 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
| Weekly |
| October 19, 2007 / 56(41);Q1-Q4 |
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Recommended Adult Immunization Schedule --- United States, October 2007--September 2008The Advisory Committee on Immunization Practices (ACIP) annually reviews the recommended Adult Immunization Schedule to ensure that the schedule reflects current recommendations for the licensed vaccines. In June 2007, ACIP approved the Adult Immunization Schedule for October 2007--September 2008. Additional information is available as follows: schedule (in English and Spanish) at http://www.cdc.gov/vaccines/recs/schedules/adult-schedule.htm; adult vaccinations at http://www.cdc.gov/vaccines/default.htm; ACIP statements for specific vaccines at http://www.cdc.gov/vaccines/pubs/acip-list.htm; and reporting adverse events at http://www.vaers.hhs.gov or by telephone, 800-822-7967. Changes for October 2007--September 2008Age-Based Schedule (Figure 1)
Medical/Other Indications Schedule (Figure 2)
ReferenceFigure 1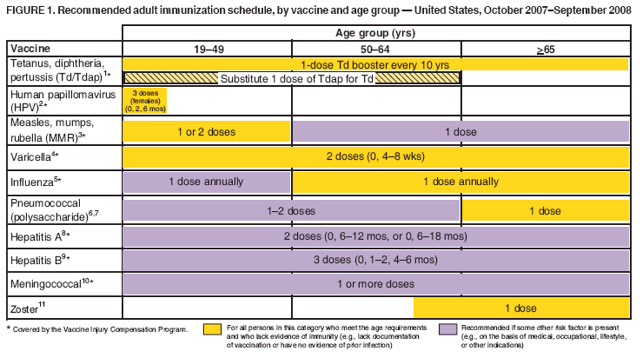 Return to top. Figure 2 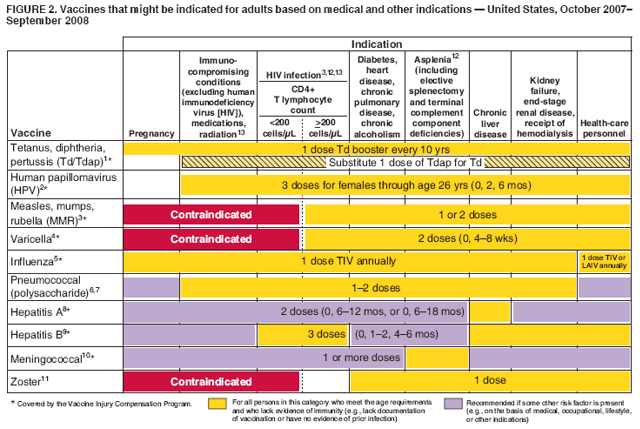 Return to top. The Recommended Adult Immunization Schedule has been approved by the Advisory Committee on Immunization Practices, the American Academy of Family Physicians, the American College of Obstetricians and Gynecologists, and the American College of Physicians. The standard MMWR footnote format has been modified for publication of this schedule. Suggested citation: Centers for Disease Control and Prevention. Recommended Adult Immunization Schedule---United States, October 2007--September 2008. MMWR 2007;56:Q1--Q4.
NOTE: These recommendations must be read along with the footnotes, which are on pages Q2--Q4 of this schedule.
