Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail.
Human Rabies --- Michigan, 2009
Weekly
April 15, 2011 / 60(14);437-440On November 9, 2009, a Michigan hospital informed CDC of suspected rabies in a man aged 55 years. The patient reportedly had awakened with a bat on his arm 9 months earlier but had not sought medical evaluation. He went to a local emergency department (ED) on October 30 and soon after was hospitalized; he died 12 days later. On November 14, CDC confirmed infection with a rabies virus variant that commonly infects the silver-haired bat (Lasionycteris noctivagans) (Figure). This report summarizes the patient's clinical course and the associated public health investigation. The report highlights the importance of public awareness of rabies, particularly among persons who might be at risk for wildlife exposures. Persons who experience contact with a bat and cannot confidently rule out a bite or scratch should seek prompt medical attention.
Case Report
On October 30, the man went to a local ED after 10 days of pain and progressive numbness in the left hand and arm and pain in his lower neck and upper back. The patient had sought treatment for these symptoms from a chiropractor several times during the preceding 6 days. Although the back pain had improved, the numbness and tingling had worsened, and he was experiencing weakness in his left hand and arm. A neurologic examination revealed normal strength and sensation of his lower extremities. His right arm showed normal strength, but the left hand showed no grip, and the patient could only lift his left arm a few inches. The patient was afebrile, and his blood pressure was normal when he arrived at the ED. A complete blood count and routine chemistries were normal except for an elevated white blood cell count of 15,300/µL (normal: 3,600--10,000/µL) and elevated glucose of 155 mg/dL (normal: 70--99 mg/dL). A computed tomography scan of the brain without contrast revealed a cavernous sinus larger on the left than on the right and an area of slightly decreased density in the right basal ganglion and paraventricular areas.
During the ED evaluation, the patient's breathing became labored, and he had difficulty with respiratory secretions. He was placed on ventilation and transferred to a nearby tertiary-care facility. At the time of intubation, the anesthesiologist noted that the procedure was easy to perform because of lack of muscle tone in the patient's pharynx.
On admission to the tertiary-care facility, respiratory failure secondary to cerebral vascular accident or acute idiopathic demyelinating polyradiculoneuropathy (AIDP or Guillain-Barré syndrome) were the chief diagnoses considered. Findings from magnetic resonance imaging were unremarkable. Electromyography showed mild decreased conduction velocities and multiple absent F waves. Thereafter, AIDP was suspected, and intravenous immunoglobulin therapy was begun. The patient's sedation was lightened to conduct physical examinations.
During the first 2 days of hospitalization, the patient experienced progressive weakness, initially on the left side. He was able to respond to verbal commands and, according to the neurologist who evaluated him, his random eye movements were normal. On November 1, the patient's mental status appeared to improve, as sedation was lightened with the hope of removing him from the ventilator. However, over the next few days, his upper extremity weakness progressed to involve the right side, and lower extremity weakness was noted, demonstrating areflexia and a lack of response to plantar stimulation. Some nystagmus on far horizontal gaze to either side also was noted as a new development. On November 3, the patient became quadriplegic but could move his eyes to the right and left on request. Analysis of his cerebrospinal fluid (CSF) revealed several abnormal values: protein of 109 mg/dL (normal: 10--55 mg/dL); glucose of 92 mg/dL (normal: 45--75 mg/dL); and a white blood cell count of 243 cells/µL (normal: <5 cells/µL) with a differential of 80% lymphocytes, 18% monocytes, and 2% segmented neutrophils. A Gram stain and culture were negative.
On November 4, the patient had an acute change in his neurologic status, including twitching of the left foot, more marked nystagmus, and slightly asymmetric pupils. Based on the results of the CSF analysis, the working diagnosis was changed to meningoencephalitis, and an infectious disease consultation was sought. The CSF was further analyzed for Borrelia burgdoferi and the following viruses: West Nile, St. Louis encephalitis, California Group, Eastern equine encephalitis, Western equine encephalitis, measles, mumps, herpes simplex virus 1 and 2, enteroviruses, varicella-zoster, cytomegalovirus, lymphocytic choriomeningitis virus, adenovirus, and influenza. All tests were negative. Antiviral treatment with acyclovir was begun. The patient's electroencephalogram showed marked deterioration from previous studies, indicating severe encephalopathy.
On November 4, the infectious disease physician asked the patient's wife about any animal exposure history. The couple lived in a rural area. In the past, the patient had trapped wildlife for pelts and raised orphaned animals, but he had not engaged in these activities in the past year. The wife had no knowledge of any recent animal bites the patient might have received.
On November 8, another relative recounted an incident that had occurred approximately 9 months before onset of illness. The patient had told the relative about waking one night to a bat crawling on his arm. The relative did not know whether the patient had been bitten by the bat. The bat had been killed and discarded, and the patient did not seek medical care for the incident.
