history of severe exacerbation. The National Heart, Lung, and Blood Institute provides more specific advice on asthma management plans, emphasizing the provider/patient partnership (available at http://www.nhlbi.nih.gov/health/public/lung/asthma/asthma.htm#plan). Writing the management plan helps clarify expectations for treatment (Box 4) and provides patients with an easy reference for remembering how to manage their asthma. The action plan should include written instructions on recognizing symptoms and signs of worsening asthma; taking appropriate medicines (type, dose, and frequency); recognizing when to seek medical care; and monitoring response to medications. Symptom-based plans may be equally effective as plans based on peak flow monitoring, although some patient preferences and circumstances (e.g., inability to recognize or report signs and symptoms of worsening asthma) may warrant a choice of peak flow monitoring. The management plan should be reviewed and adjusted, as needed, at every visit. For children, a copy of the plan should be given to each care giver and the child's school.
Key Clinical Activity 10. Asthma education is essential for successful management of the disease. Effective asthma education is developed in a patient--provider partnership, tailored to the individual patient's needs relative to cultural or ethnic beliefs and practices. At a minimum, competent asthma education enlists and encourages family support, includes instructions on self-management skills (Box 5), and is integrated with routine ongoing care. It is provided, either as group or individual patient programs, to all patients and parents/guardians of children who have had a diagnosis of asthma. A patient's ability to take asthma medications is a necessary skill of self-management. Patients and parents/guardians of children with asthma need to know the rationale behind daily long-term and quick-relief medications, how to take medications correctly, and how to adjust the dosage if asthma symptoms occur. Instructions and verification on the proper use of any medication delivery devices and PFMs (for patients with moderate or severe persistent asthma) should be provided at the initial and each subsequent visit. Instruction should include how to interpret peak flow results and take action according to the asthma management plan. To help patients avoid or control environmental factors that worsen their asthma, education should focus first on identifying simple measures. Once the patient notices improved asthma control, more