1. Tetanus, diphtheria, and acellular pertussis (Td/Tdap) vaccination Tdap should replace a single dose of Td for adults aged <65 years who have not previously received a dose of Tdap. Only one of two Tdap products (Adacel® [Sanofi Pasteur]) is licensed for use in adults. Adults with uncertain histories of a complete primary vaccination series with tetanus and diphtheria toxoid--containing vaccines should begin or complete a primary vaccination series. A primary series for adults is 3 doses of tetanus and diphtheria toxoid--containing vaccines; administer the first 2 doses at least 4 weeks apart and the third dose 6--12 months after the second. However, Tdap can substitute for any one of the doses of Td in the 3-dose primary series. The booster dose of tetanus and diphtheria toxoid--containing vaccine should be administered to adults who have completed a primary series and if the last vaccination was received >10 years previously. Tdap or Td vaccine may be used, as indicated. If the person is pregnant and received the last Td vaccination >10 years previously, administer Td during the second or third trimester; if the person received the last Td vaccination in <10 years, administer Tdap during the immediate postpartum period. A one-time administration of 1 dose of Tdap with an interval as short as 2 years from a previous Td vaccination is recommended for postpartum women, close contacts of infants aged <12 months, and all health-care workers with direct patient contact. In certain situations, Td can be deferred during pregnancy and Tdap substituted in the immediate postpartum period, or Tdap can be administered instead of Td to a pregnant woman after an informed discussion with the woman. Consult the ACIP statement for recommendations for administering Td as prophylaxis in wound management. 2. Human papillomavirus (HPV) vaccination HPV vaccination is recommended for all females aged <26 years who have not completed the vaccine series. History of genital warts, abnormal Papanicolaou test, or positive HPV DNA test is not evidence of prior infection with all vaccine HPV types; HPV vaccination is still recommended for these persons. Ideally, vaccine should be administered before potential exposure to HPV through sexual activity; however, females who are sexually active should still be vaccinated. Sexually active females who have not been infected with any of the HPV vaccine types receive the full benefit of the vaccination. Vaccination is less beneficial for females who have already been infected with one or more of the HPV vaccine types. A complete series consists of 3 doses. The second dose should be administered 2 months after the first dose; the third dose should be administered 6 months after the first dose. Although HPV vaccination is not specifically recommended for females with the medical indications described in Figure 2, "Vaccines that might be indicated for adults based on medical and other indications," it is not a live-virus vaccine and can be administered. However, immune response and vaccine efficacy might be less than in persons who do not have the medical indications described or who are immunocompetent. 3. Measles, mumps, rubella (MMR) vaccination Measles component: adults born before 1957 can be considered immune to measles. Adults born during or after 1957 should receive >1 dose of MMR unless they have a medical contraindication, documentation of >1 dose, history of measles based on health-care provider diagnosis, or laboratory evidence of immunity. A second dose of MMR is recommended for adults who 1) have been recently exposed to measles or are in an outbreak setting; 2) have been previously vaccinated with killed measles vaccine; 3) have been vaccinated with an unknown type of measles vaccine during 1963--1967; 4) are students in postsecondary educational institutions; 5) work in a health-care facility; or 6) plan to travel internationally. Mumps component: adults born before 1957 can generally be considered immune to mumps. Adults born during or after 1957 should receive 1 dose of MMR unless they have a medical contraindication, history of mumps based on health-care provider diagnosis, or laboratory evidence of immunity. A second dose of MMR is recommended for adults who 1) are in an age group that is affected during a mumps outbreak; 2) are students in postsecondary educational institutions; 3) work in a health-care facility; or 4) plan to travel internationally. For unvaccinated health-care workers born before 1957 who do not have other evidence of mumps immunity, consider administering 1 dose on a routine basis and strongly consider administering a second dose during an outbreak. Rubella component: administer 1 dose of MMR vaccine to women whose rubella vaccination history is unreliable or who lack laboratory evidence of immunity. For women of childbearing age, regardless of birth year, routinely determine rubella immunity and counsel women regarding congenital rubella syndrome. Women who do not have evidence of immunity should receive MMR vaccine on completion or termination of pregnancy and before discharge from the health-care facility. 