The patient's condition, characterized as complete flaccid paralysis, coma, and flat electroencephalogram, remained unchanged. On November 11, the patient's family elected to withdraw life support, and the patient died shortly afterward.
Public Health Investigation
After obtaining the bat exposure history, the infectious disease physician contacted CDC on November 9 to discuss a diagnosis of rabies. The Michigan Department of Community Health Bureau of Laboratories also was contacted by the hospital regarding specimen collection. Serum, CSF, saliva, and nuchal skin biopsy specimens were collected and sent to CDC on November 10.
On November 12, CDC reported detecting no rabies virus antigens in the skin biopsy by direct fluorescent antibody test, nor amplicons in the saliva or skin biopsy specimens by reverse transcription--polymerase chain reaction. However, rabies virus antibodies were detected by indirect fluorescent antibody test and rapid fluorescent focus inhibition tests on serum and CSF. Both health-care facilities involved in the patient's care were informed of the results, as well as the local health departments covering those jurisdictions. The patient's family was informed and gave permission for a brain autopsy. On November 13, brain specimens were collected and shipped overnight to CDC. On November 14, CDC reported that rabies virus antigens were detected in the brain by direct fluorescent antibody test. Sequence analysis of the nucleoprotein gene was consistent with a rabies virus variant found in L. noctivagans in the United States.
A total of 14 family members and friends were interviewed by the local health department regarding exposure to the patient's saliva during the 2 weeks before his illness onset and during his hospitalization. Eleven family members received rabies postexposure prophylaxis (PEP) at the advice of the local health department because of possible exposure to saliva through shared glasses or cups; an additional person also received PEP, although it was not recommended. Of 180 health-care providers from the two health-care facilities who were assessed for potential exposure to rabies virus based on their likelihood of saliva contact, six received rabies PEP.
Reported by
K Signs, DVM, MG Stobierski, DVM, Michigan Dept of Community Health. CE Rupprecht, VMD, PhD, Div of High-Consequence Pathogens and Pathology, National Center for Emerging and Zoonotic Infectious Diseases; K Robertson, DVM,* EIS Officer, CDC. *Corresponding contributor: Kis L. Robertson, CDC, 410-767-0202, krobertson@cdc.gov.
Editorial Note
The case described in this report underscores the importance of prompt medical care after bat encounters during which undetected bites might have occurred. Such encounters include being in close proximity to a bat while asleep or being heavily intoxicated or otherwise impaired (1). Although the bat described in the elicited exposure history was not tested for rabies, sequence analysis of the virus associated with the patient's illness corroborates suspicion that a bat was the source of the patient's infection. Reports that medical care was not sought following the reported incident suggest that, regardless of the actual source of transmission, possible factors in the patient's illness were a lack of rabies awareness or a low perception of risk.
Rabies is a viral disease of the central nervous system that is transmitted when broken skin or a mucous membrane is contaminated with saliva from an infectious mammal. Typically, after a 1--3 month incubation period, an acute, rapidly progressive encephalomyelitis develops, and death of the patient occurs within 20 days (2). The disease is preventable if exposure to the virus is promptly followed by wound cleaning, administration of rabies immune globulin, and rabies vaccination (3). Clinical signs of rabies most often are associated with the encephalitic form of the disease and include hydrophobia, muscle spasms, and altered mental status. The patient described in this report exhibited characteristic signs of paralytic rabies, a less common presentation that manifests as flaccid paralysis relatively early in the illness course.
During 1980--2009, a total of 39 (91%) of the 43 reported cases of human rabies acquired in the United States were associated with bat exposures* (2,4--7). Median age of these 39 patients was 32 years, with a range of 4 to 82 years; 28 (72%) were male. Wide differences in median age are evident when cases are compared by sex. The median age of the 11 female patients was 14 years (range: 4--42 years), and only two patients were aged ≥40 years. In contrast, the median age of the 28 male patients was 46 years (range: 10--82 years), with 16 patients aged ≥40 years (2,4--7). The difference in age distribution between male and female patients is statistically significant (p = 0.001, by the Wilcoxon rank sum test) and appears to derive from a preponderance of older male patients; the incidence in patients aged <40 years does not appear to differ significantly by sex (11 males and 8 females, respectively†). Explanations for this disparity are unclear, but it might be attributable, in part, to adult males spending more time engaged in outdoor activities that increase their proximity to bats and other wildlife (8). Studies also have shown that health-related risk perception and awareness is lower in men than in women (9,10). In countries where dogs are most often implicated in cases of human rabies, patients are disproportionately aged <15 years.