complicated or extensive measures can be undertaken. Including members of the family in these discussions may be helpful because implementing avoidance and control measures often affects all family members. This is especially true with ETS education. ConclusionThe 10 key clinical activities for quality asthma care, derived from the NAEPP EPR-2 and EPR-Update 2002, offer guidance for health-care managers and planners in making decisions regarding the resources necessary to ensure quality health care for persons with asthma. Managers and planners using these guides should understand the resources needed for appropriate diagnosis and treatment of asthma and the corresponding clinical activities recommended to ensure proper care and control of asthma. Action steps listed for each activity suggest specific ways to accomplish the respective activities. Adoption of the key clinical activities will lead to more appropriate health care for persons with asthma. References
National Asthma Education and Prevention Program (NAEPP) Chairperson: William Storms, M.D., American College of Allergy, Asthma, and Immunology, Colorado Springs, Colorado.
Members of the Document Development Working Group American Academy of Family Physicians, Barbara Yawn, M.D., Rochester, Minnesota; American College of Allergy, Asthma and Immunology, William Storms, M.D., Colorado Springs, Colorado; American College of Chest Physicians, John P. Mitchell, M.D., Davis, California; American Society of Health System Pharmacists, Leslie Hendeles, Pharm.D., Gainesville, Florida; Centers for Disease Control and Prevention, Stephen Redd, M.D., Seymour Williams, M.D., Atlanta, Georgia; National Institutes of Health, Diana Schmidt, M.P.H., Virginia Taggart, M.P.H., Bethesda, Maryland; Society for Academic Emergency Medicine, Carlos Carmago, Boston, Massachusetts; Environmental Protection Agency, Tracey Mitchell, Washington, DC. Table 1 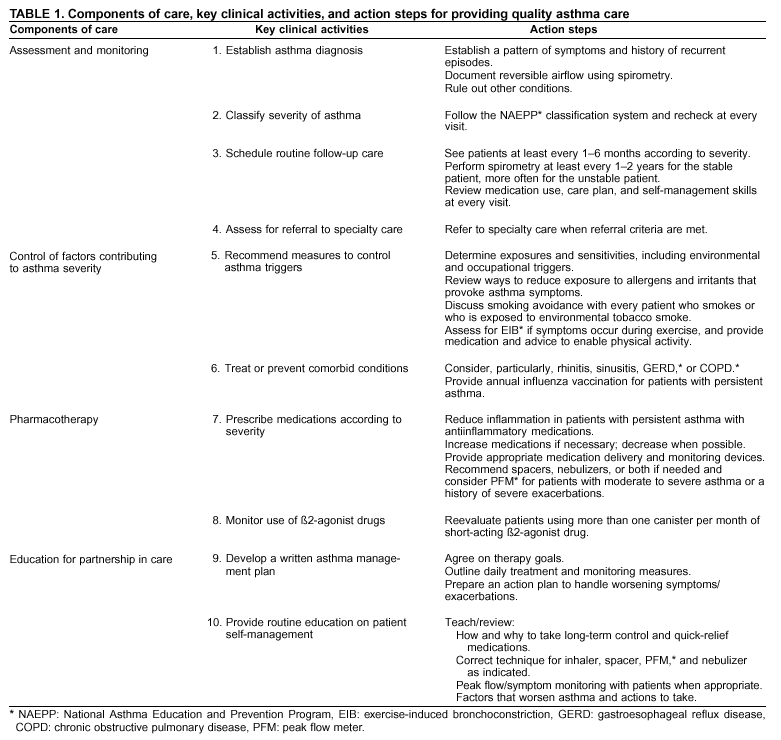 Return to top. Box 1 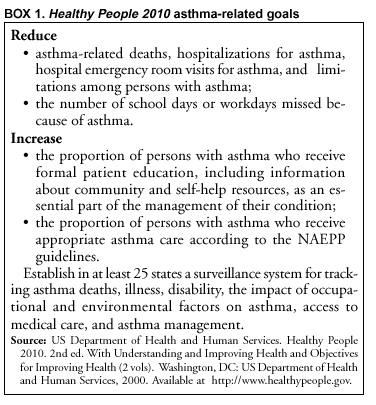 Return to top. Table 2 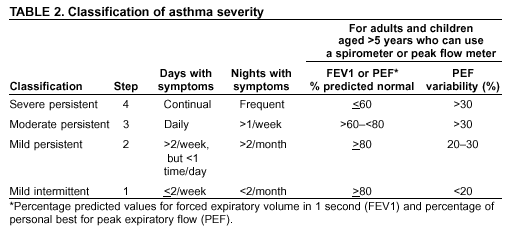 Return to top. Box 2 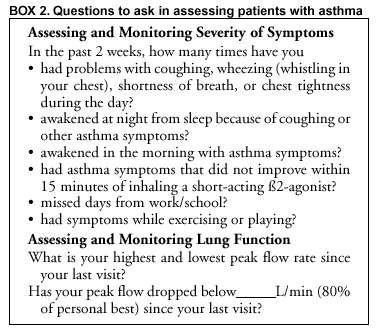 Return to top. Table 3 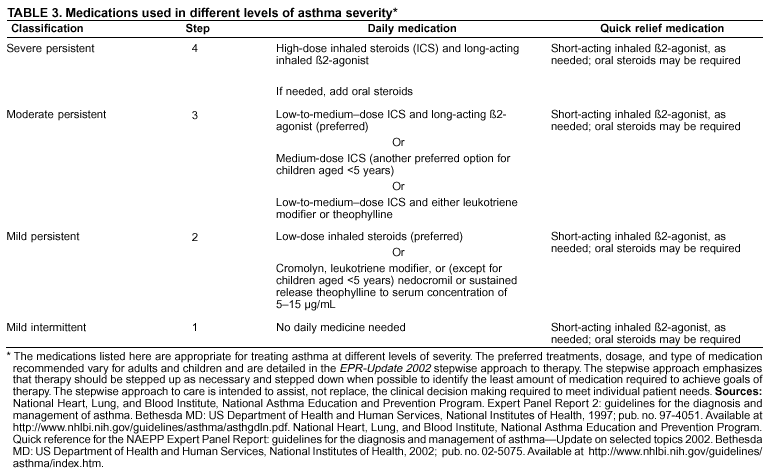 Return to top. Box 3 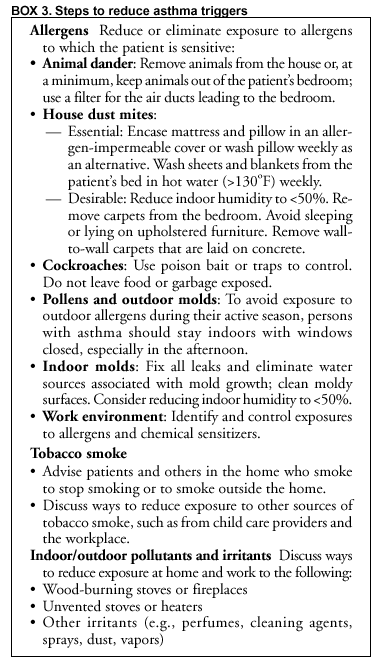 Return to top. Box 4 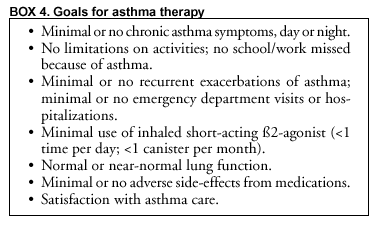 Return to top. Box 5 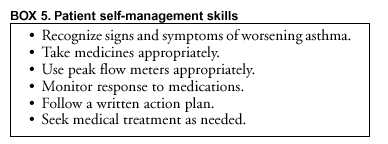 Return to top.
Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Page converted: 3/12/2003 |
|||||||||
This page last reviewed 3/12/2003
|