4. Varicella vaccination All adults without evidence of immunity to varicella should receive 2 doses of single-antigen varicella vaccine unless they have a medical contraindication. Special consideration should be given to those who 1) have close contact with persons at high risk for severe disease (e.g., health-care personnel and family contacts of immunocompromised persons) or 2) are at high risk for exposure or transmission (e.g., teachers; child care employees; residents and staff members of institutional settings, including correctional institutions; college students; military personnel; adolescents and adults living in households with children; nonpregnant women of childbearing age; and international travelers). Evidence of immunity to varicella in adults includes any of the following: 1) documentation of 2 doses of varicella vaccine at least 4 weeks apart; 2) U.S.-born before 1980 (although for health-care personnel and pregnant women, birth before 1980 should not be considered evidence of immunity); 3) history of varicella based on diagnosis or verification of varicella by a health-care provider (for a patient reporting a history of or presenting with an atypical case, a mild case, or both, health-care providers should seek either an epidemiologic link with a typical varicella case or to a laboratory-confirmed case or evidence of laboratory confirmation, if it was performed at the time of acute disease); 4) history of herpes zoster based on health-care provider diagnosis; or 5) laboratory evidence of immunity or laboratory confirmation of disease. Assess pregnant women for evidence of varicella immunity. Women who do not have evidence of immunity should receive the first dose of varicella vaccine upon completion or termination of pregnancy and before discharge from the health-care facility. The second dose should be administered 4--8 weeks after the first dose. 5. Influenza vaccination Medical indications: chronic disorders of the cardiovascular or pulmonary systems, including asthma; chronic metabolic diseases, including diabetes mellitus, renal or hepatic dysfunction, hemoglobinopathies, or immunosuppression (including immunosuppression caused by medications or human immunodeficiency virus [HIV]); any condition that compromises respiratory function or the handling of respiratory secretions or that can increase the risk of aspiration (e.g., cognitive dysfunction, spinal cord injury, or seizure disorder or other neuromuscular disorder); and pregnancy during the influenza season. No data exist on the risk for severe or complicated influenza disease among persons with asplenia; however, influenza is a risk factor for secondary bacterial infections that can cause severe disease among persons with asplenia. Occupational indications: health-care personnel and employees of long-term--care and assisted-living facilities. Other indications: residents of nursing homes and other long-term--care and assisted-living facilities; persons likely to transmit influenza to persons at high risk (e.g., in-home household contacts and caregivers of children aged 0--59 months, or persons of all ages with high-risk conditions); and anyone who would like to be vaccinated. Healthy, nonpregnant adults aged <49 years without high-risk medical conditions who are not contacts of severely immunocompromised persons in special care units can receive either intranasally administered live, attenuated influenza vaccine (FluMist®) or inactivated vaccine. Other persons should receive the inactivated vaccine. 6. Pneumococcal polysaccharide vaccination Medical indications: chronic pulmonary disease (excluding asthma); chronic cardiovascular diseases; diabetes mellitus; chronic liver diseases, including liver disease as a result of alcohol abuse (e.g., cirrhosis); chronic alcoholism, chronic renal failure, or nephrotic syndrome; functional or anatomic asplenia (e.g., sickle cell disease or splenectomy [if elective splenectomy is planned, vaccinate at least 2 weeks before surgery]); immunosuppressive conditions; and cochlear implants and cerebrospinal fluid leaks. Vaccinate as close to HIV diagnosis as possible. Other indications: Alaska Natives and certain American Indian populations and residents of nursing homes or other long-term--care facilities. 7. Revaccination with pneumococcal polysaccharide vaccine One-time revaccination after 5 years for persons with chronic renal failure or nephrotic syndrome; functional or anatomic asplenia (e.g., sickle cell disease or splenectomy); or immunosuppressive conditions. For persons aged >65 years, one-time revaccination if they were vaccinated >5 years previously and were aged <65 years at the time of primary vaccination. 8. Hepatitis A vaccination Medical indications: persons with chronic liver disease and persons who receive clotting factor concentrates. Behavioral indications: men who have sex with men and persons who use illegal drugs. Occupational indications: persons working with hepatitis A virus (HAV)-infected primates or with HAV in a research laboratory setting. Other indications: persons traveling to or working in countries that have high or intermediate endemicity of hepatitis A (a list of countries is available at http://wwwn.cdc.gov/travel/contentdiseases.aspx) and any person seeking protection from HAV infection. Single-antigen vaccine formulations should be administered in a 2-dose schedule at either 0 and 6--12 months (Havrix®), or 0 and 6--18 months (Vaqta®). If the combined hepatitis A and hepatitis B vaccine (Twinrix®) is used, administer 3 doses at 0, 1, and 6 months. 