Education is an important prevention strategy against rabies and should be directed particularly toward groups most likely to have wildlife encounters. Messages should emphasize appropriate actions to take after possible animal bites, including contacting local authorities for guidance on how to safely capture and submit animals for rabies diagnosis (1). In the absence of a negative animal rabies diagnostic result, persons who come in contact with a bat and cannot confidently exclude a bite or scratch should be advised to seek medical attention. After the onset of symptoms, the clinical course of rabies is almost invariably fatal.
Acknowledgments
This report is based, in part, on contributions by District Health Dept No. 10, Grand Traverse County Health Dept; D Martin, MD, K Speirs, DO, D Ochs, MD, L Gottfried, MD, B Schreibe, Munson Medical Center, Traverse City, Michigan. J Ellison, R Franka, DVM, PhD, I Kuzmin, MD, PhD, L Orciari, MS, A Velasco, PhD, and P Yager, Div of High-Consequence Pathogens and Pathology, National Center for Emerging Zoonotic and Infectious Diseases, CDC.
References
- CDC. Human rabies prevention---United States, 2008. Recommendations of the Advisory Committee on Immunization Practices. MMWR 2008;57(No. RR-3).
- Noah DL, Drenzek CL, Smith JS, et al. Epidemiology of human rabies in the United States, 1980 to 1996. Ann Intern Med 1998;128:922--30.
- CDC. Use of a reduced (4-dose) vaccine schedule for postexposure prophylaxis to prevent human rabies: recommendations of the Advisory Committee on Immunization Practices. MMWR 2010;59(No. RR-2).
- De Serres G, Dallaire F, Côte, Skowronski DM. Bat rabies in the United States and Canada from 1950 through 2007: human cases with and without bat contact. Clin Infect Dis 2008;46:1329--37.
- CDC. Human rabies---Missouri, 2008. MMWR 2009;58:1207--9.
- CDC. Presumptive abortive human rabies---Texas, 2009. MMWR 2010;59:185--90.
- CDC. Human rabies---Kentucky/Indiana, 2009. MMWR 2010;59:393--6.
- Kwok RK, Linet MS, Chodick G, et al. Simplified categorization of outdoor activities for male and female U.S. indoor workers---a feasibility study to improve assessment of ultraviolet radiation exposures in epidemiologic study questionnaires. Photochem Photobiol 2009;85:45--9.
- Näslund GK. Relationships between health behavior, knowledge, and beliefs among Swedish blue-collar workers. Scand J Soc Med 1997;25:100--10.
- Gustafson PE. Gender differences in risk perception: theoretical and methodological perspectives. Risk Anal 1998;18:805--11.
* Not including four cases that occurred in 2004 associated with transplanted tissue from an infected human donor (4).
† Age was not documented for one female and one male patient.
What is already known about this topic?
During 1980--2009, a total of 39 (91%) of the 43 reported cases of human rabies acquired in the United States via animals were associated with bat exposures.
What is added by this report?
In 2009, a Michigan resident died from rabies. The man had contact with a bat while sleeping but did not report a bite and did not seek medical care until 9 months later, after symptoms had developed.
What are the implications for public health practice?
The public should be aware of the risk for rabies associated with bats and should take appropriate actions after exposure, including contacting local authorities for guidance on how to safely capture and submit a bat for rabies diagnosis and consulting a physician or state or local health department for advice regarding rabies postexposure prophylaxis.
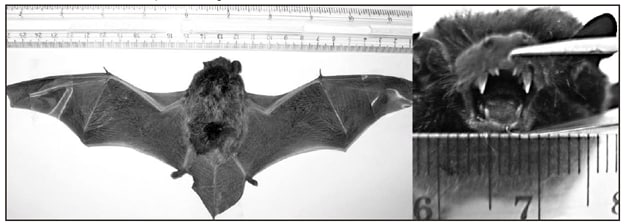
Photos/J. Ellison, CDC
Alternate Text: The figure above shows a silver-haired bat (Lasionycteris noctivagans).
Use of trade names and commercial sources is for identification only and does not imply endorsement by the U.S. Department of
Health and Human Services.
References to non-CDC sites on the Internet are
provided as a service to MMWR readers and do not constitute or imply
endorsement of these organizations or their programs by CDC or the U.S.
Department of Health and Human Services. CDC is not responsible for the content
of pages found at these sites. URL addresses listed in MMWR were current as of
the date of publication.
All MMWR HTML versions of articles are electronic conversions from typeset documents.
This conversion might result in character translation or format errors in the HTML version.
Users are referred to the electronic PDF version (http://www.cdc.gov/mmwr)
and/or the original MMWR paper copy for printable versions of official text, figures, and tables.
An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S.
Government Printing Office (GPO), Washington, DC 20402-9371;
telephone: (202) 512-1800. Contact GPO for current prices.
**Questions or messages regarding errors in formatting should be addressed to
mmwrq@cdc.gov.