9. Hepatitis B vaccination Medical indications: persons with end-stage renal disease, including patients receiving hemodialysis; persons seeking evaluation or treatment for a sexually transmitted disease (STD); persons with HIV infection; and persons with chronic liver disease. Occupational indications: health-care personnel and public-safety workers who are exposed to blood or other potentially infectious body fluids. Behavioral indications: sexually active persons who are not in a long-term, mutually monogamous relationship (e.g., persons with more than one sex partner during the previous 6 months); current or recent injection-drug users; and men who have sex with men. Other indications: household contacts and sex partners of persons with chronic hepatitis B virus (HBV) infection; clients and staff members of institutions for persons with developmental disabilities; international travelers to countries with high or intermediate prevalence of chronic HBV infection (a list of countries is available at http://wwwn.cdc.gov/travel/contentdiseases.aspx); and any adult seeking protection from HBV infection. Settings where hepatitis B vaccination is recommended for all adults: STD treatment facilities; HIV testing and treatment facilities; facilities providing drug-abuse treatment and prevention services; health-care settings targeting services to injection-drug users or men who have sex with men; correctional facilities; end-stage renal disease programs and facilities for chronic hemodialysis patients; and institutions and nonresidential day care facilities for persons with developmental disabilities. Special formulation indications: for adult patients receiving hemodialysis and other immunocompromised adults, 1 dose of 40 µg/mL (Recombivax HB®) or 2 doses of 20 µg/mL (Engerix-B®), administered simultaneously. 10. Meningococcal vaccination Medical indications: adults with anatomic or functional asplenia or terminal complement component deficiencies. Other indications: first-year college students living in dormitories; microbiologists who are routinely exposed to isolates of Neisseria meningitidis; military recruits; and persons who travel to or live in countries in which meningococcal disease is hyperendemic or epidemic (e.g., the "meningitis belt" of sub-Saharan Africa during the dry season [December--June]), particularly if their contact with local populations will be prolonged. Vaccination is required by the government of Saudi Arabia for all travelers to Mecca during the annual Hajj. Meningococcal conjugate vaccine is preferred for adults with any of the preceding indications who are aged <55 years, although meningococcal polysaccharide vaccine (MPSV4) is an acceptable alternative. Revaccination after 3--5 years might be indicated for adults previously vaccinated with MPSV4 who remain at increased risk for infection (e.g., persons residing in areas in which disease is epidemic). 11. Herpes zoster vaccination A single dose of zoster vaccine is recommended for adults aged >60 years regardless of whether they report a prior episode of herpes zoster. Persons with chronic medical conditions may be vaccinated unless a contraindication or precaution exists for their condition. 12. Selected conditions for which Haemophilus influenzae type b (Hib) vaccine may be used Hib conjugate vaccines are licensed for children aged 6 weeks--71 months. No efficacy data are available on which to base a recommendation concerning use of Hib vaccine for older children and adults with the chronic conditions associated with an increased risk for Hib disease. However, studies suggest good immunogenicity in patients who have sickle cell disease, leukemia, or HIV infection or who have had splenectomies; administering vaccine to these patients is not contraindicated. 13. Immunocompromising conditions Inactivated vaccines generally are acceptable (e.g., pneumococcal, meningococcal, and influenza [trivalent inactivated influenza vaccine]) and live vaccines generally are avoided in persons with immune deficiencies or immune suppressive conditions. Information on specific conditions is available at http://www.cdc.gov/vaccines/pubs/acip-list.htm. This schedule indicates the recommended age groups and medical indications for routine administration of currently licensed vaccines for persons aged >19 years, as of October 1, 2007. Licensed combination vaccines may be used whenever any components of the combination are indicated and when the vaccine's other components are not contraindicated. For detailed recommendations on all vaccines, including those used primarily for travelers or those issued during the year, consult the manufacturers' package inserts and the complete statements from the Advisory Committee on Immunization Practices (available at http://www.cdc.gov/vaccines/pubs/acip-list.htm). Report all clinically significant postvaccination reactions to the Vaccine Adverse Event Reporting System (VAERS). Reporting forms and instructions on filing a VAERS report are available at http://www.vaers.hhs.gov or by telephone, 800-822-7967. Information on how to file a Vaccine Injury Compensation Program claim is available at http://www.hrsa.gov/vaccinecompensation or by telephone, 800-338-2382. To file a claim for vaccine injury, contact the U.S. Court of Federal Claims, 717 Madison Place, N.W., Washington, D.C. 20005; telephone, 202-357-6400. Use of trade names and commercial sources is for identification only and does not imply endorsement by the U.S. Department of Health and Human Services.
Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Date last reviewed: 10/18/2007 |
|||||||||
|